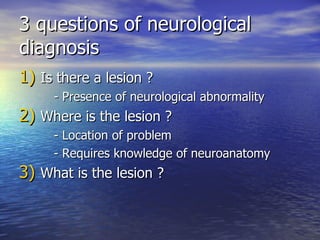
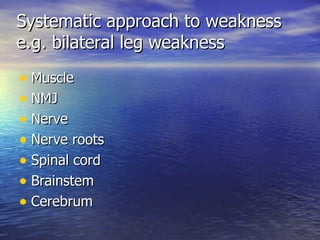
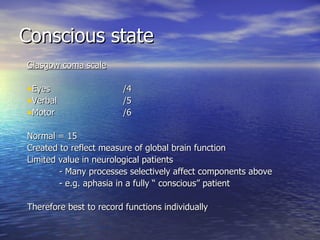
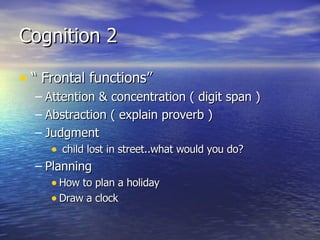
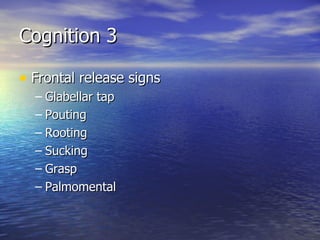
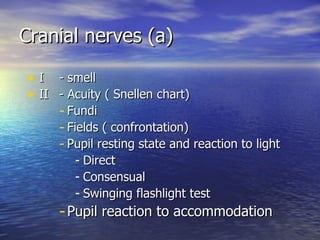
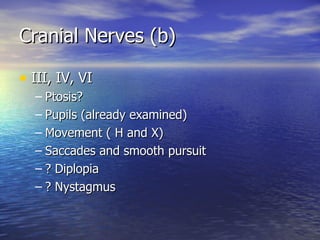
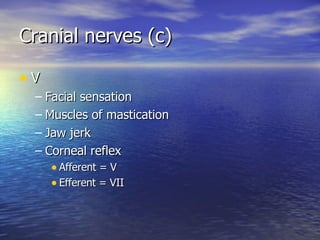
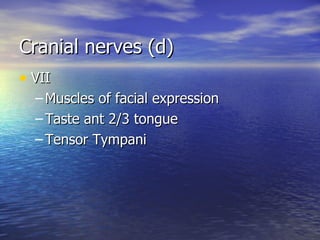
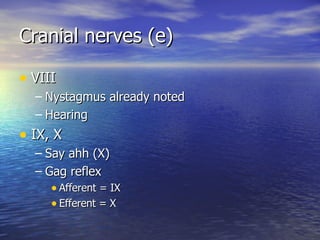
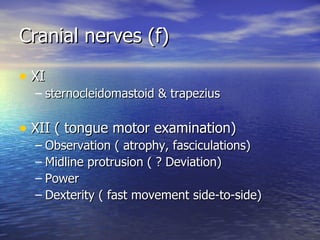
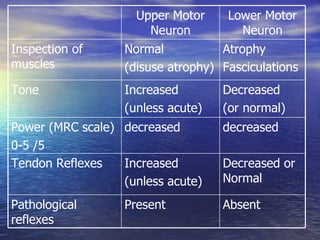
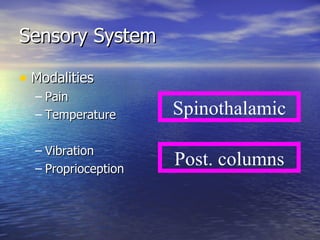
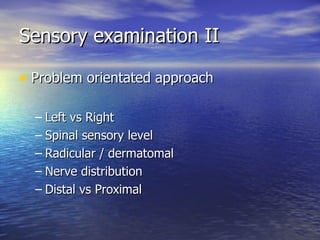
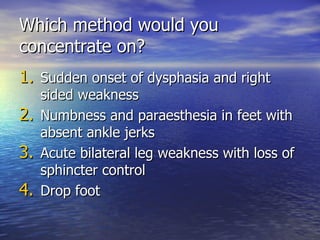
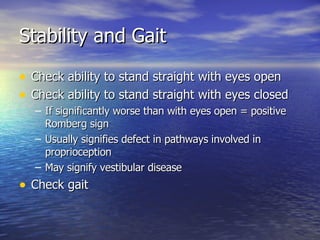
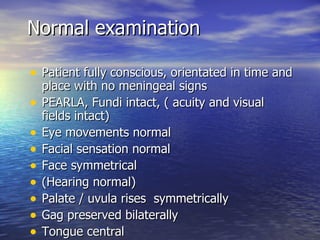
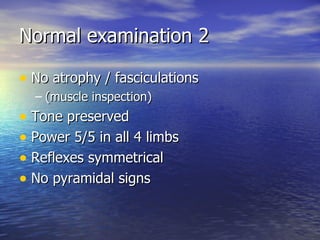
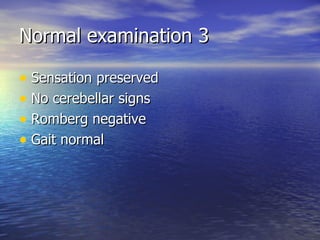
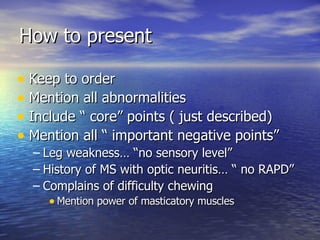
The document provides guidance on performing a neurological examination to systematically evaluate patients for neurological abnormalities. It discusses evaluating the patient's conscious state, cognition, cranial nerves, motor system, sensory system, and extrapyramidal signs. The examination aims to detect any neurological abnormalities, localize them within the nervous system, and determine the specific lesion.