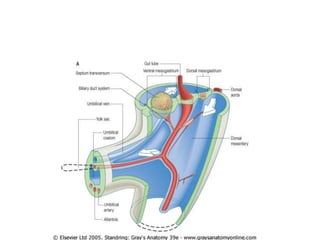
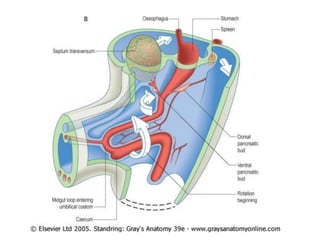
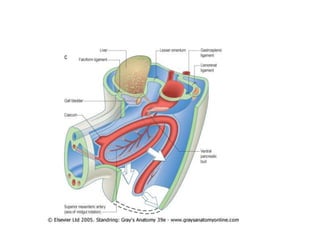
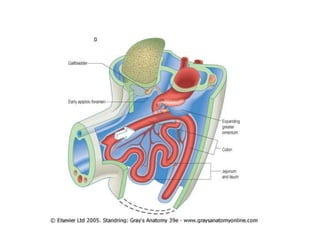
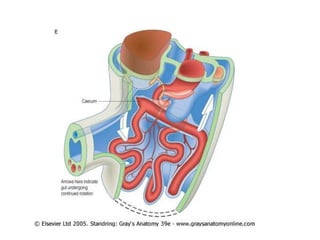
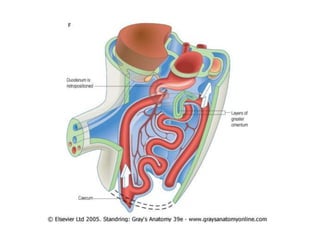
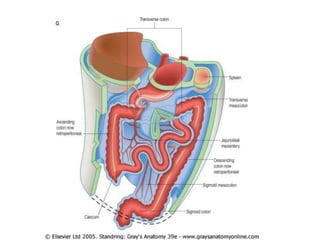
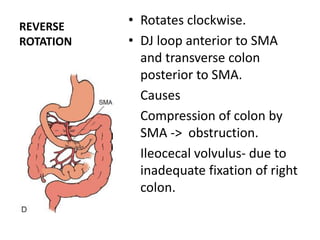
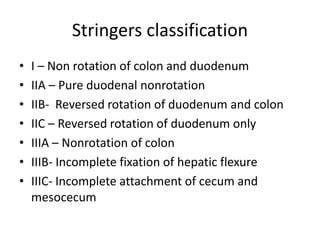
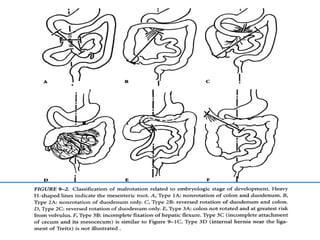
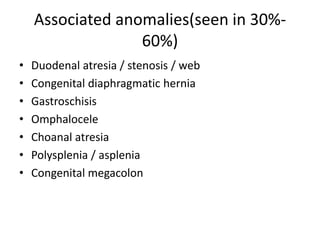
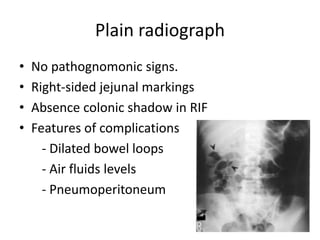
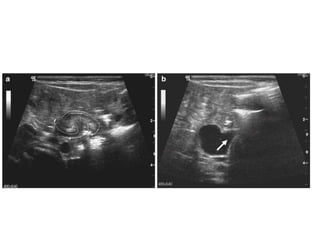
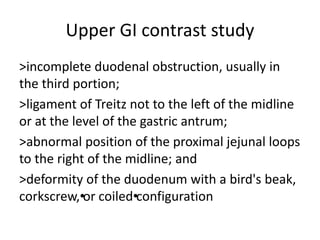
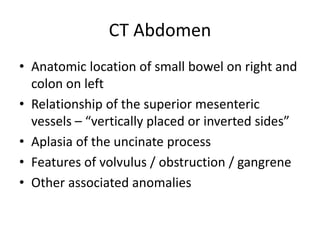
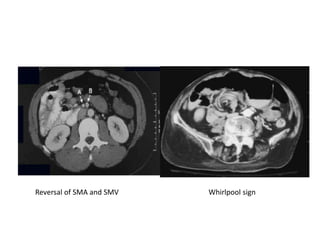
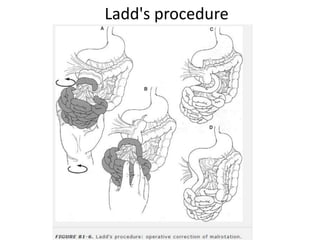
Malrotation is a congenital anomaly resulting from abnormal intestinal rotation during gestation. It can cause midgut volvulus and obstruction. Clinical presentation varies from asymptomatic to symptoms of obstruction. Diagnosis is made through imaging findings showing abnormal relationships of intestines and superior mesenteric vessels. Treatment is surgical correction through Ladd's procedure to unwind volvulus and fix intestines in normal position. Complications include recurrent volvulus and adhesive bowel obstruction.