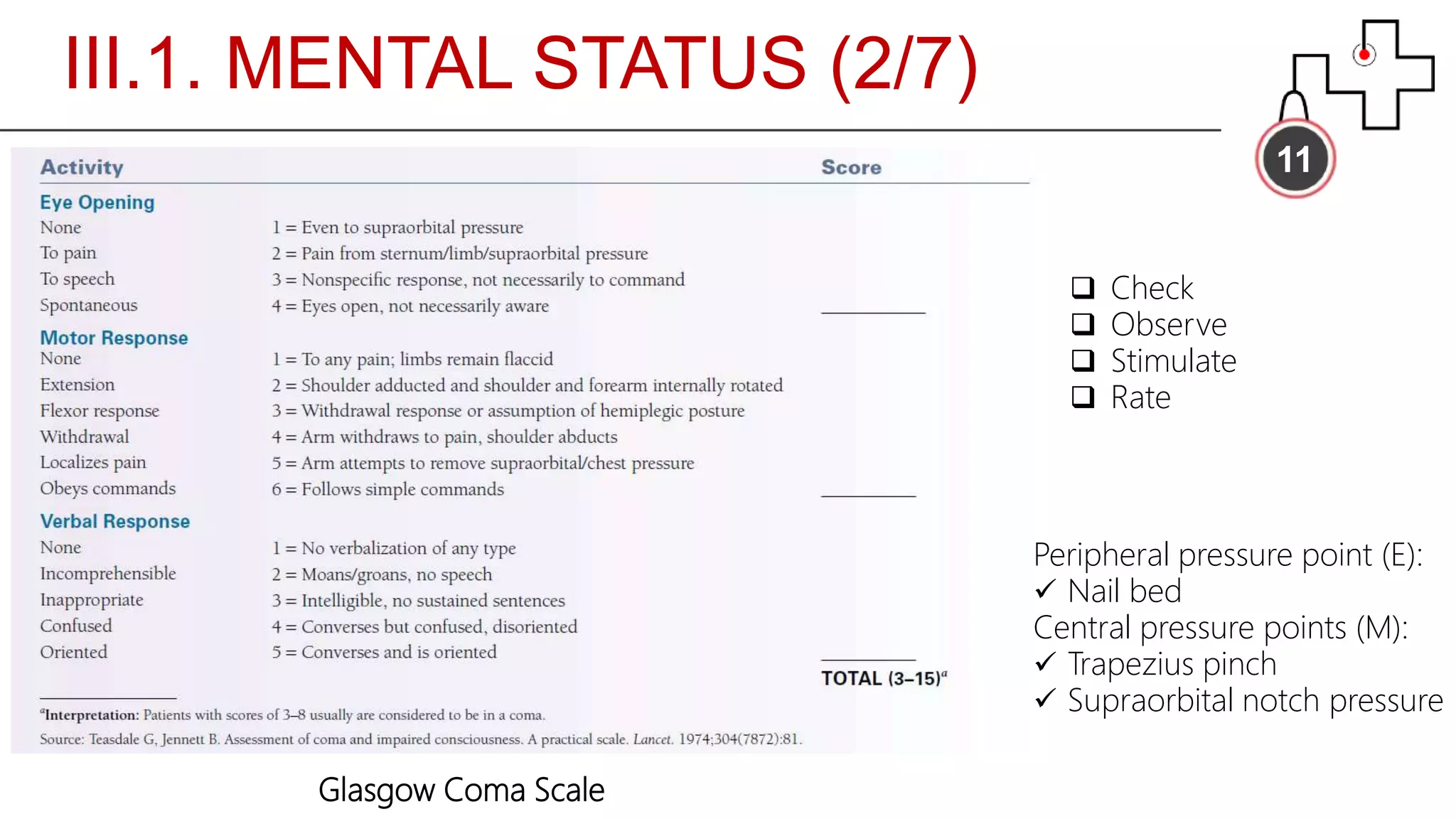
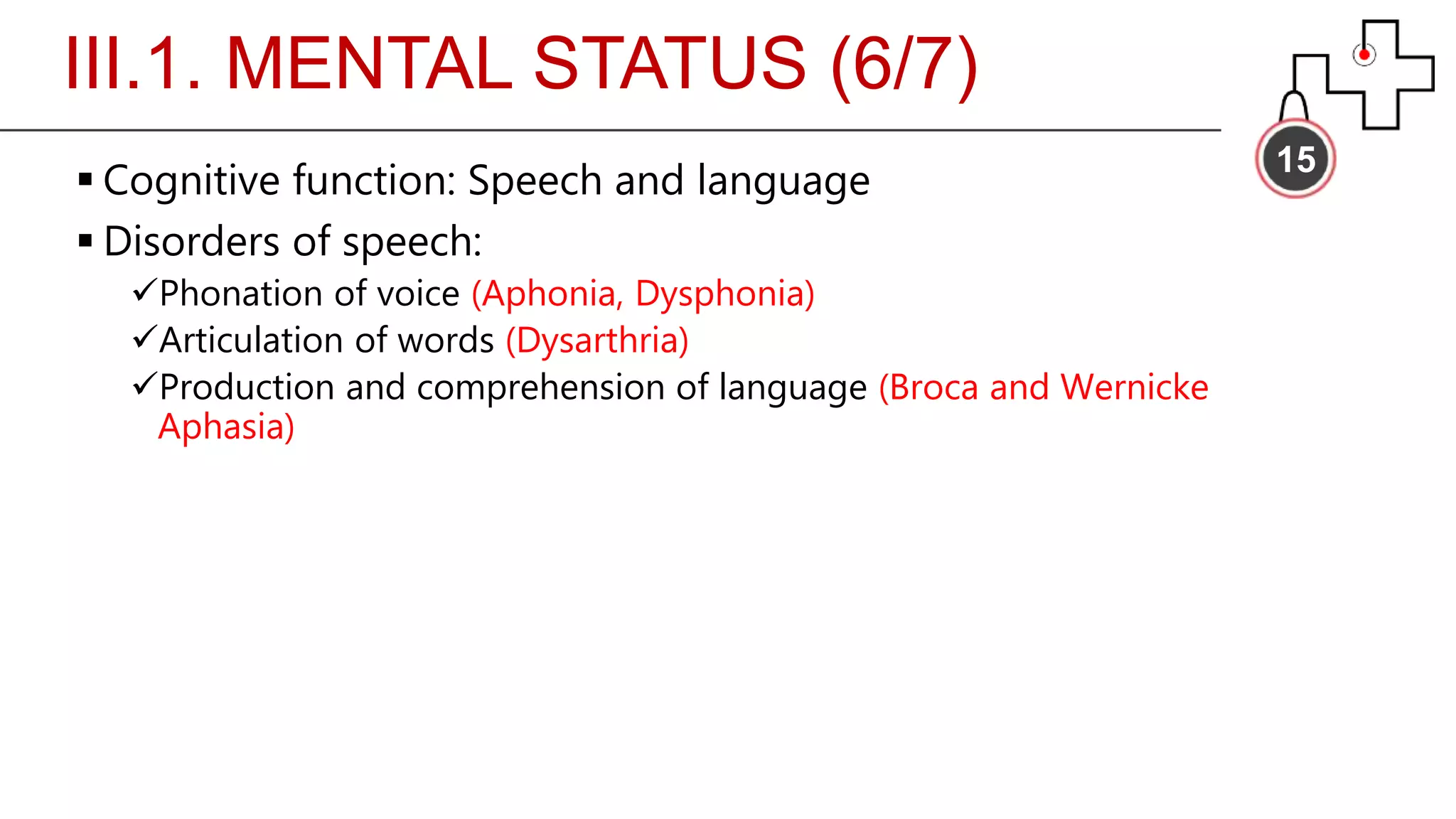
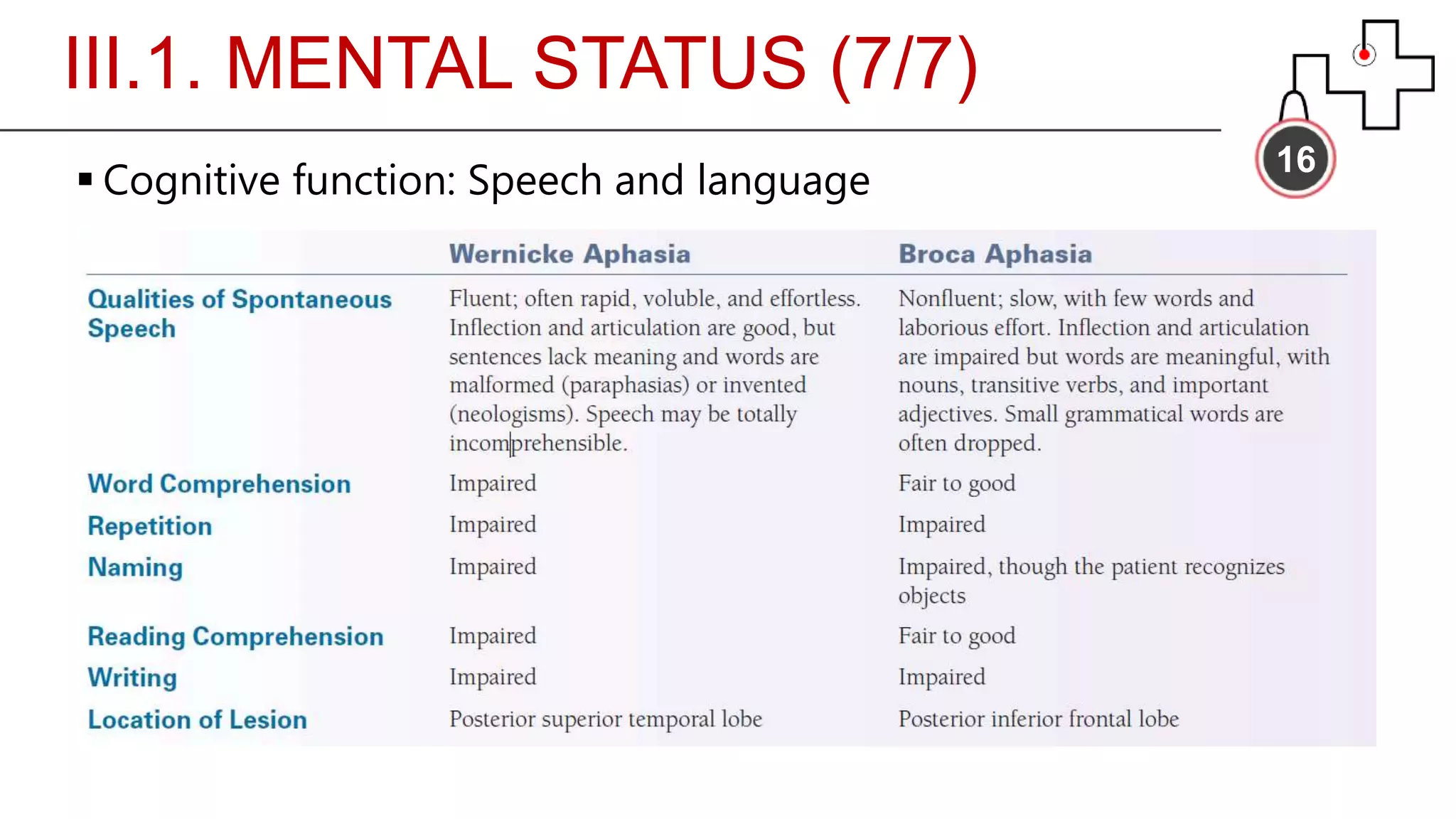
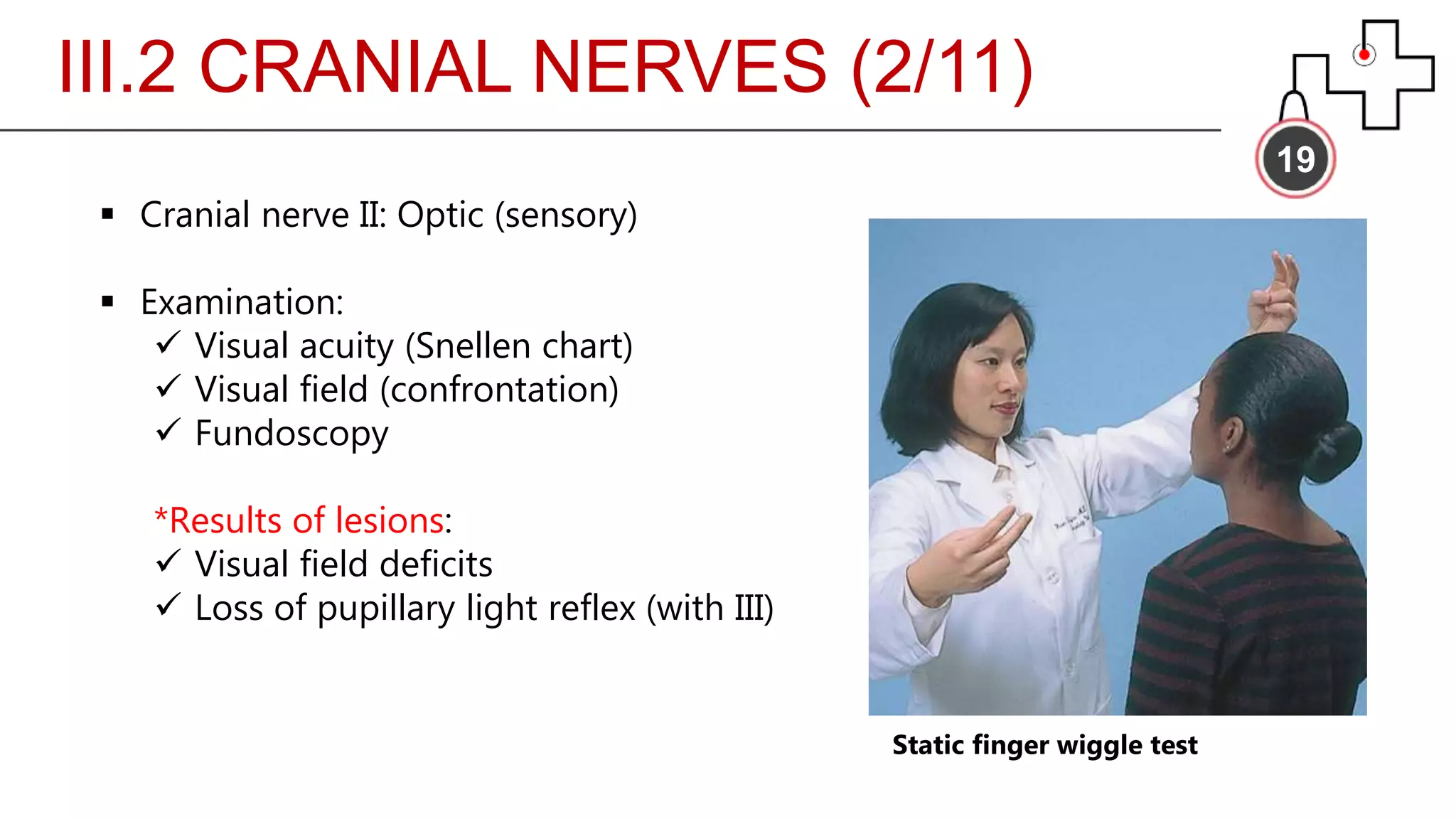
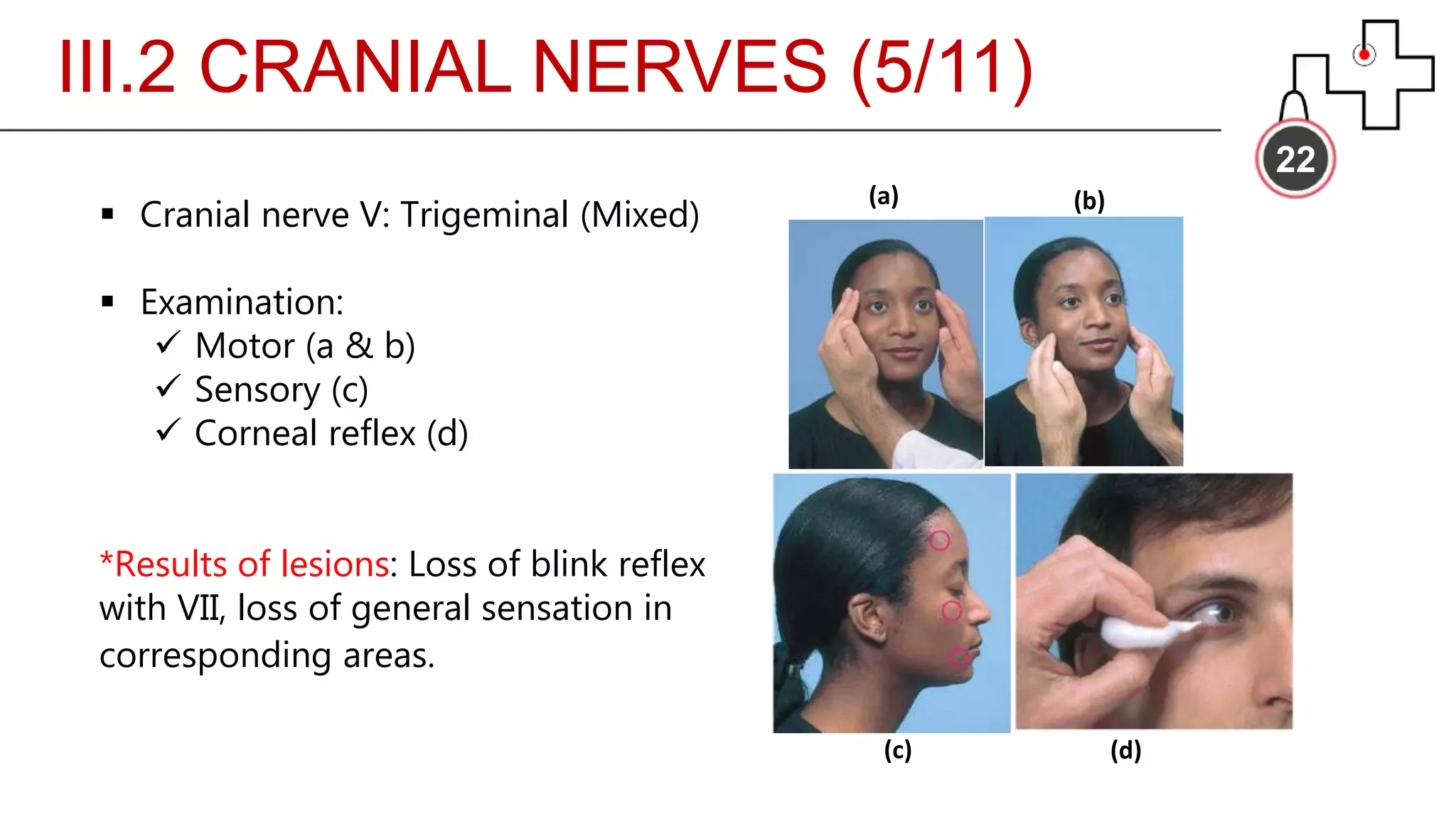
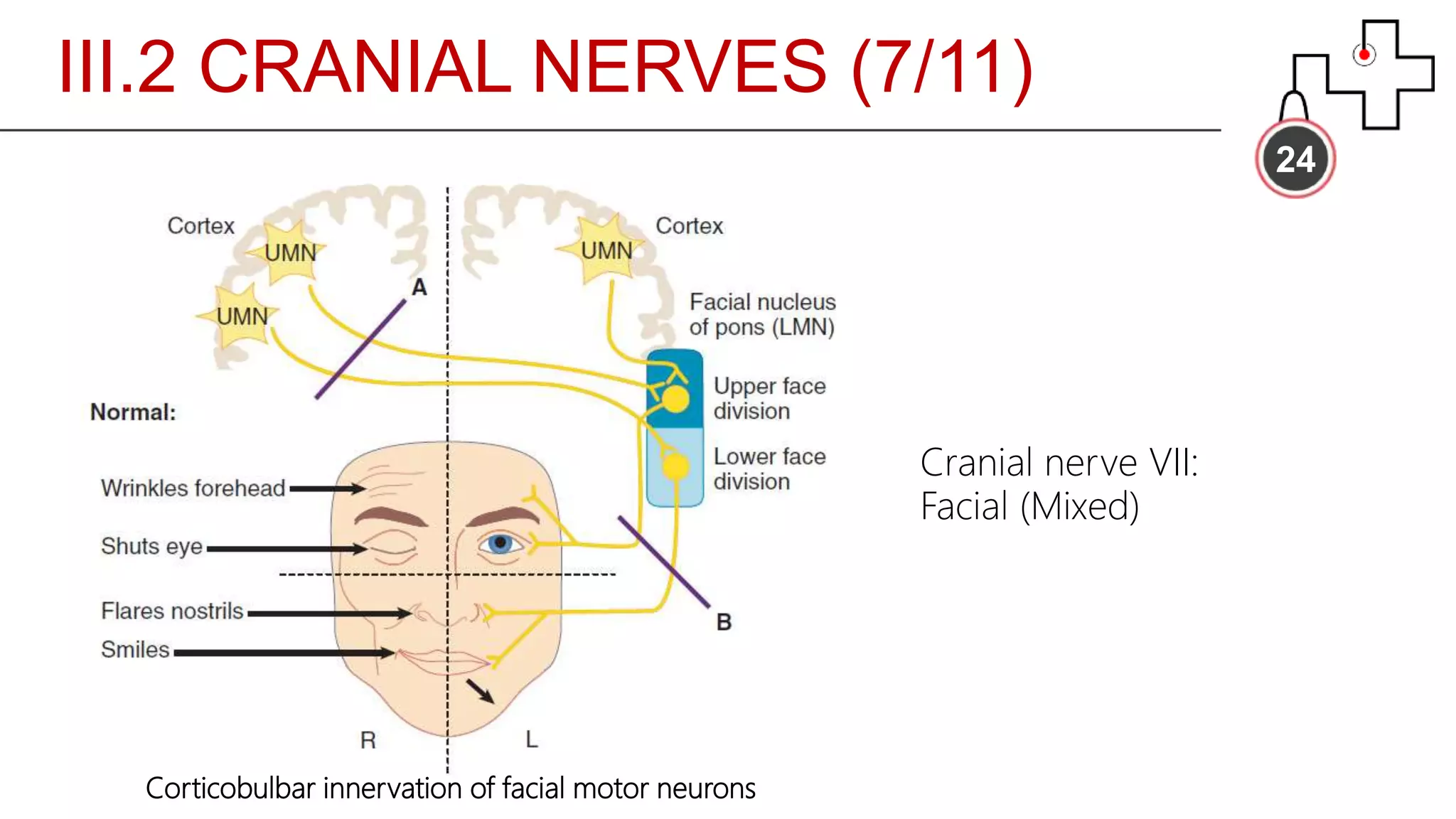
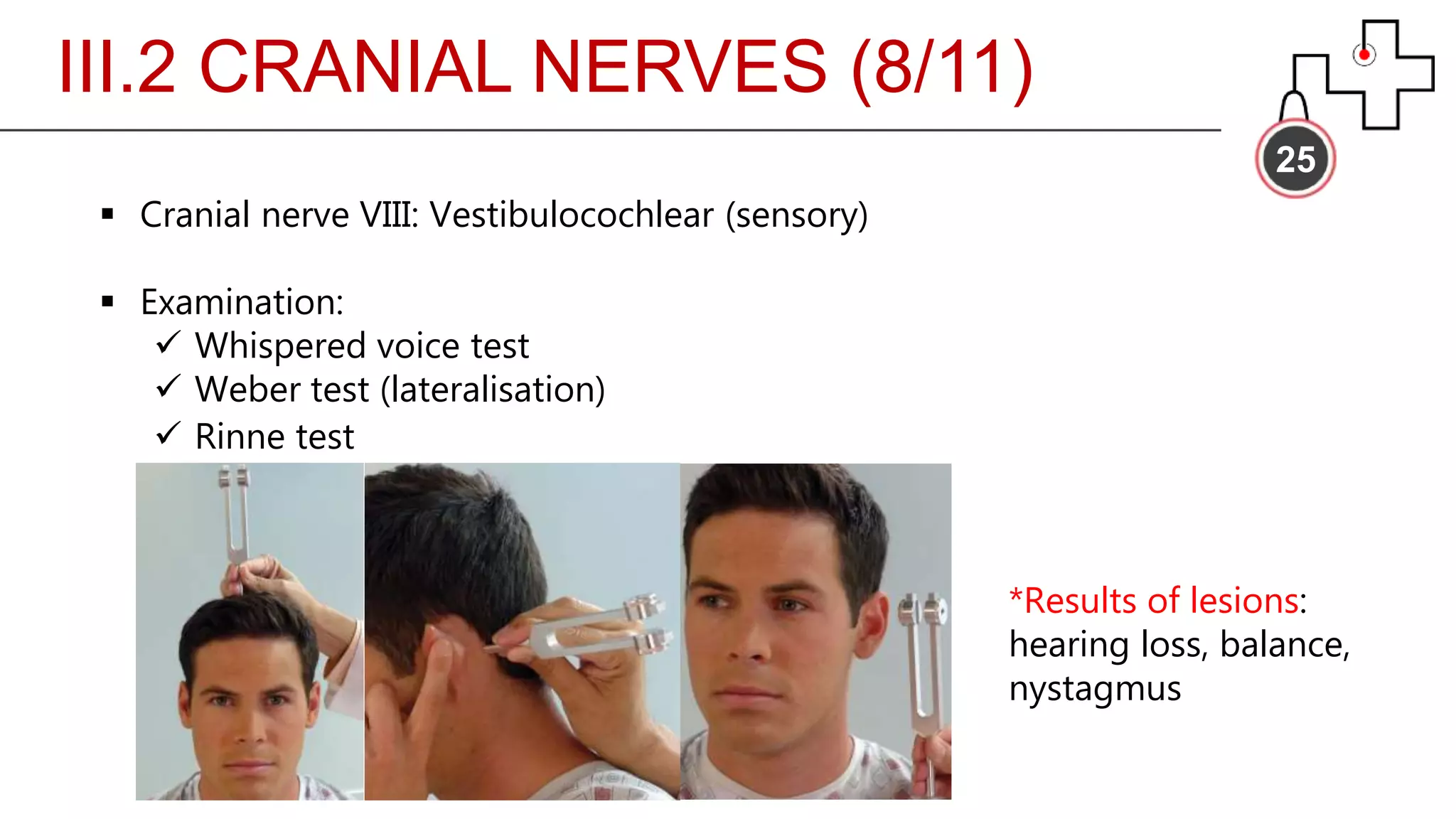
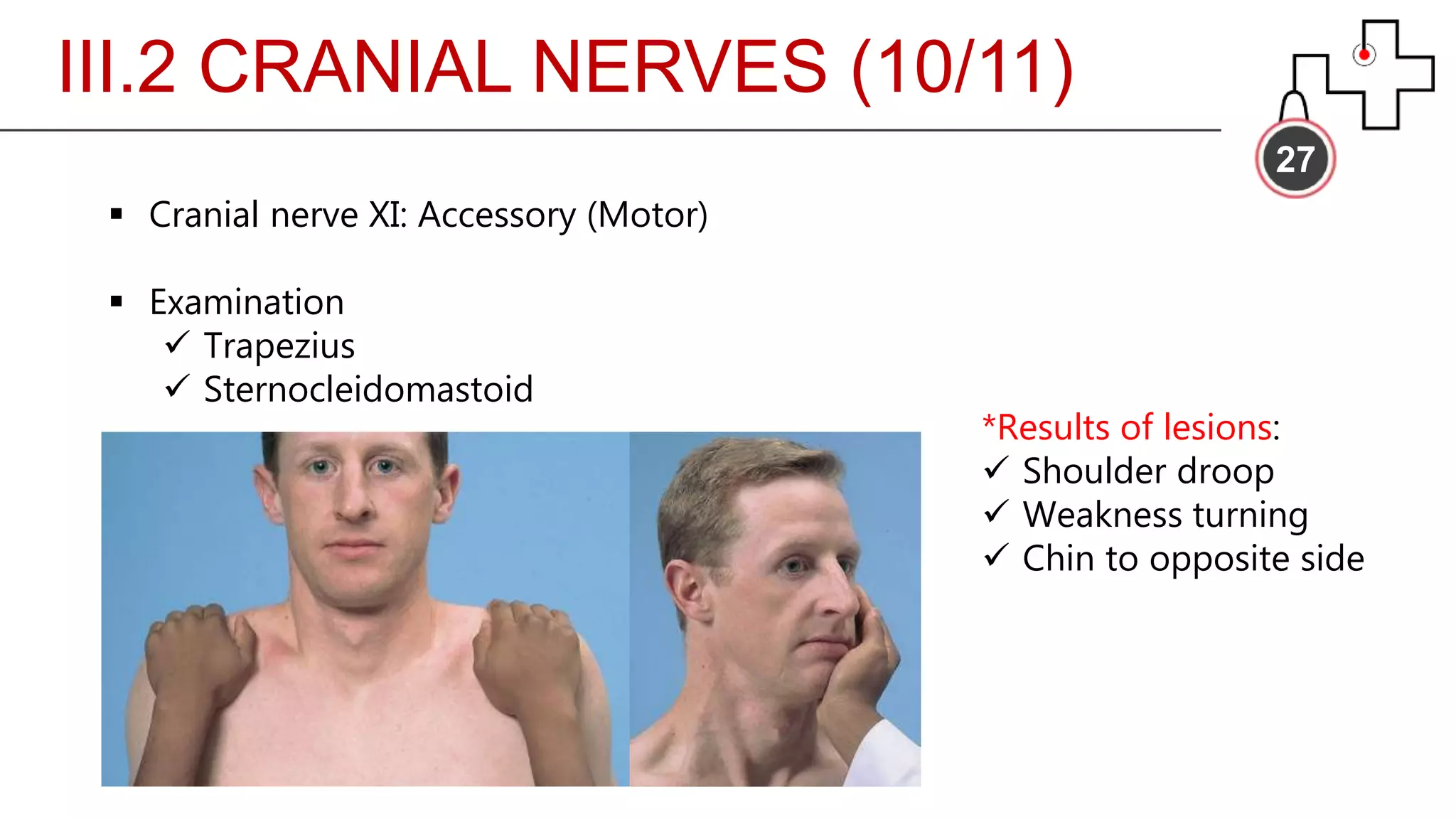
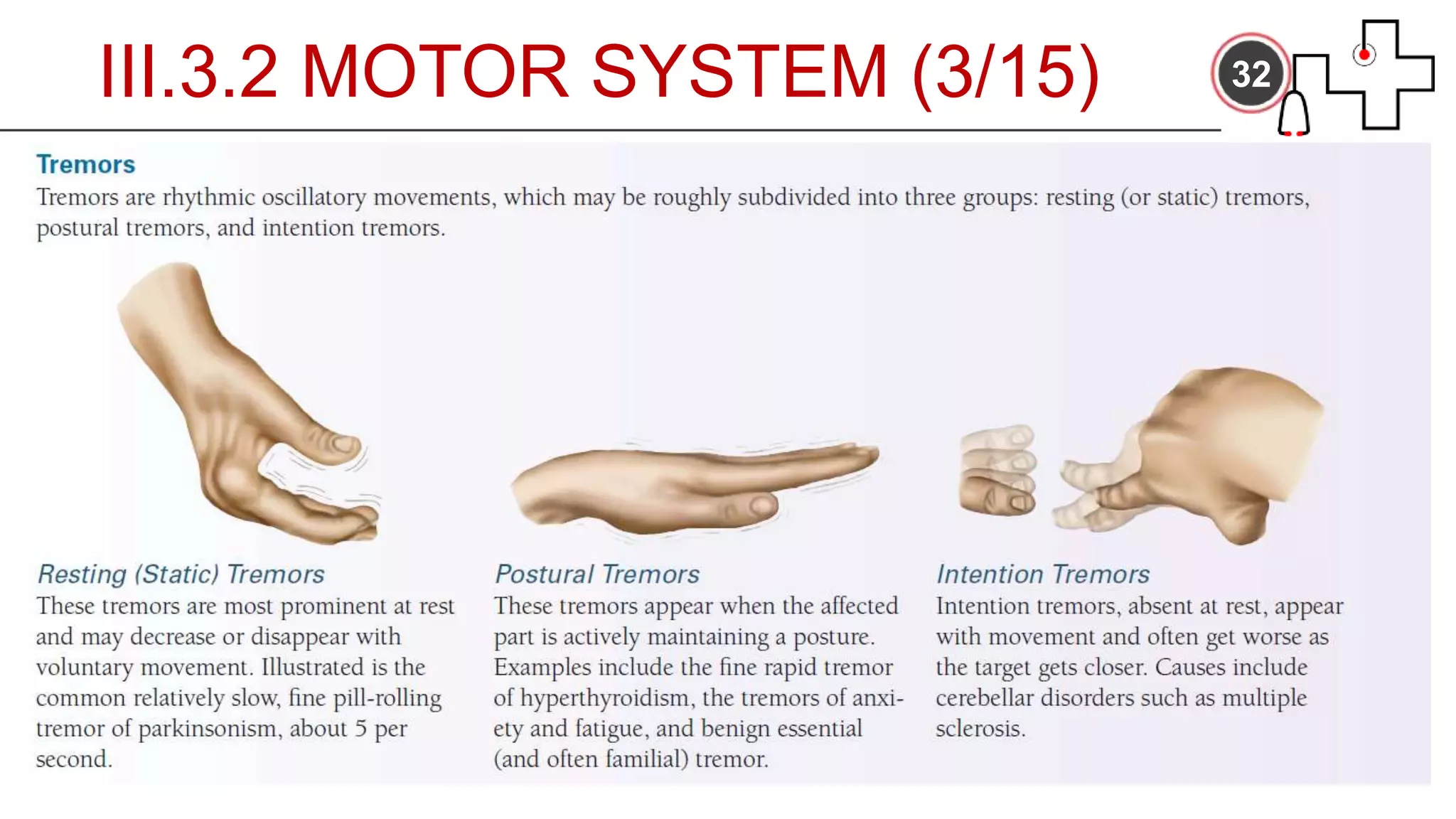
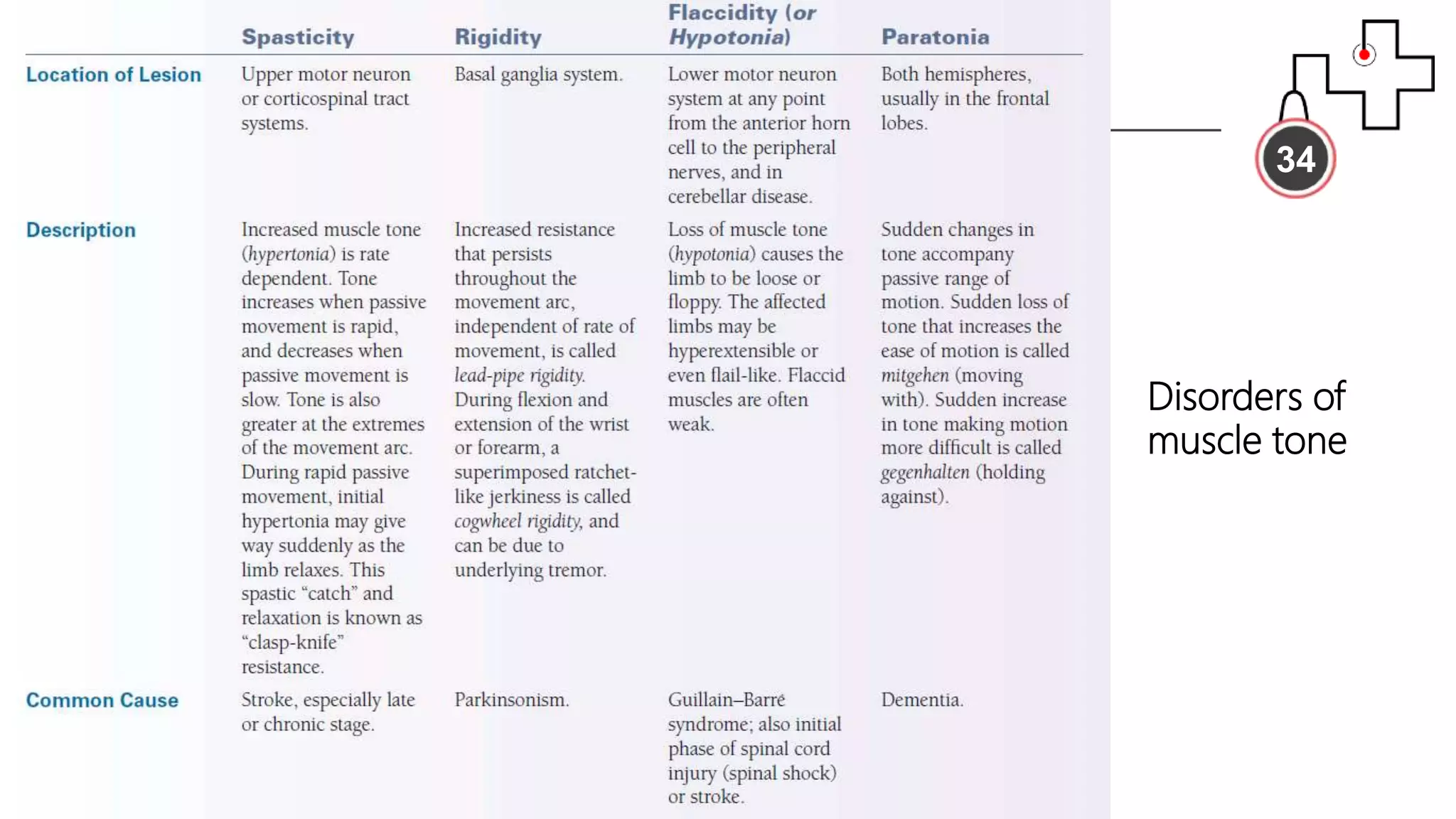
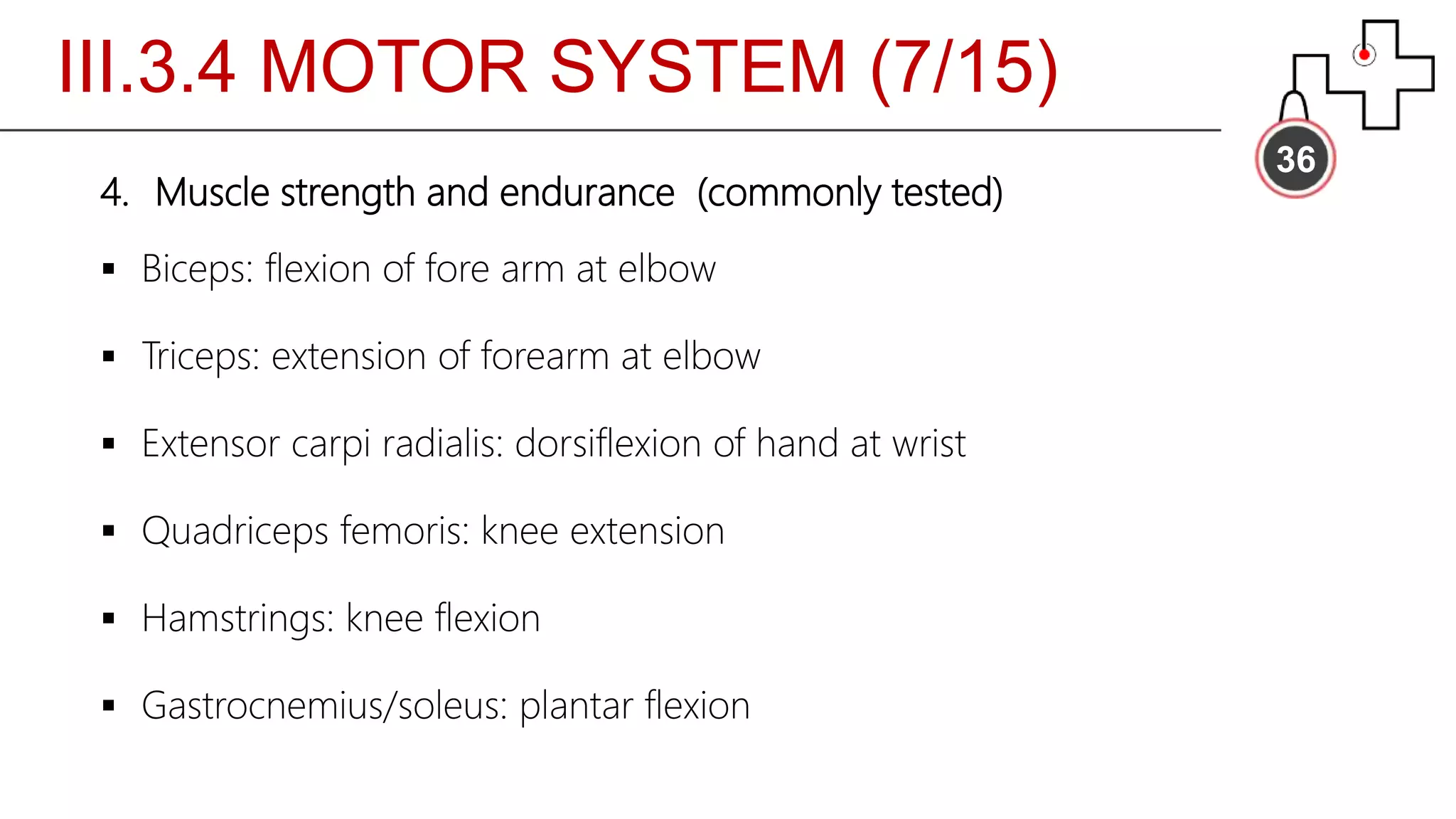
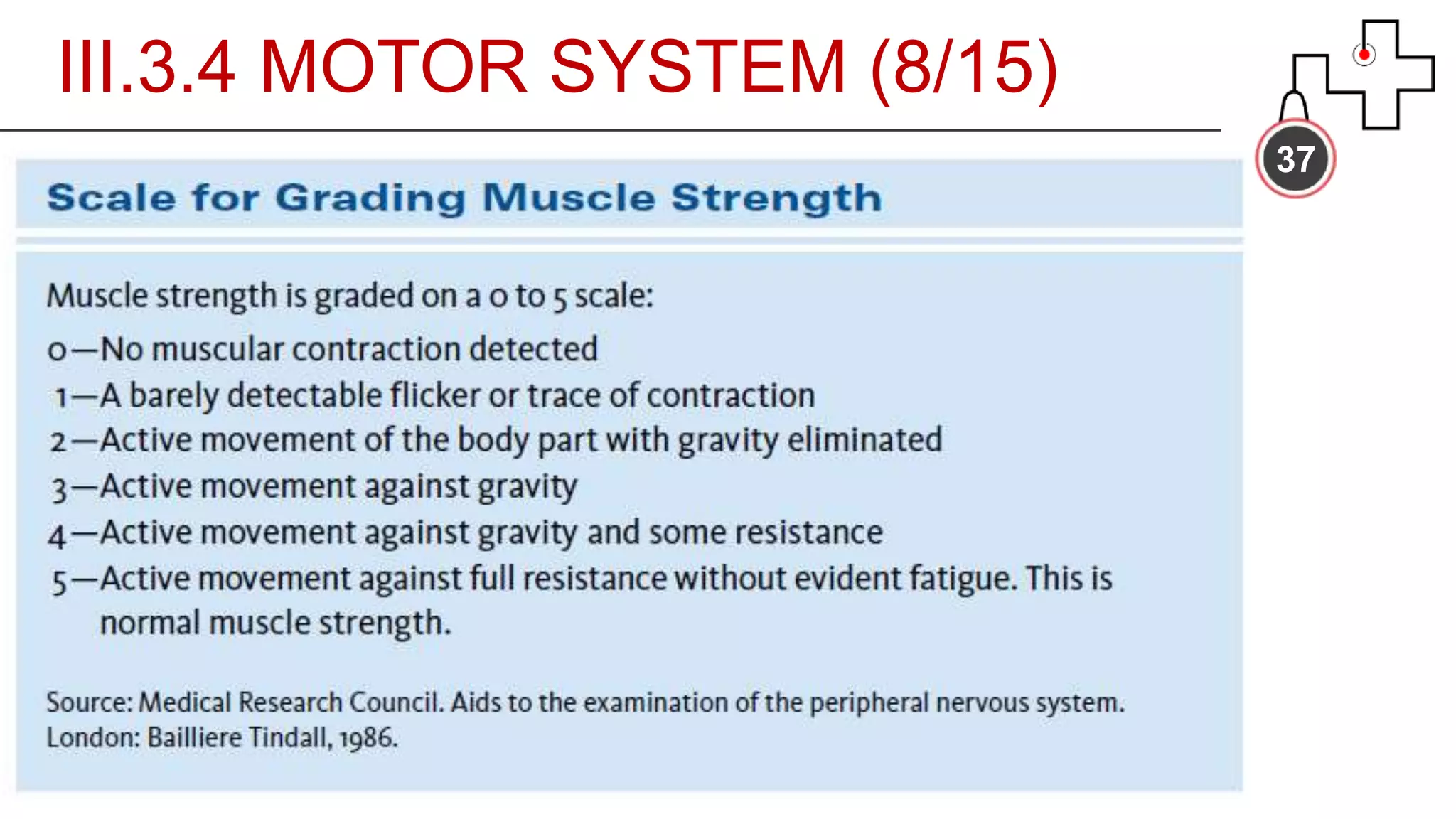
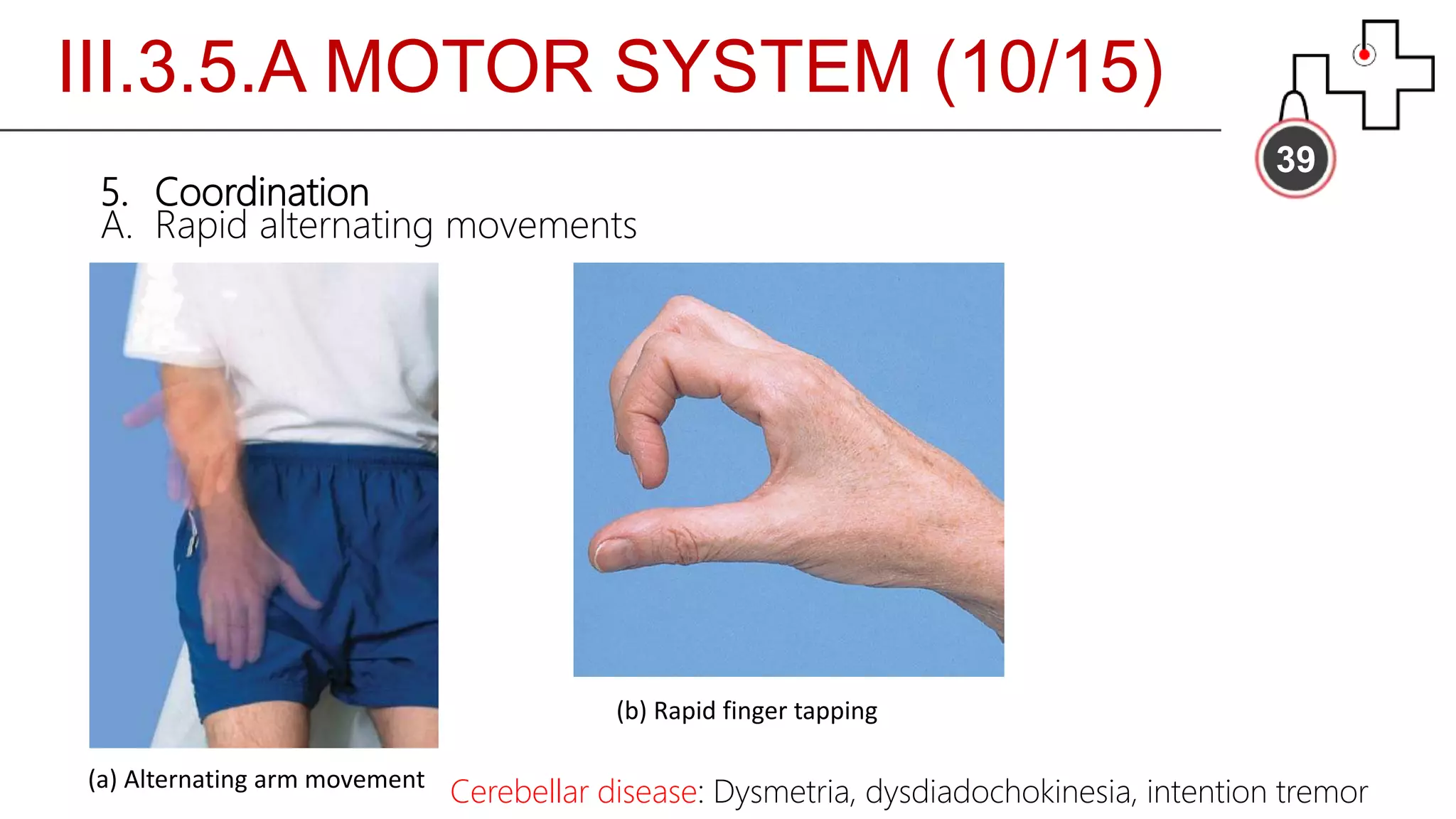
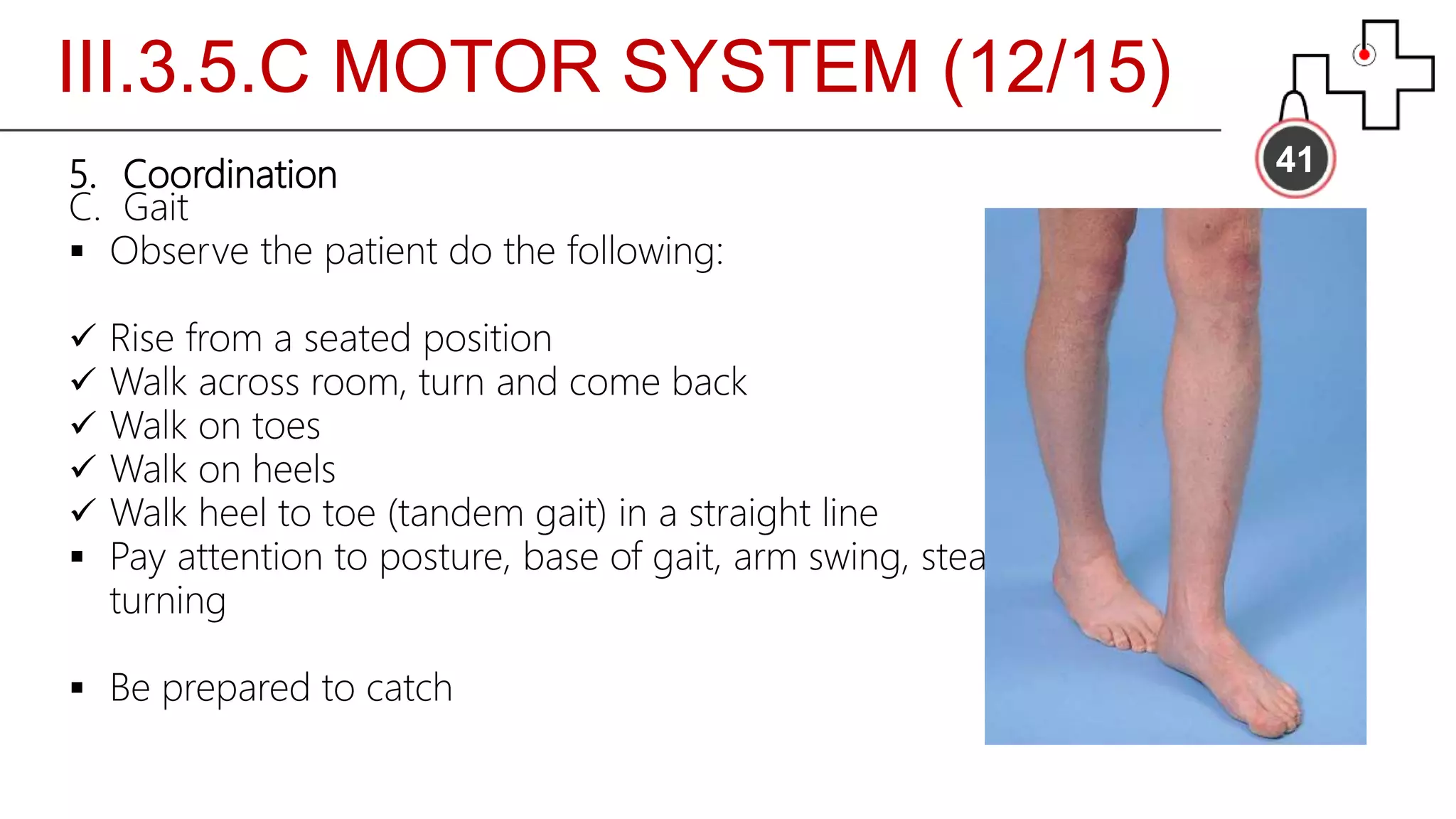
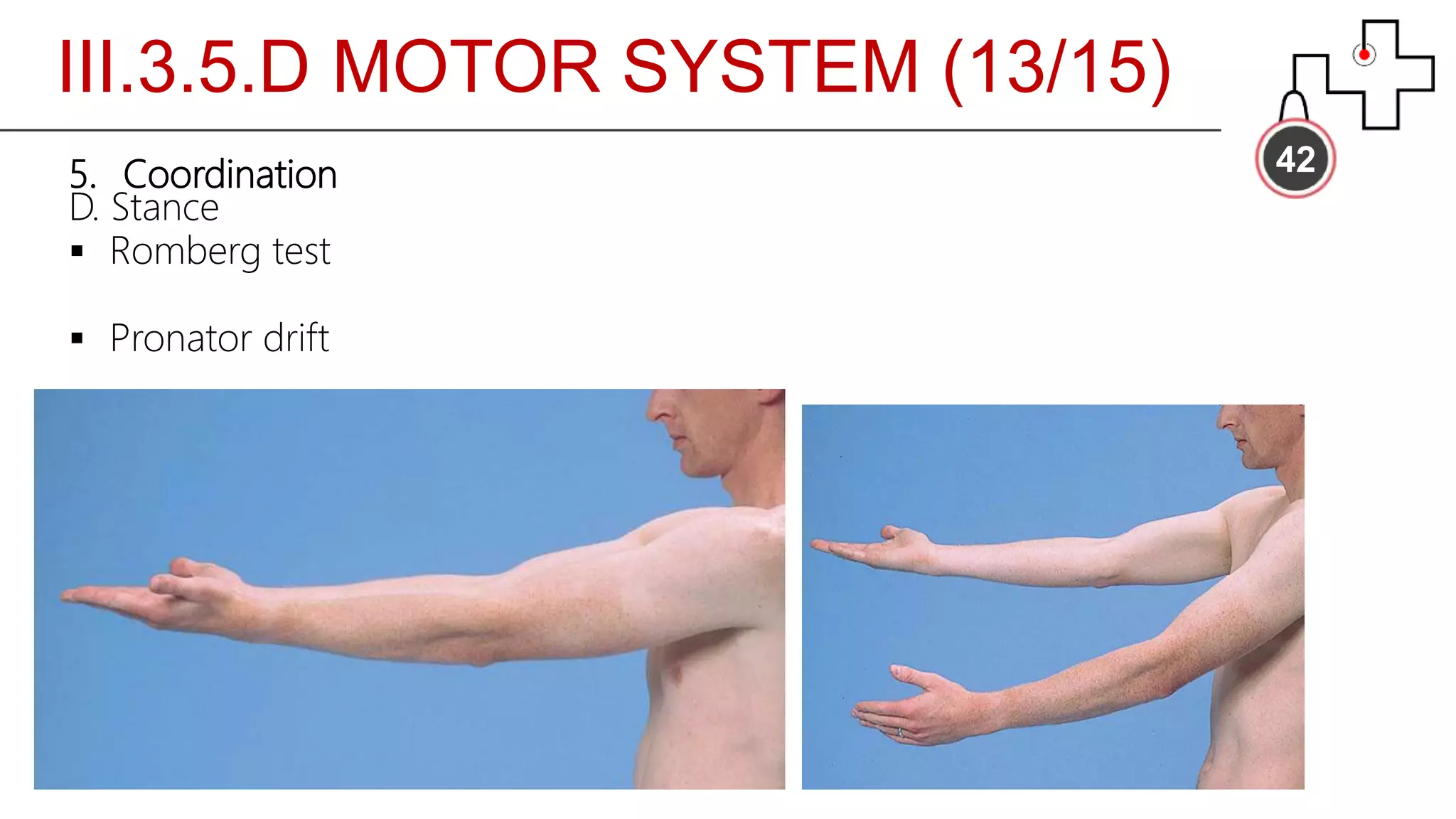
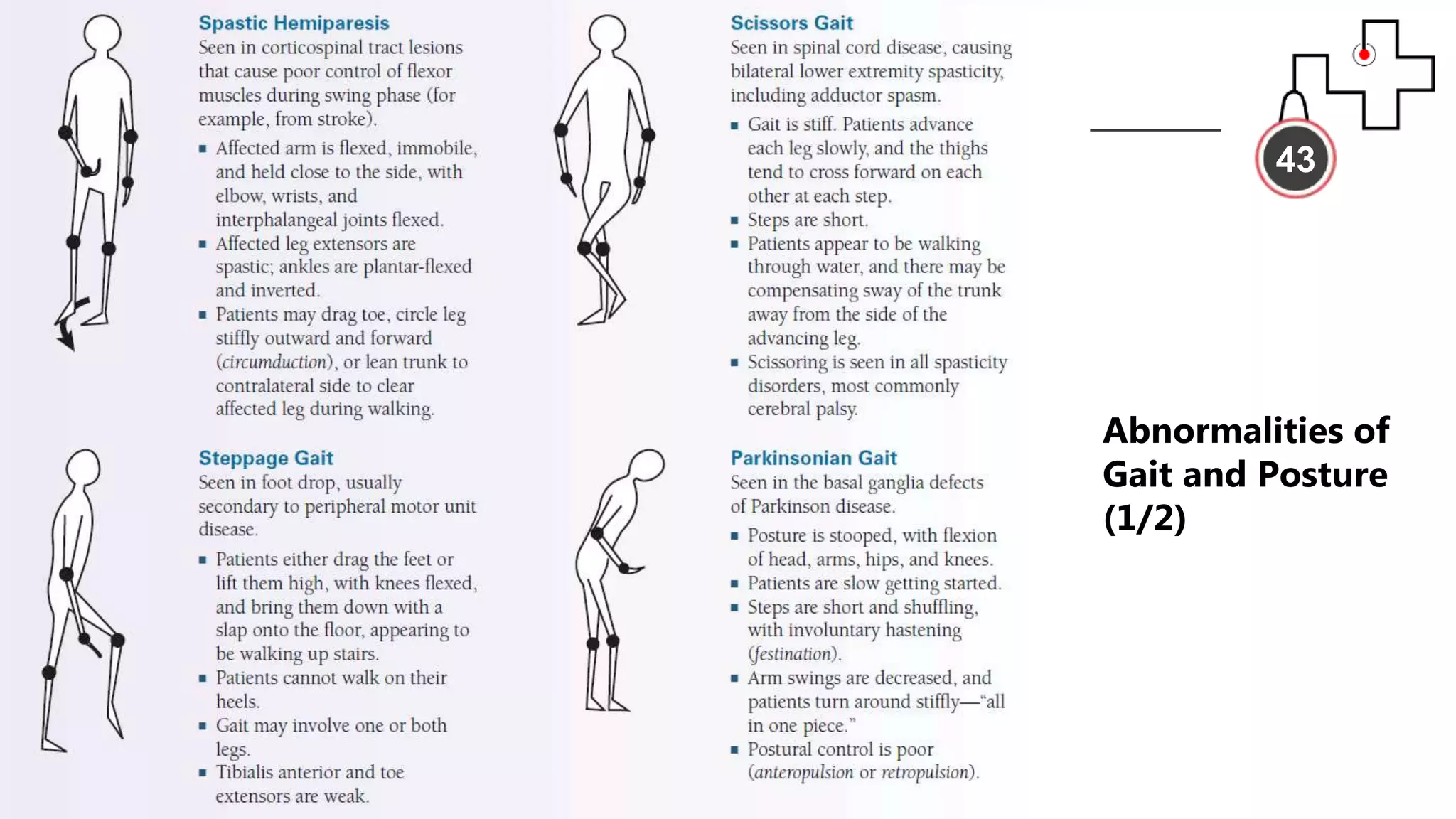
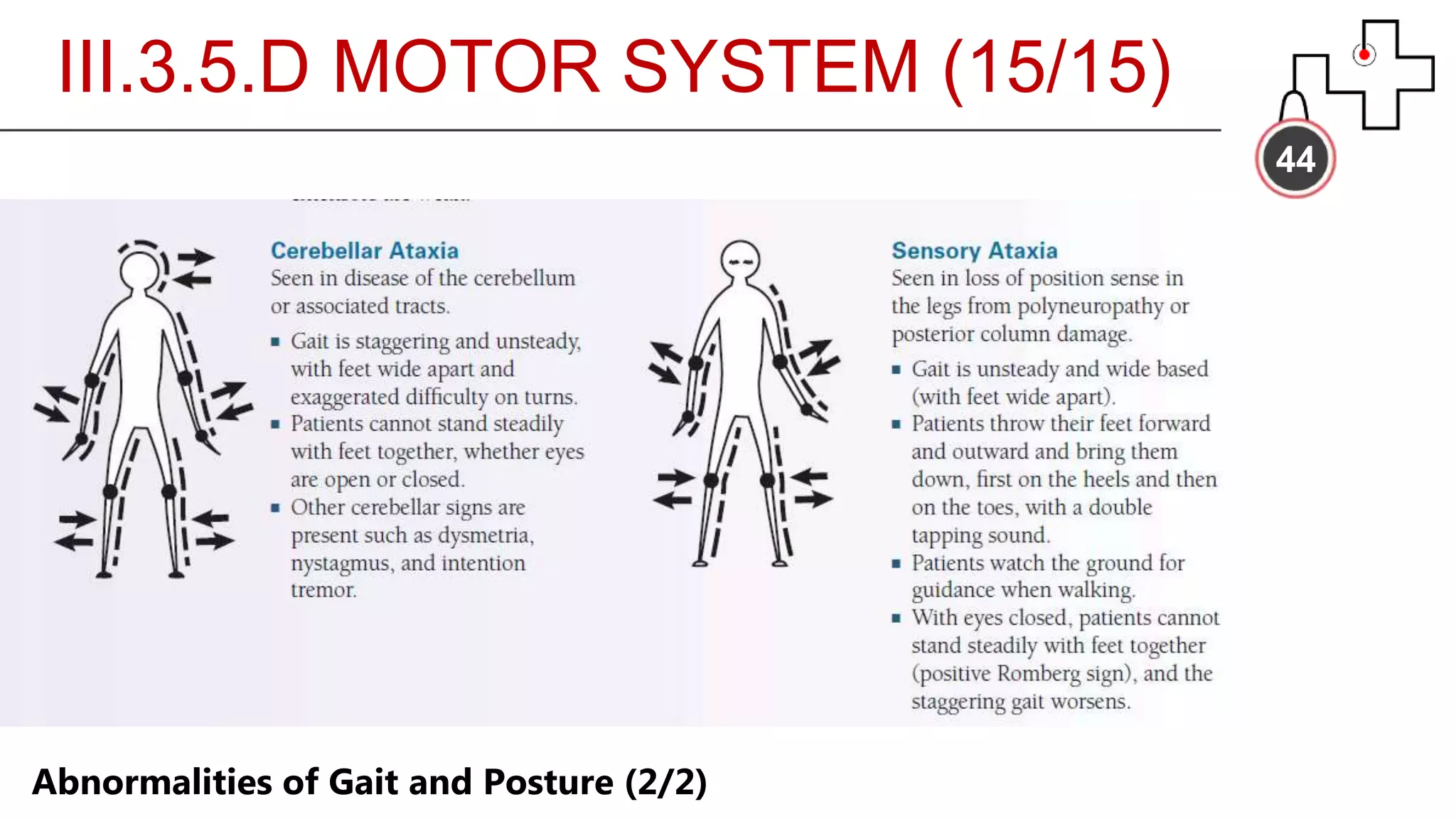
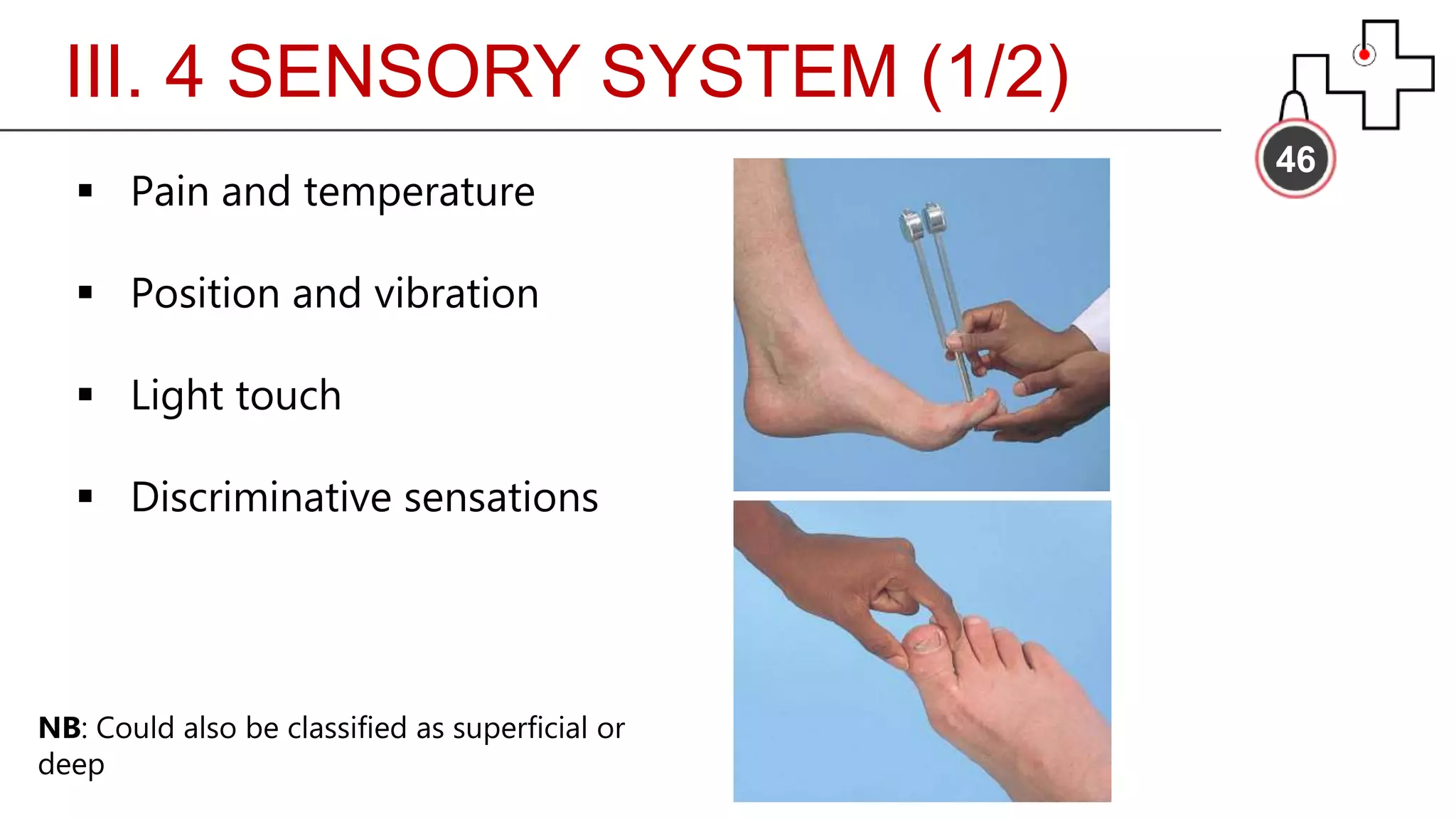
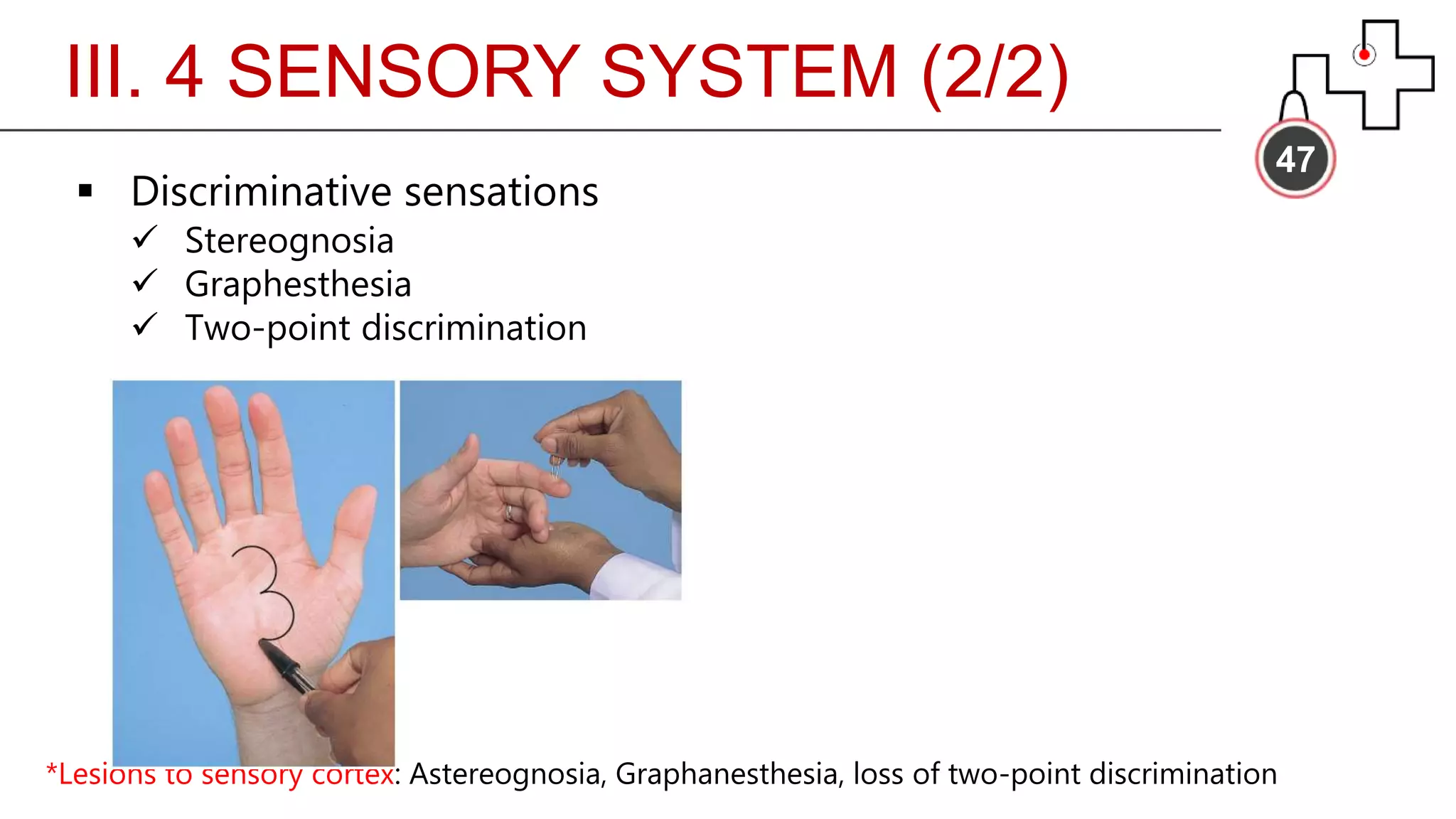
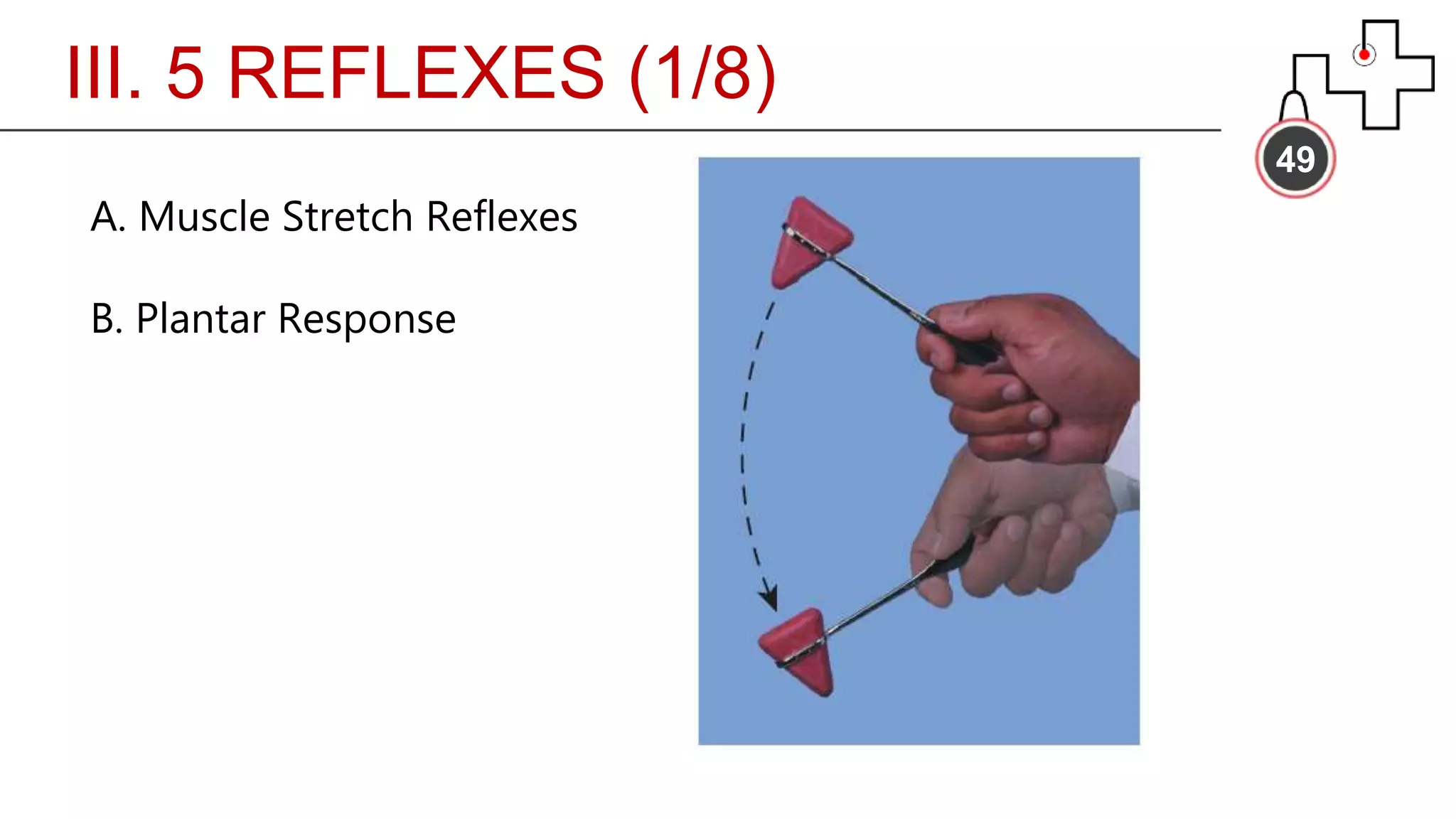
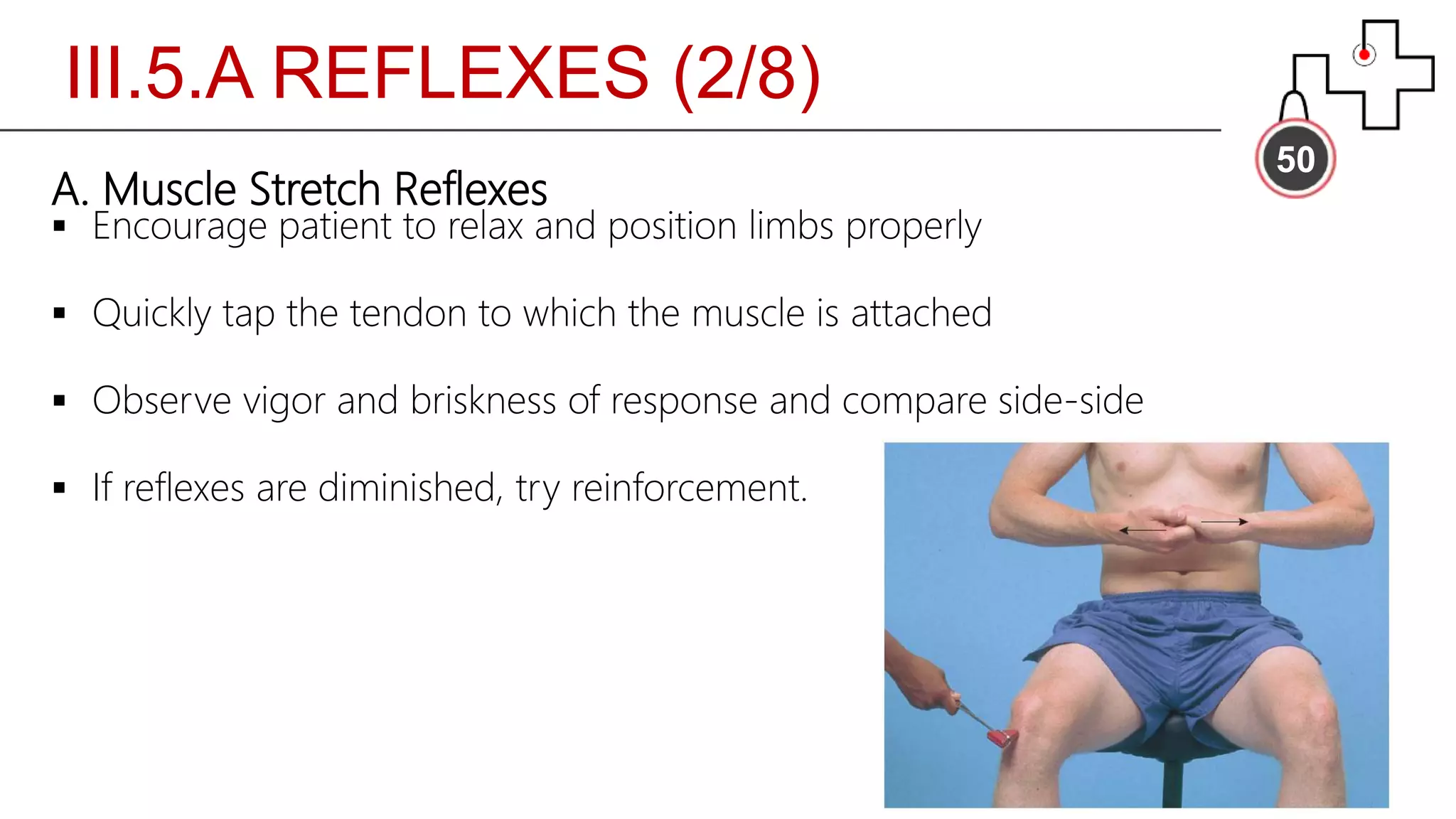
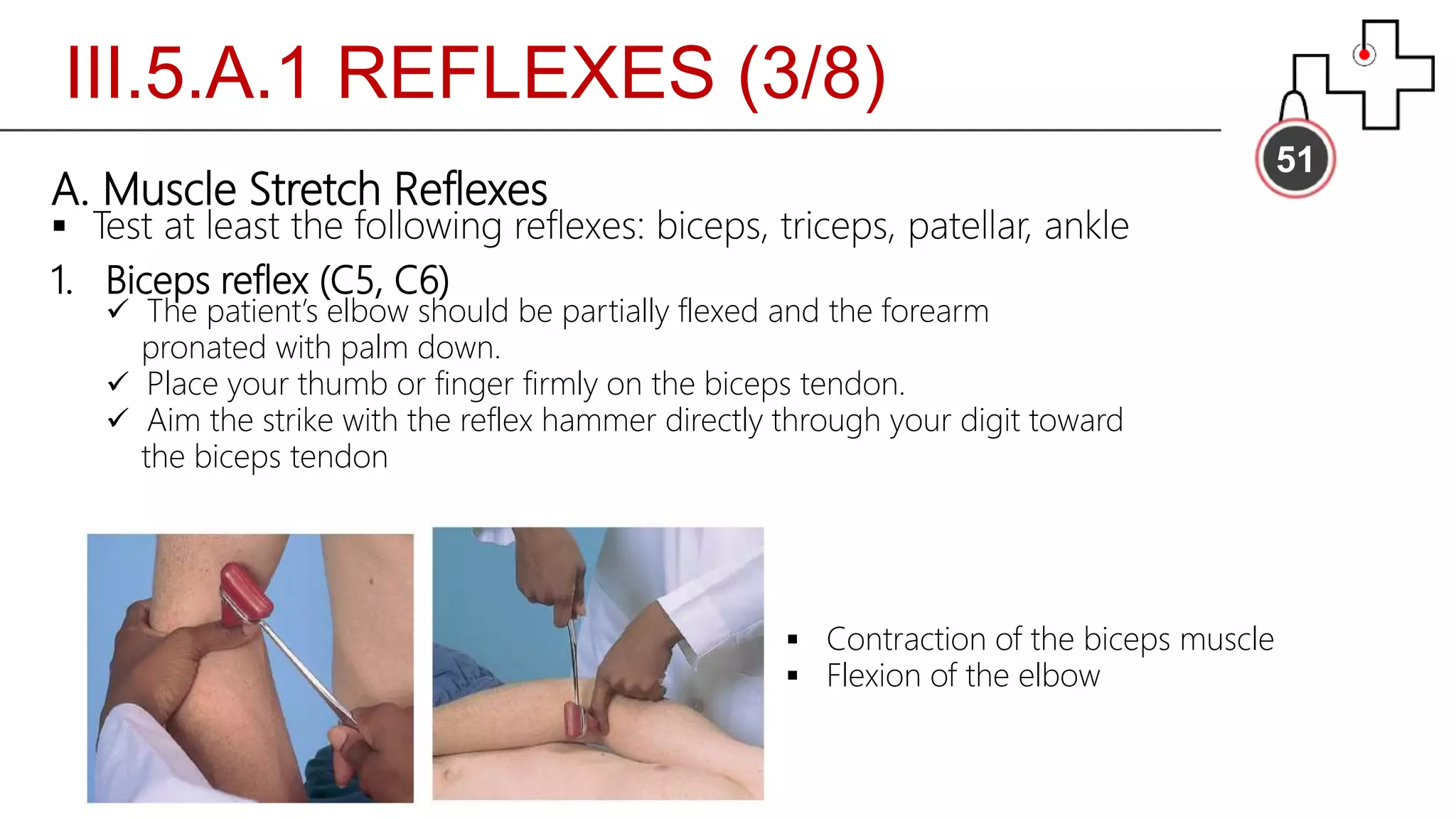
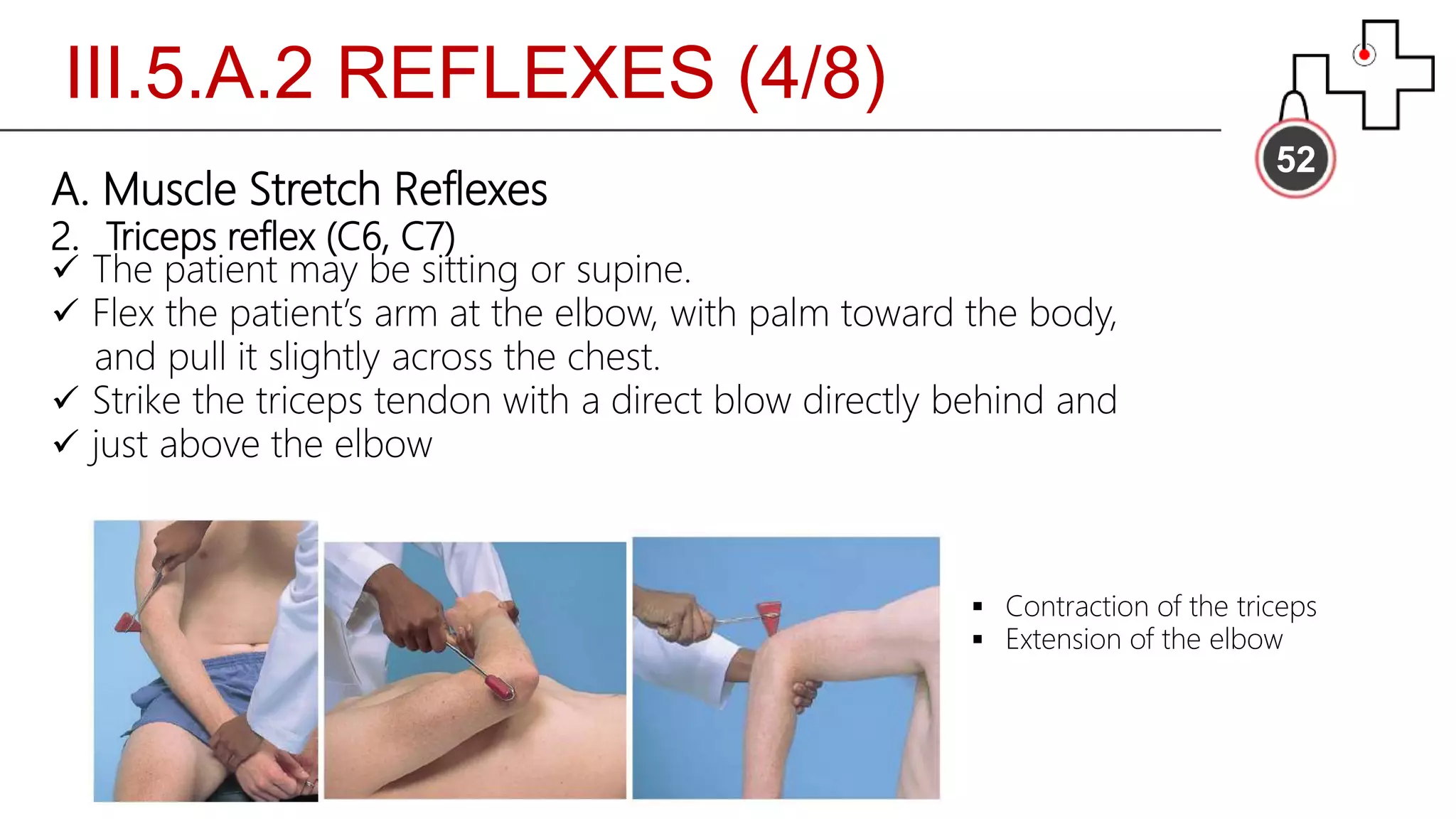
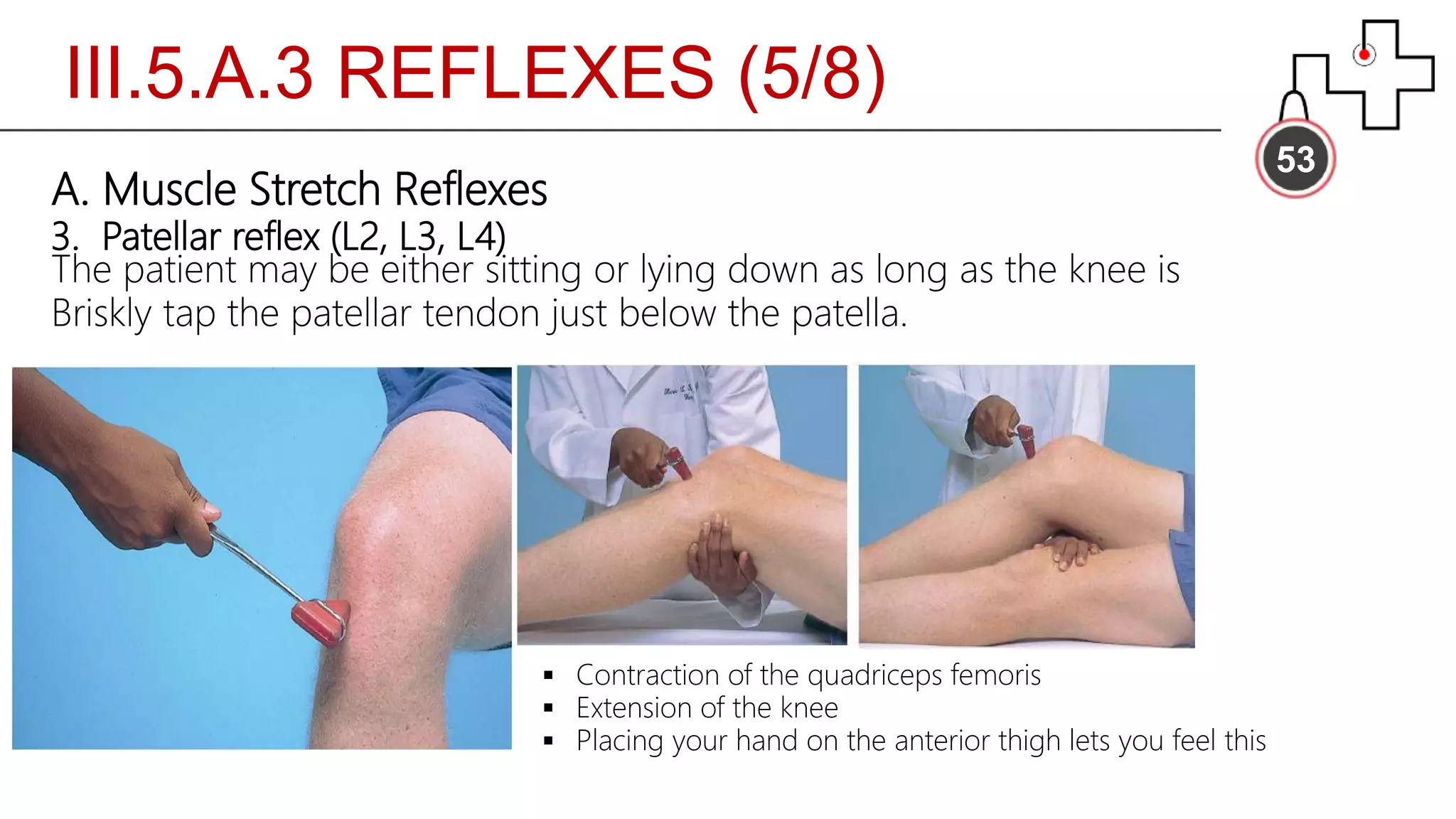
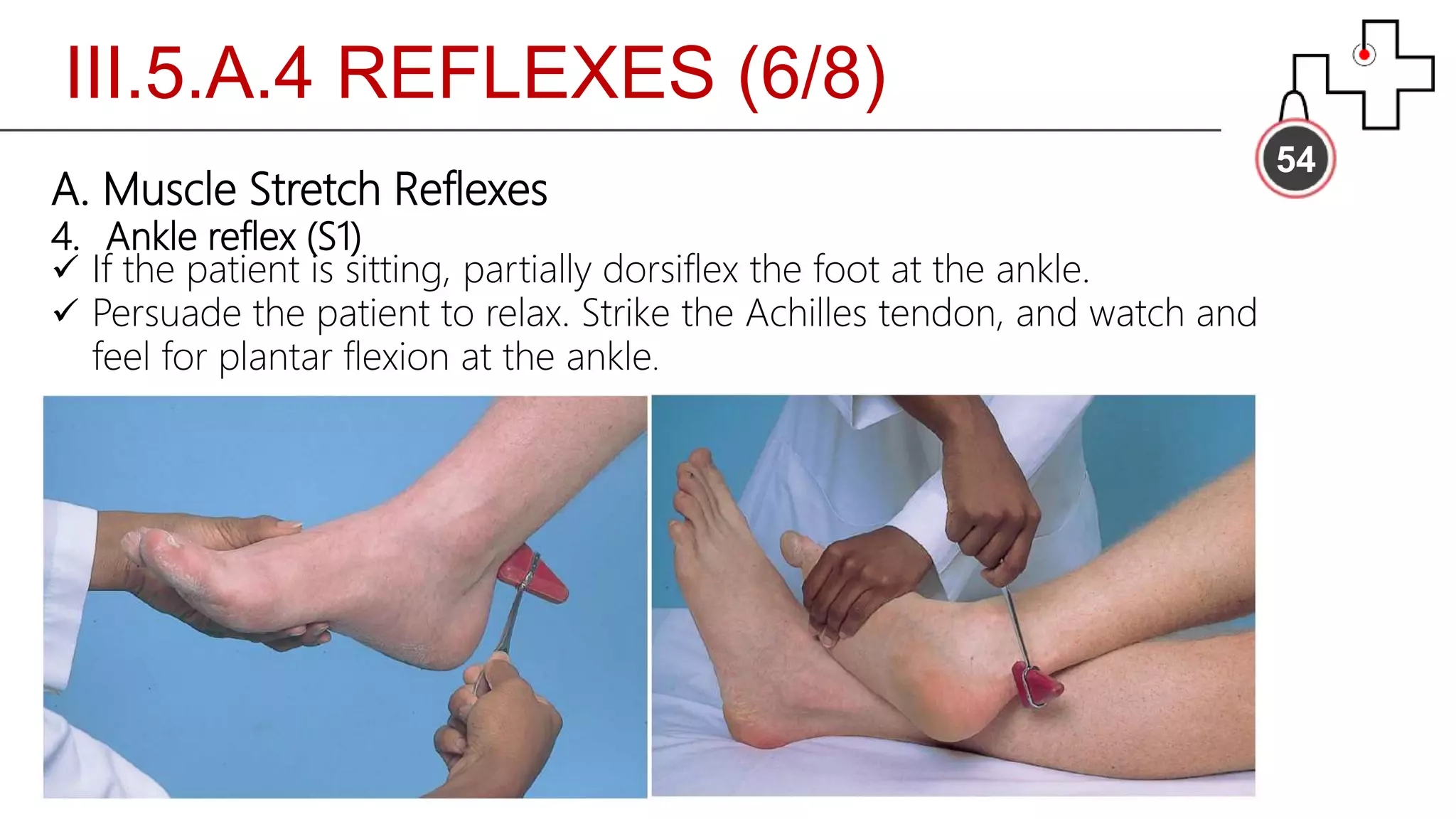
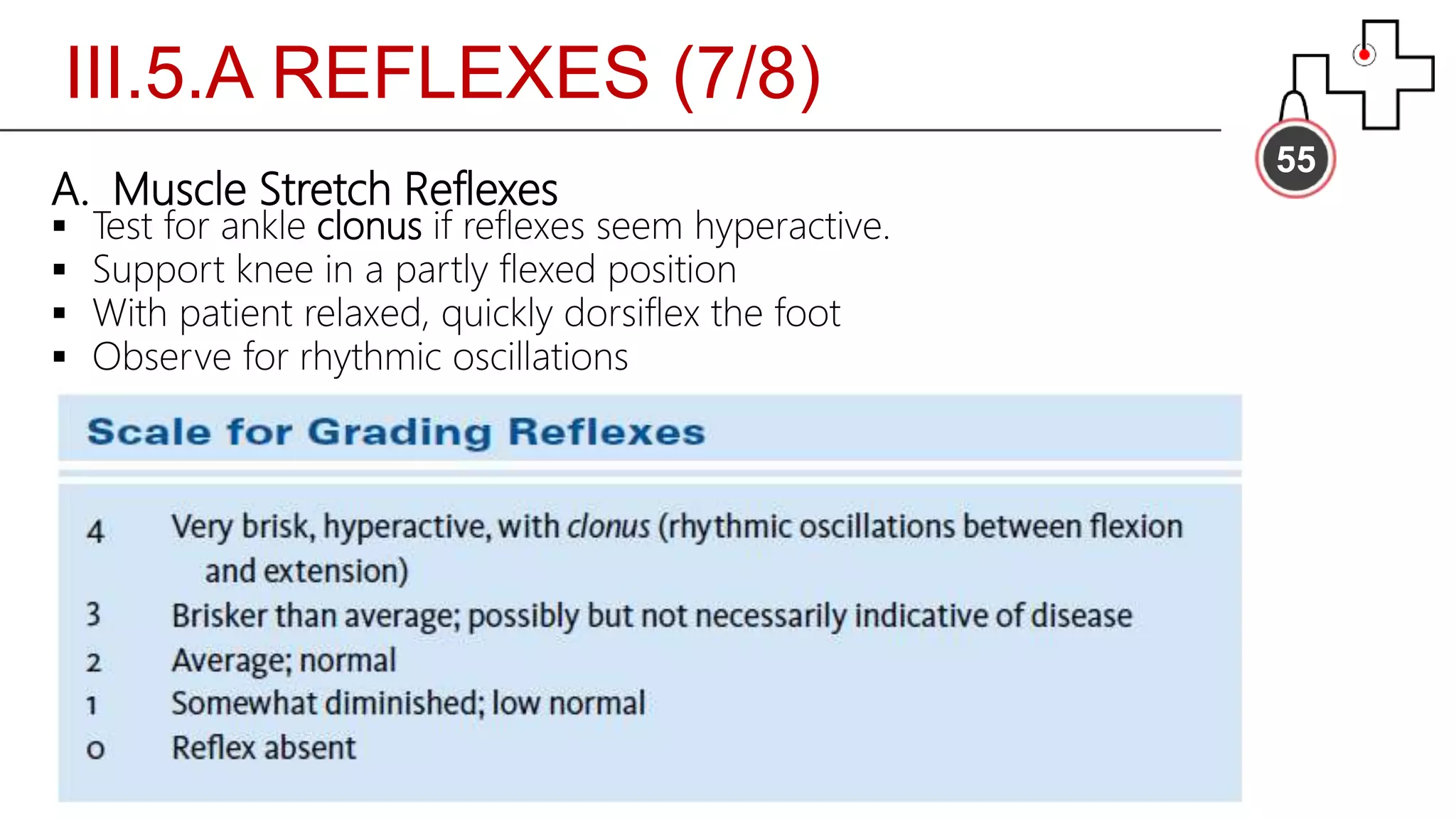
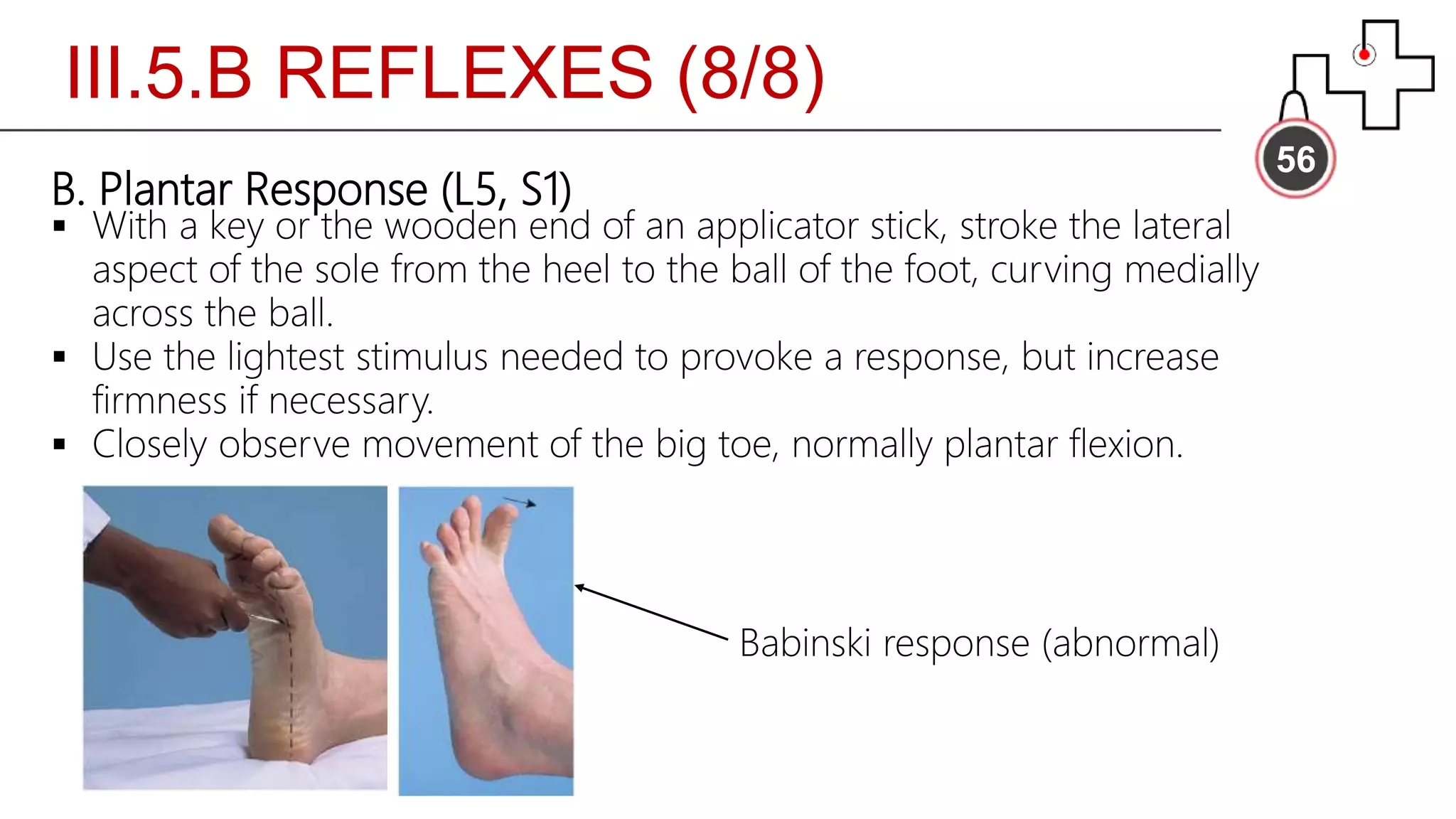
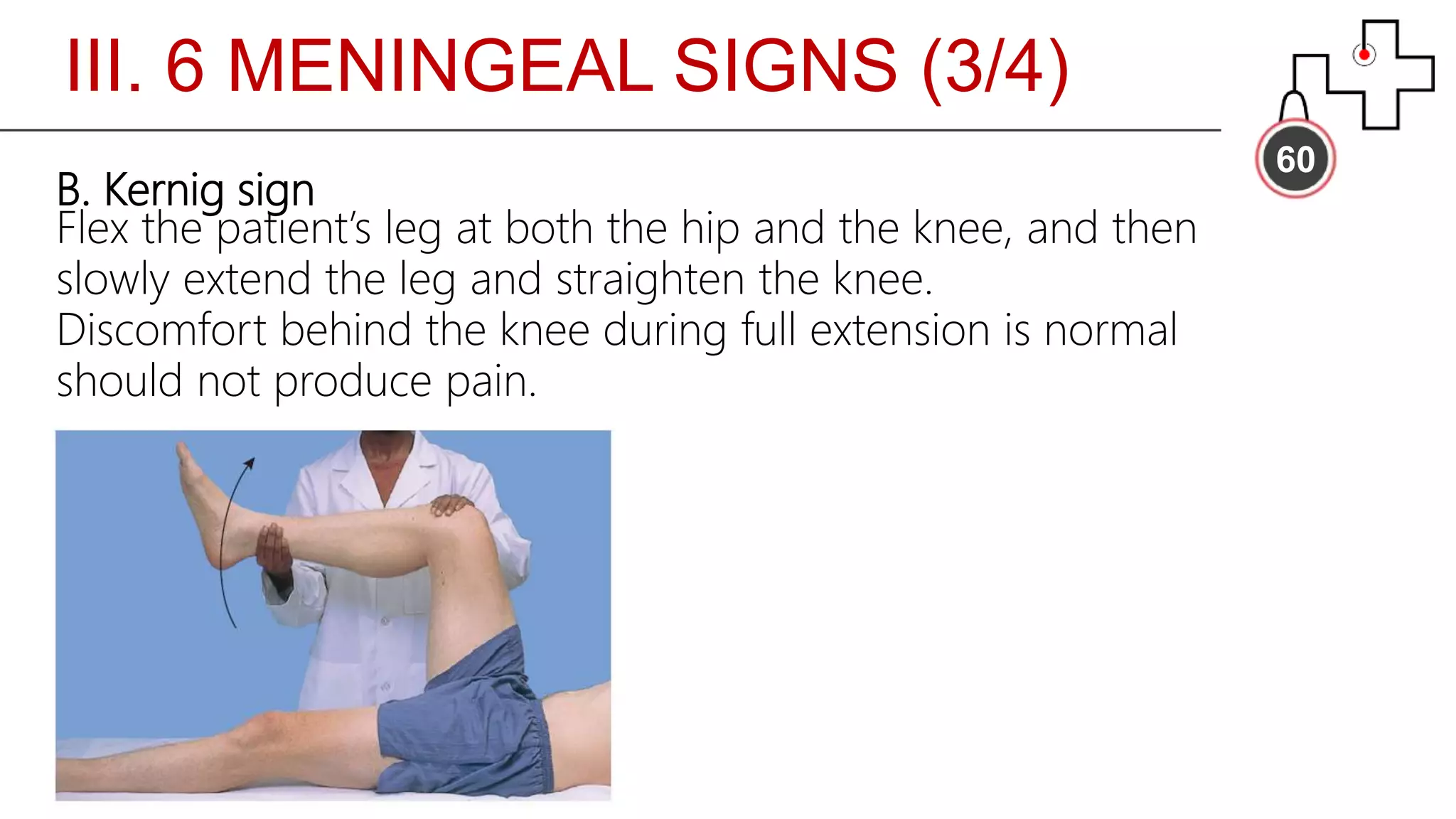
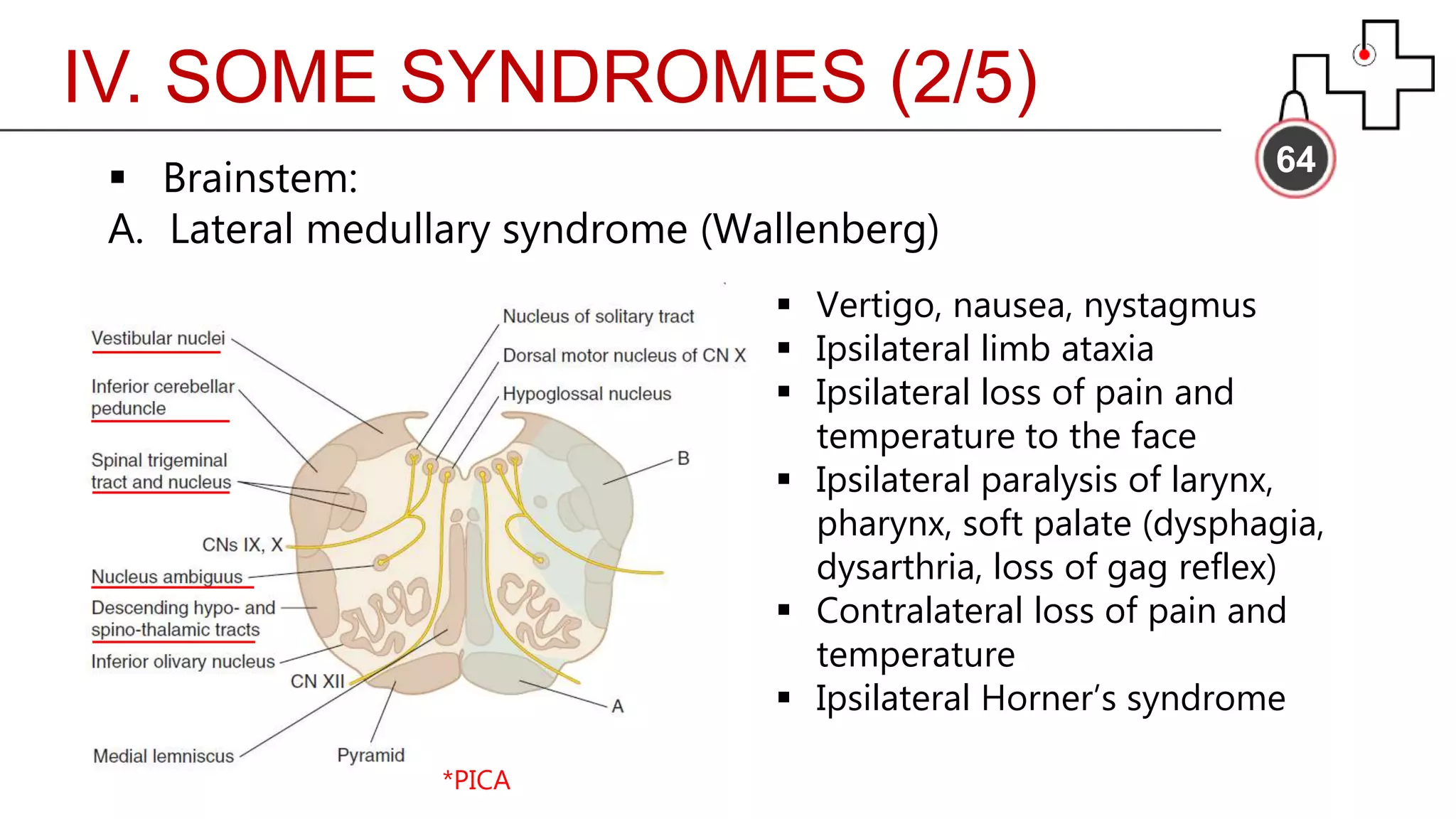
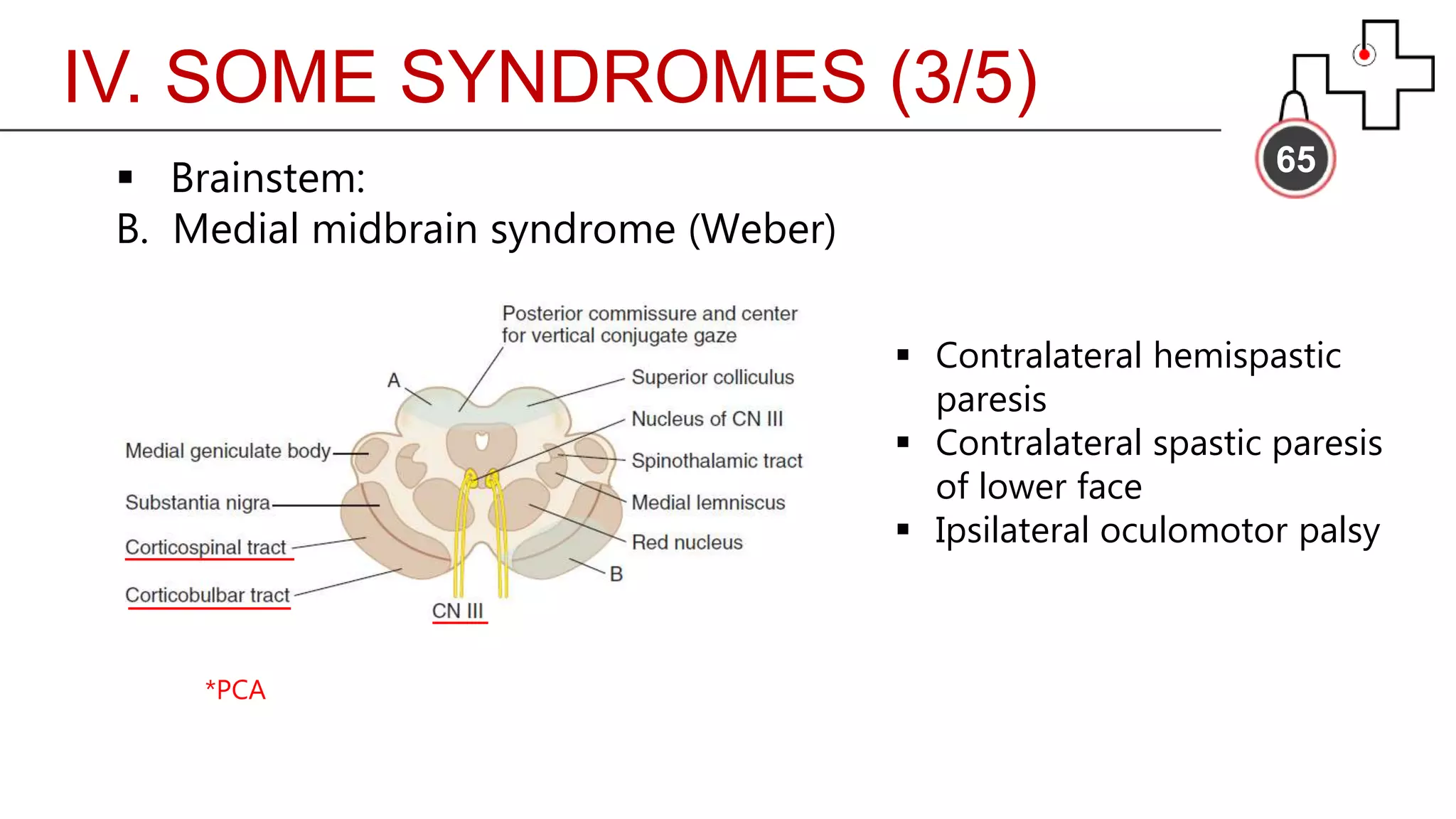
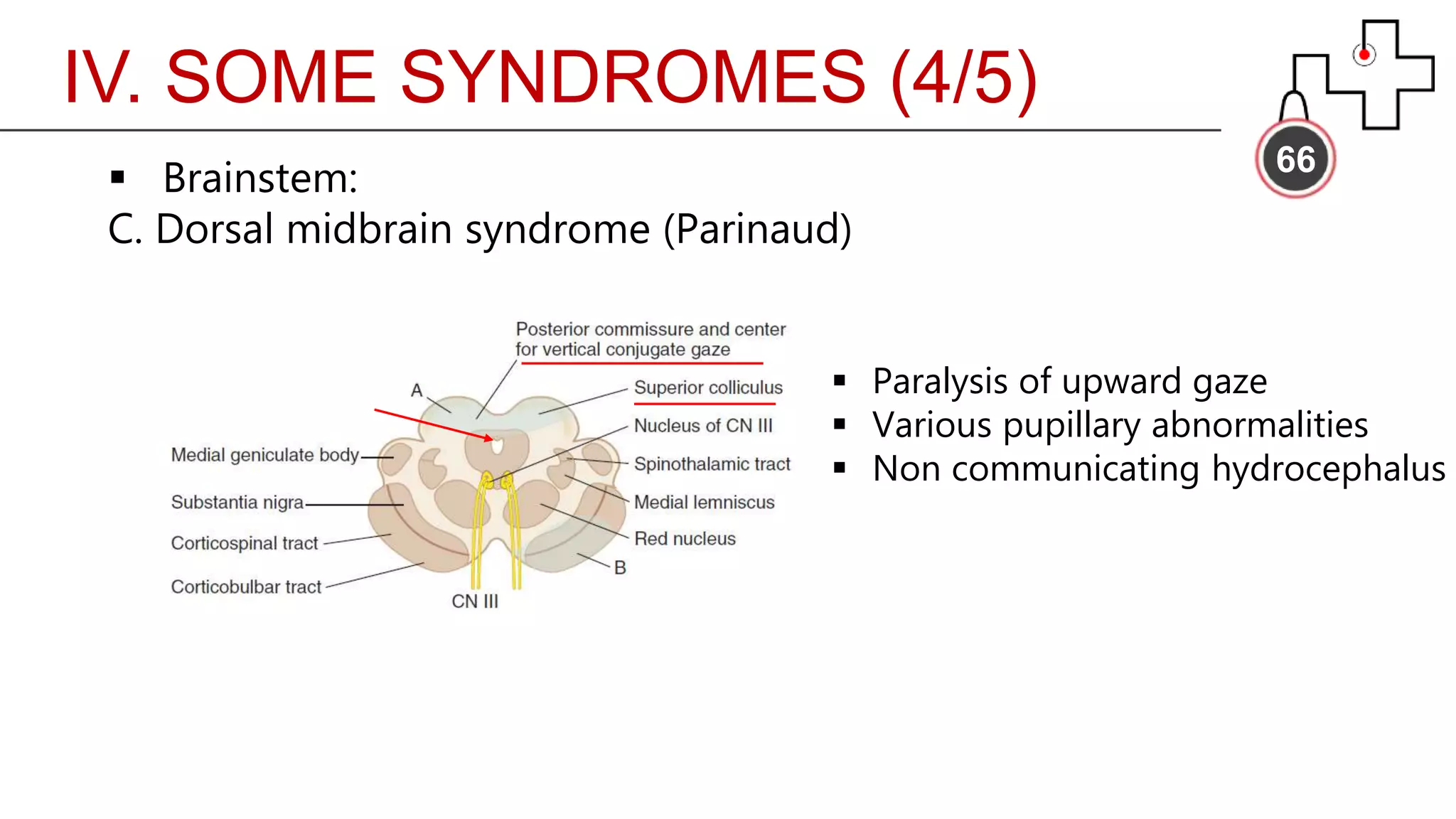
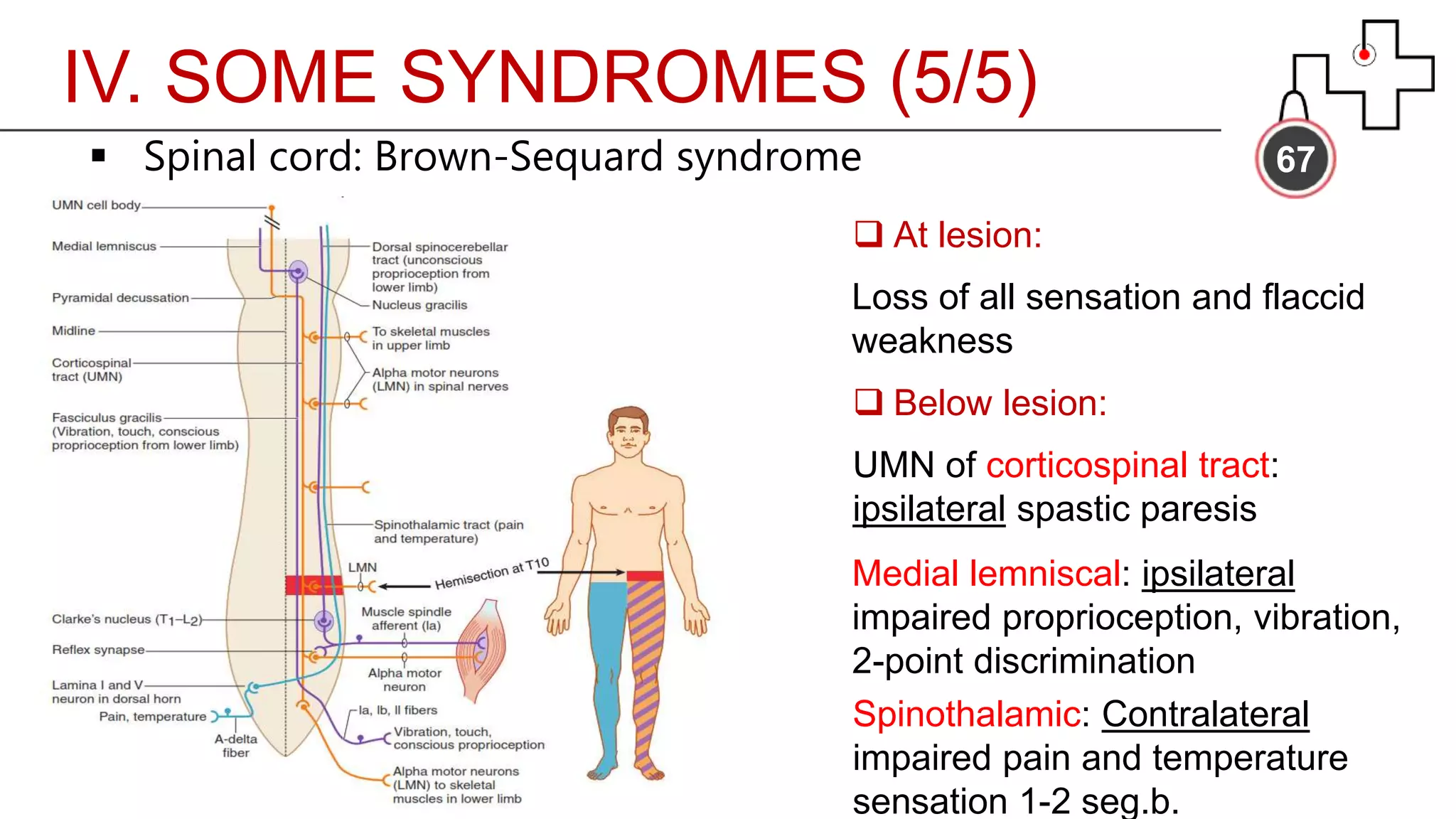
The document outlines the components and procedures of a neurologic examination, emphasizing the importance of history taking, common symptoms, essential screening exams, and specific syndromes. Key areas of focus include mental status, cranial nerves, motor system, sensory system, reflexes, and meningeal signs. The content reinforces the need for a structured approach and familiarity with clinical terms in neurology.