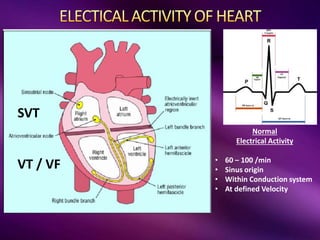
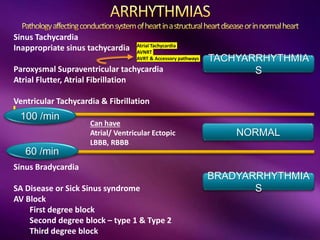
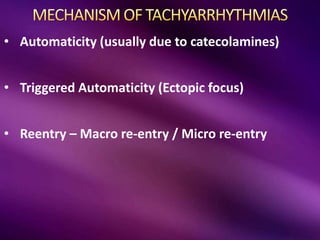
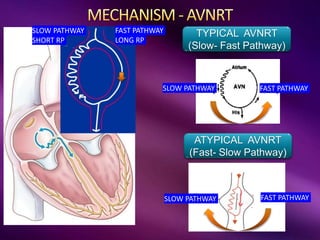
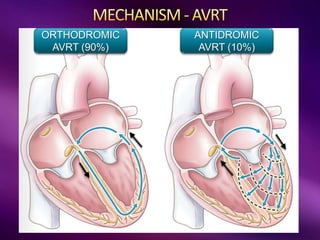
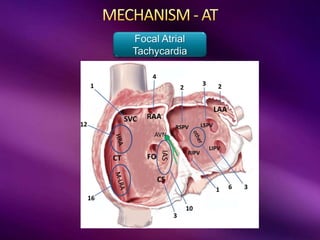
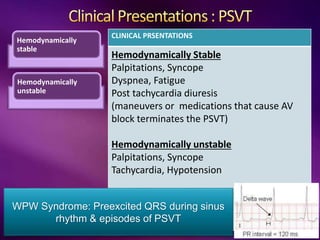
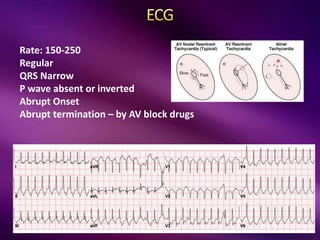
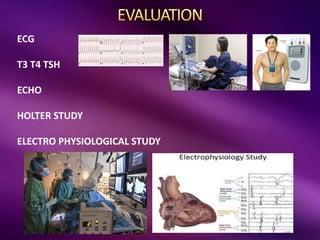
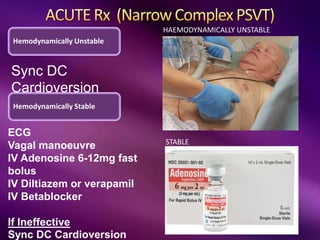
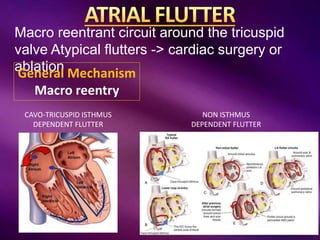
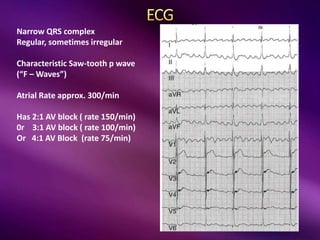
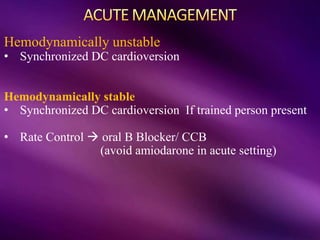
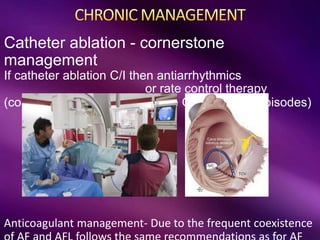
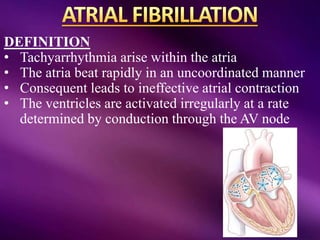
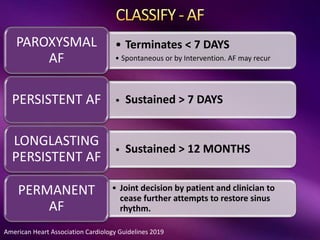
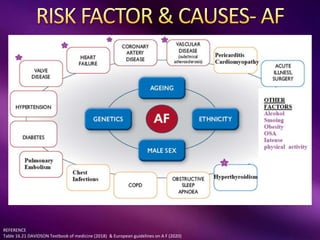
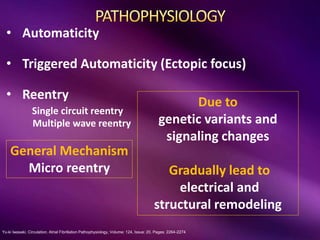
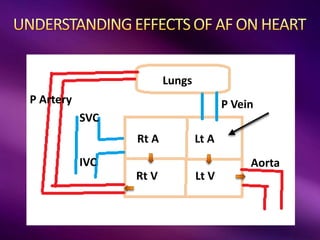
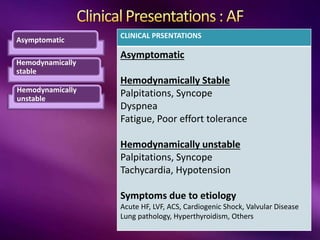
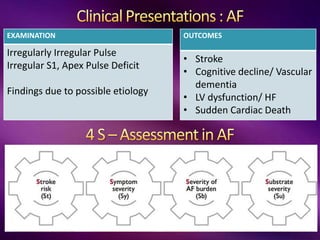
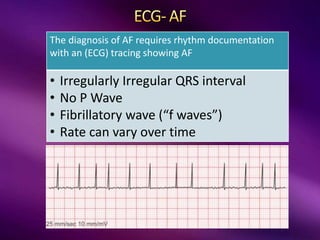
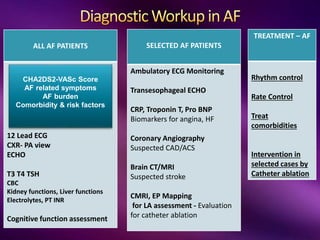
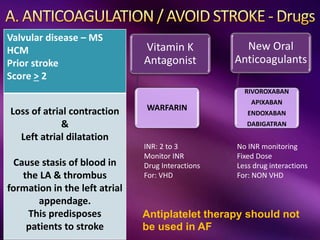
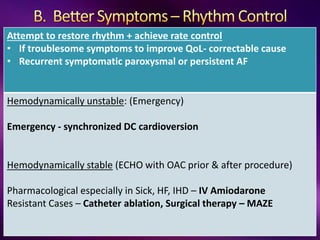
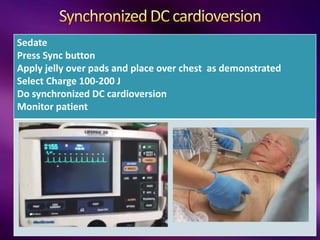
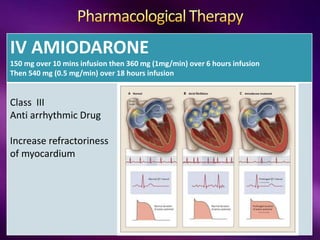
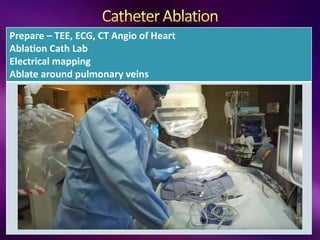
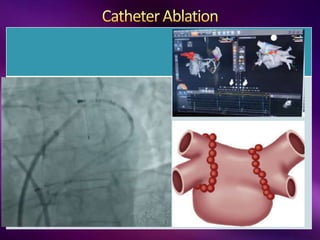
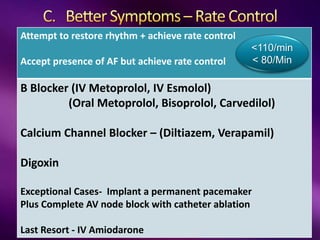
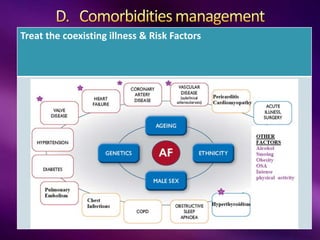
This document provides an overview of atrial fibrillation (AF) and paroxysmal supraventricular tachycardia (PSVT). It defines these conditions and describes their typical ECG patterns, mechanisms, clinical presentations, diagnostic evaluations, and treatment approaches including medications, procedures like cardioversion and ablation. Key points include: AF can be paroxysmal, persistent or permanent, and is caused by mechanisms like reentry and ectopic automaticity; evaluation involves assessing thromboembolic risk with scores like CHA2DS2-VASc; treatment focuses on rate or rhythm control with medications or ablation, while preventing thromboembolism with anticoagulation; PSVT often presents with abrupt