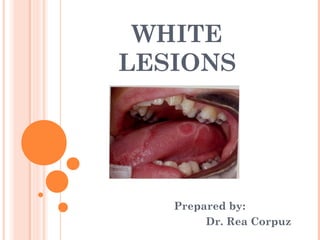
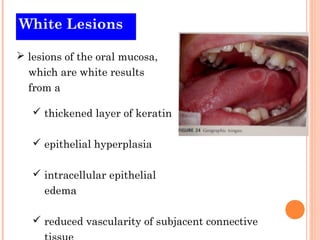
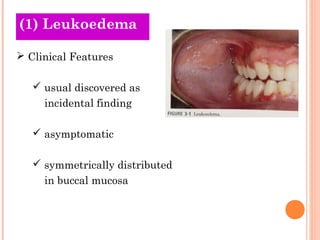
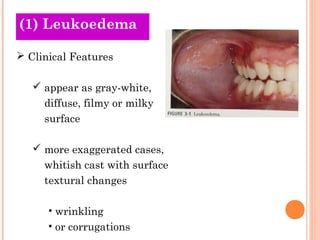
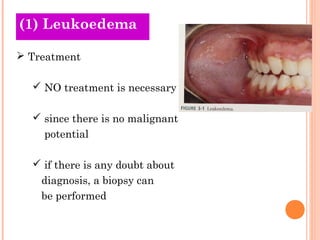
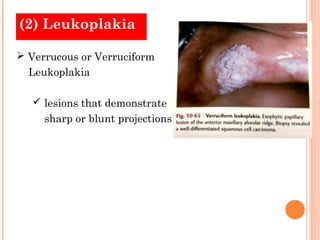
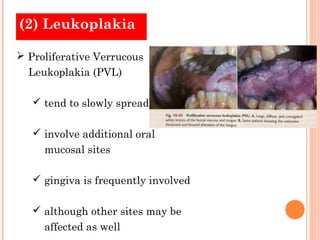
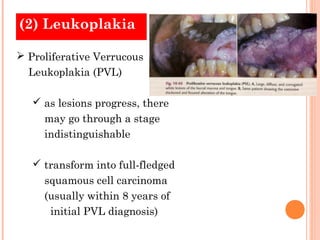
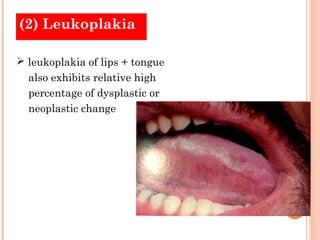
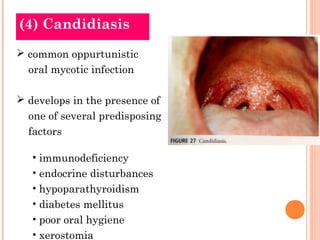
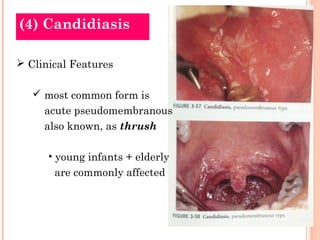
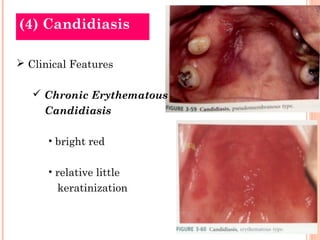
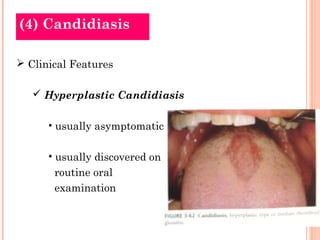
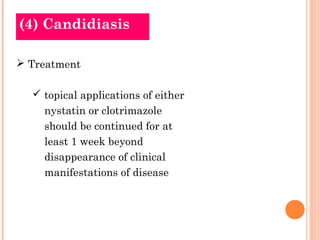
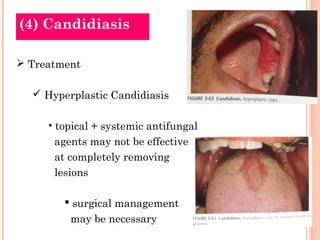
The document discusses various white oral lesions including leukoedema, leukoplakia, lichen planus, and candidiasis. Leukoedema is a common white lesion considered normal variation, while leukoplakia is a premalignant condition defined as a white patch that is not caused by other disease. Lichen planus is a chronic inflammatory disease presenting as bilateral white lesions, and candidiasis is an opportunistic fungal infection caused by Candida albicans.