1) The document discusses the anatomy, imaging, classification, clinical approach, and localization of spinal cord pathology. It covers various spinal cord diseases including compressive myelopathy, non-compressive myelopathy, intramedullary and extramedullary lesions.
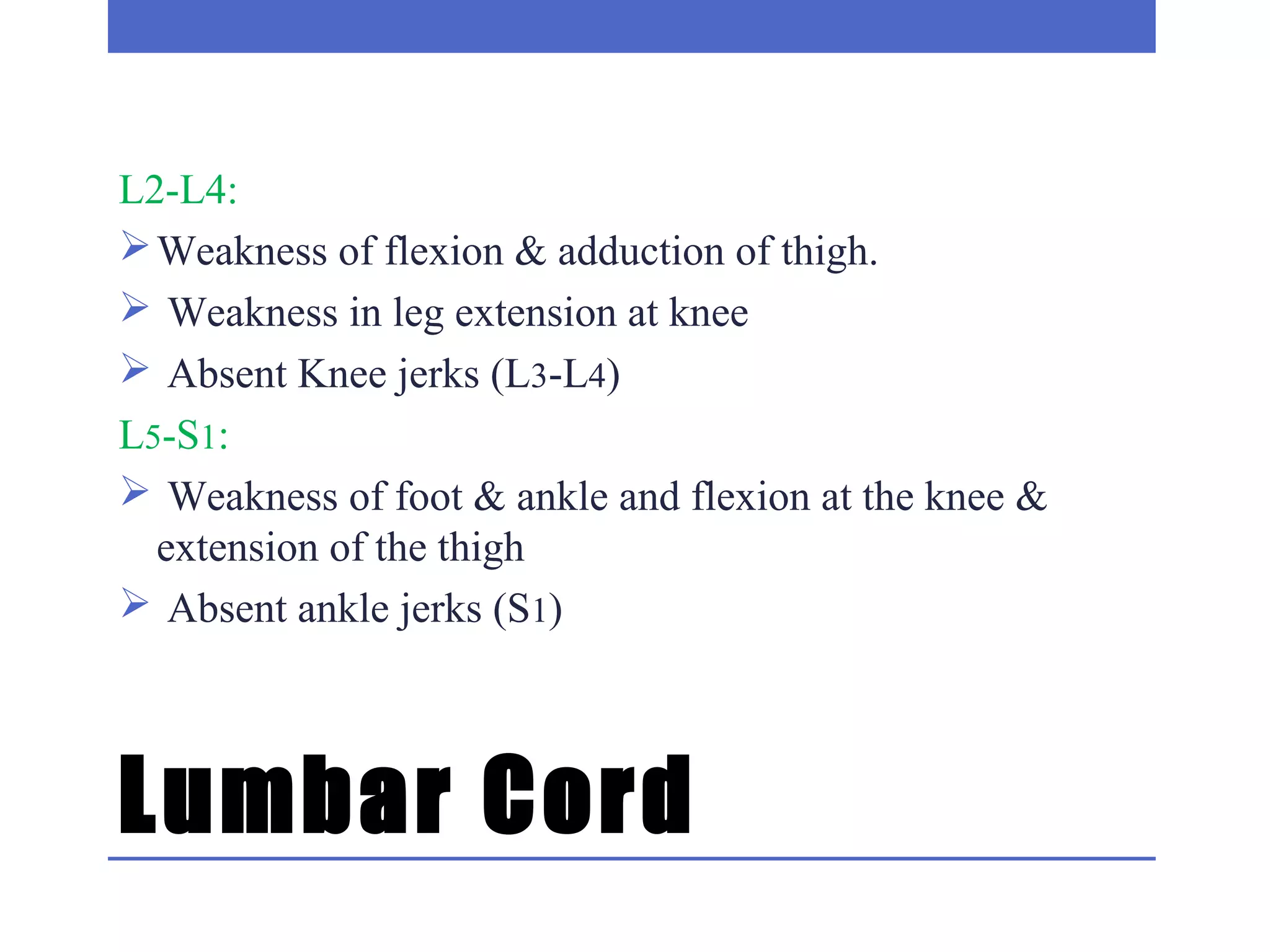
2) Special patterns of presentation like Brown-Sequard syndrome, anterior/posterior cord syndromes, and central cord syndrome are explained. Localization of lesions in the cervical, thoracic, lumbar, and sacral regions is outlined.
3) The clinical approach involves considering features like onset, progression, bladder involvement, presence of pain, and nature of paraplegia to classify spinal cord diseases. Key points on examination include types of motor and sensory