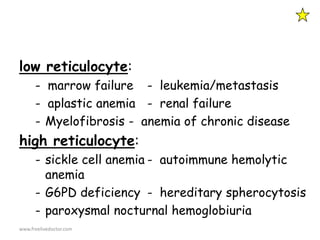
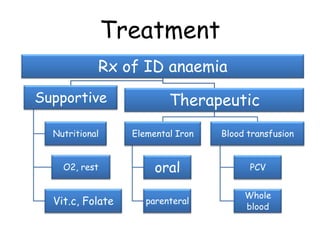
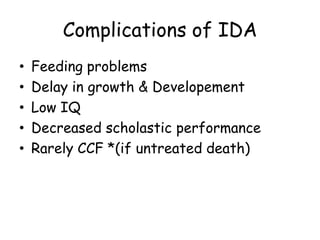
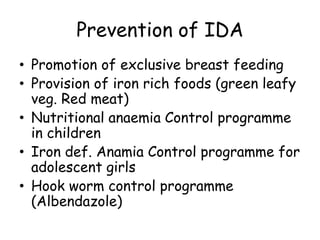
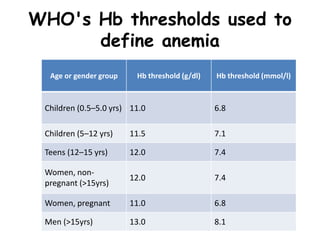
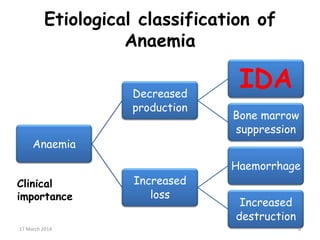
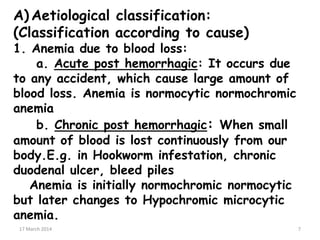
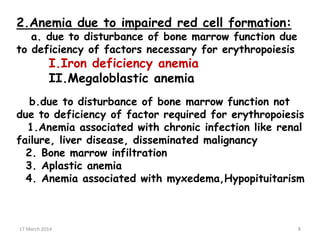
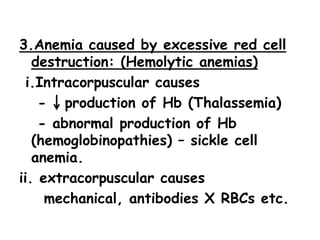
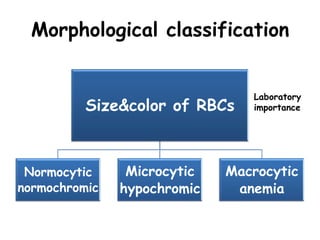
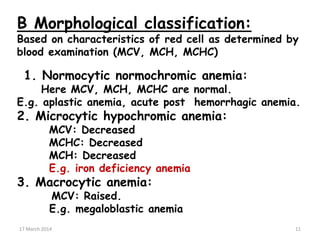
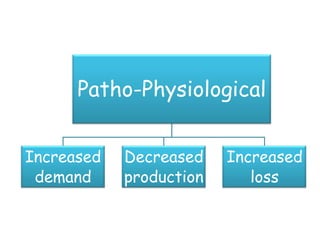
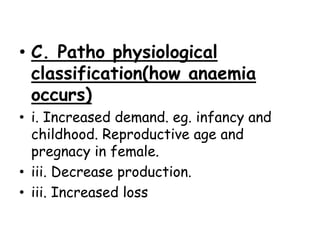
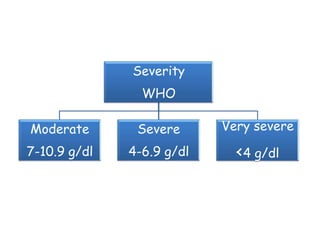
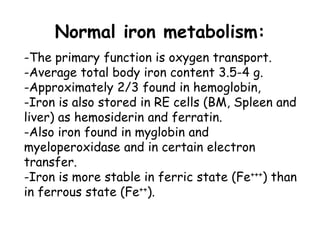
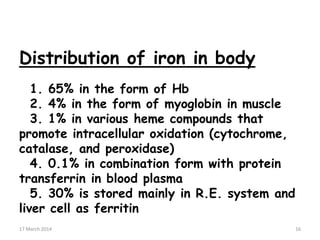
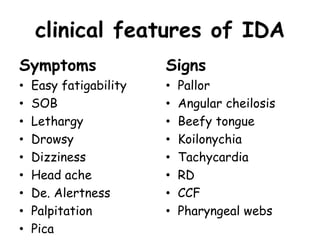
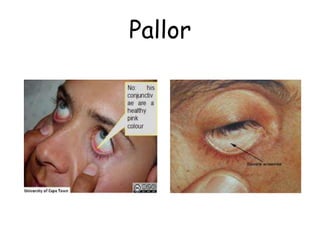
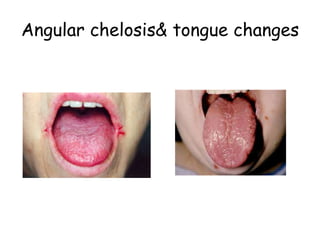
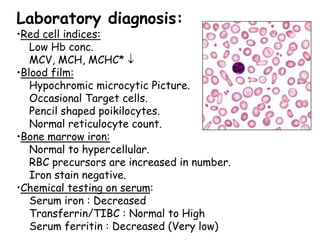
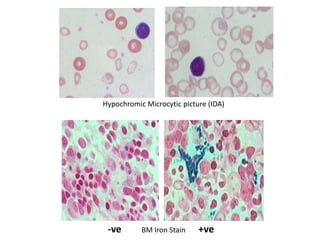
This document discusses iron deficiency anemia (IDA) in children. It begins by defining anemia and listing the WHO thresholds used to define anemia in different age groups. It then covers the etiological, morphological and pathophysiological classifications of anemia. Under the etiological classification, it describes anemias caused by blood loss, impaired red blood cell formation, and excessive red blood cell destruction. It also discusses the clinical features, laboratory diagnosis, treatment, complications and prevention of IDA in children.



![Labo. Approach (work-up)
M: Hb <13.5 Hct <41
F:Hb <12 Hct <36 : Child ; Hb <11
[check MCV]
MCV <80 = microcytic
• Fe deficiency
• thalassemia
• anemia of chronic disease
• sideroblastic anemia
www.freelivedoctor.com](https://image.slidesharecdn.com/anaemiainchildren-140317063654-phpapp02/85/Anaemia-in-children-27-320.jpg)
![MCV >100 = macrocytic
• megaloblastic anemia
• VitB12 deficiency
• folate deficiency
• alcoholic liver disease
MCV 80-100 = normocytic
[chech reticulocyte count]
www.freelivedoctor.com](https://image.slidesharecdn.com/anaemiainchildren-140317063654-phpapp02/85/Anaemia-in-children-28-320.jpg)