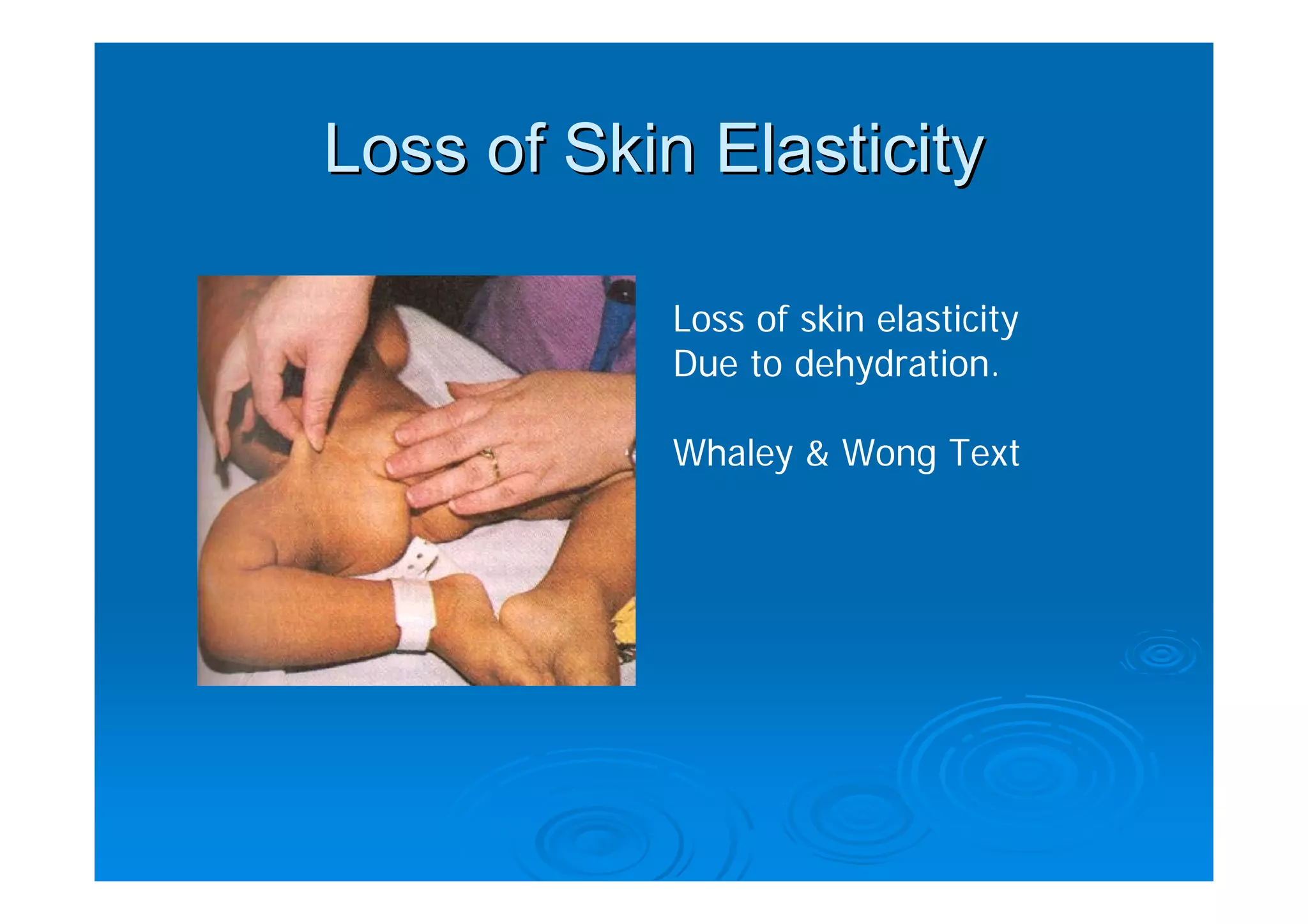
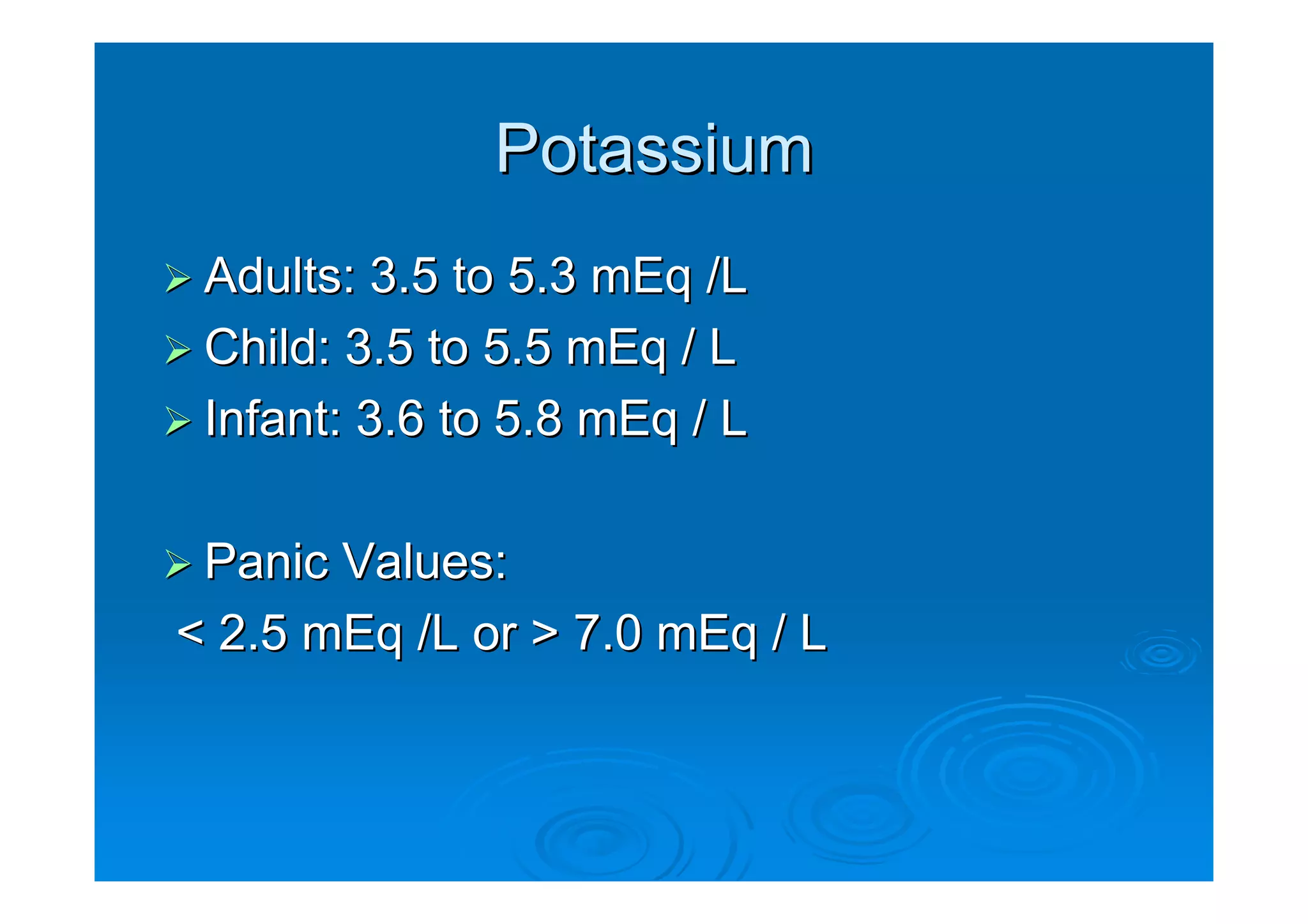
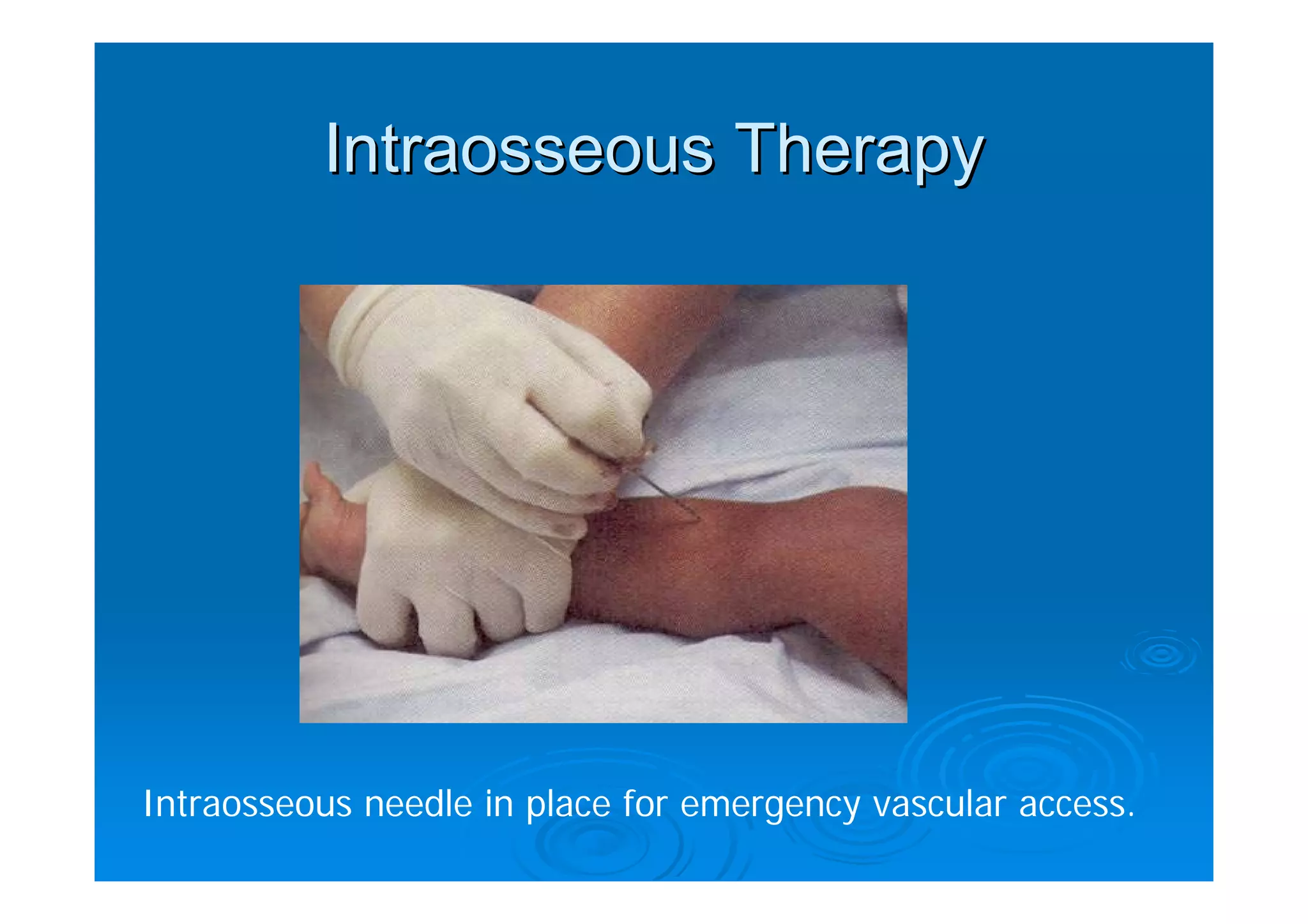
This document discusses fluid and electrolyte balance in infants and children. It covers normal fluid regulation, increased and decreased fluid needs, signs of dehydration and fluid overload, diagnostic tests including electrolyte levels, treatment for dehydration including oral and IV rehydration, and acid-base imbalances including causes and management of respiratory and metabolic acidosis and alkalosis.