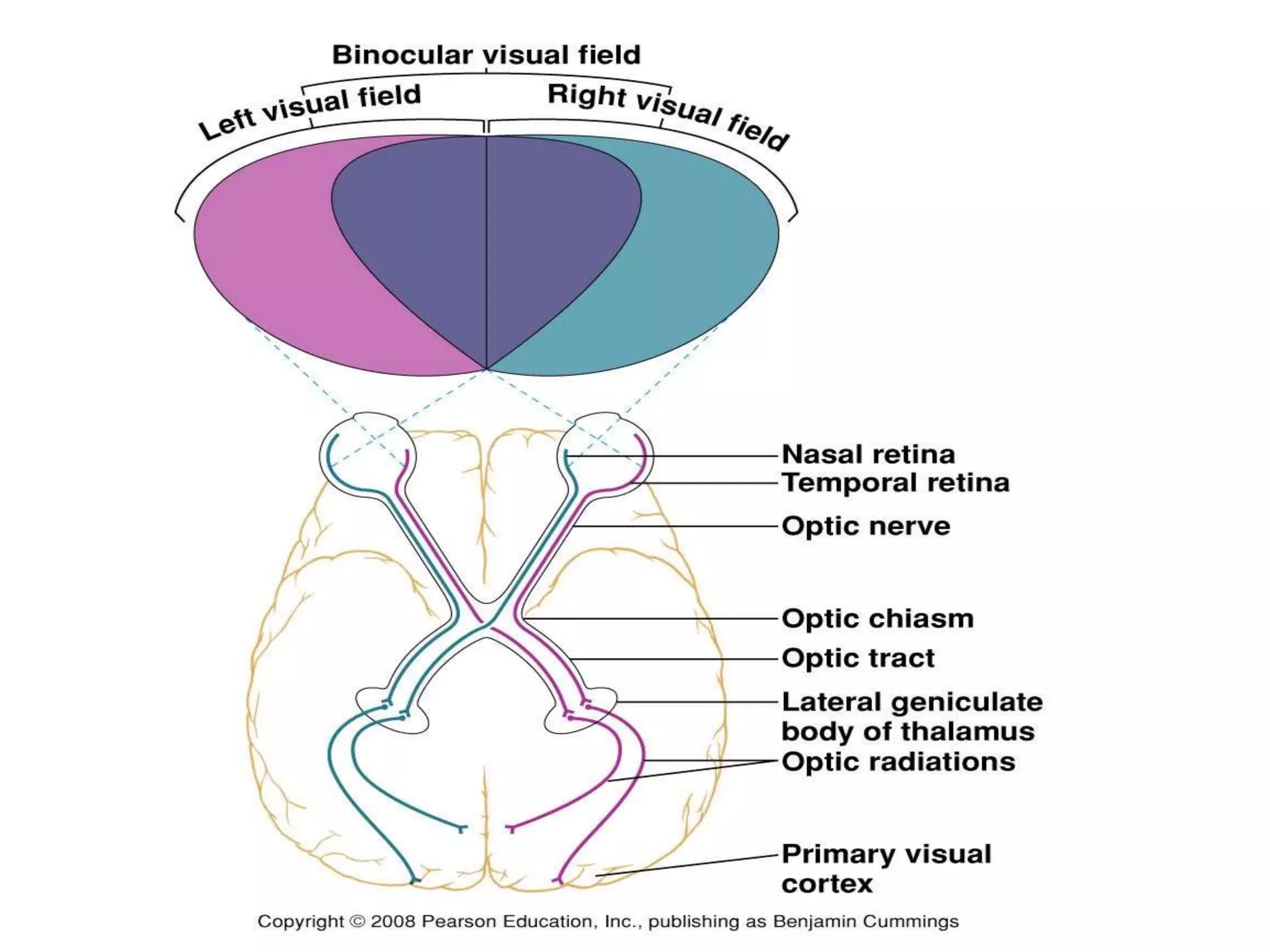
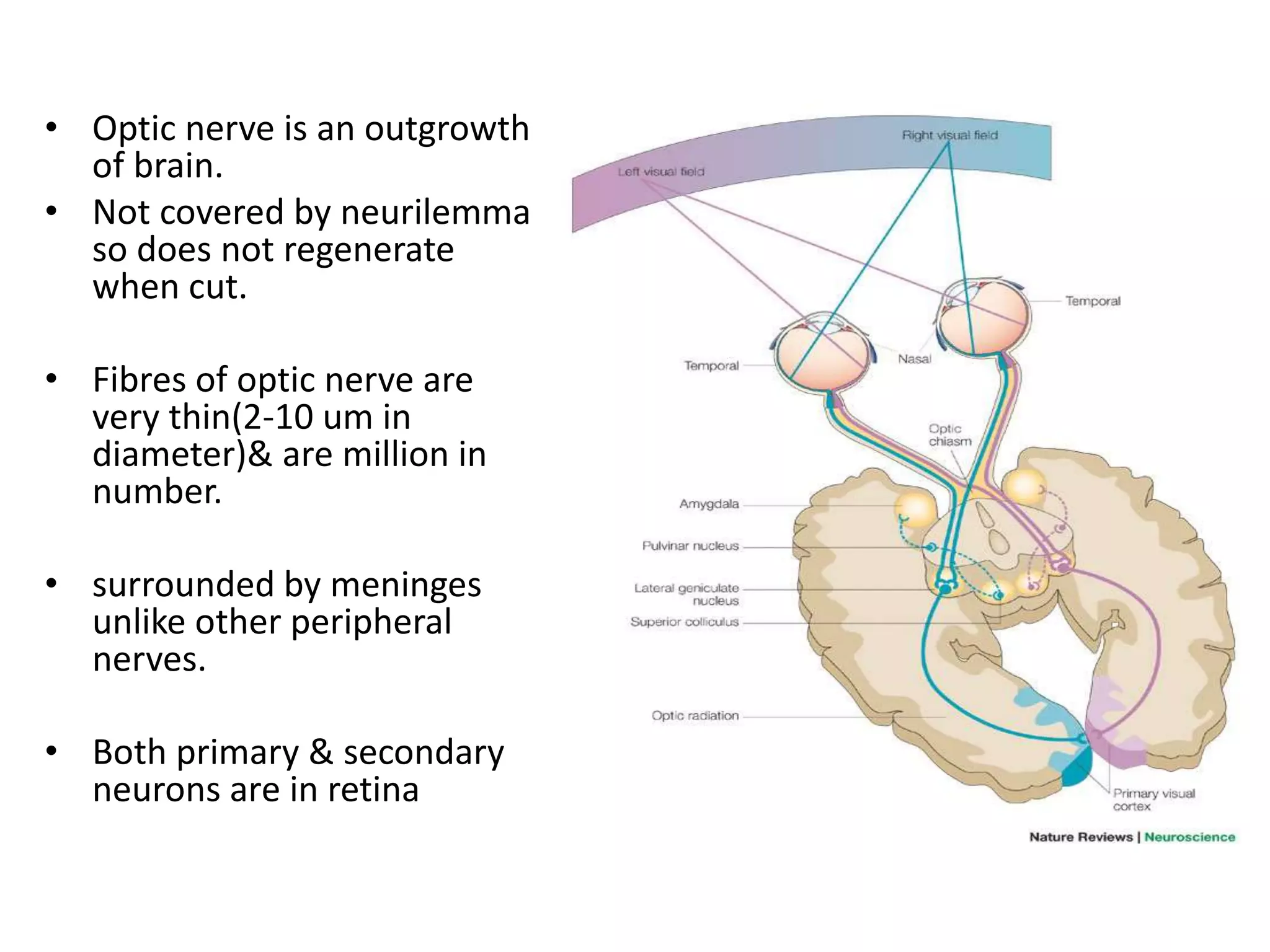
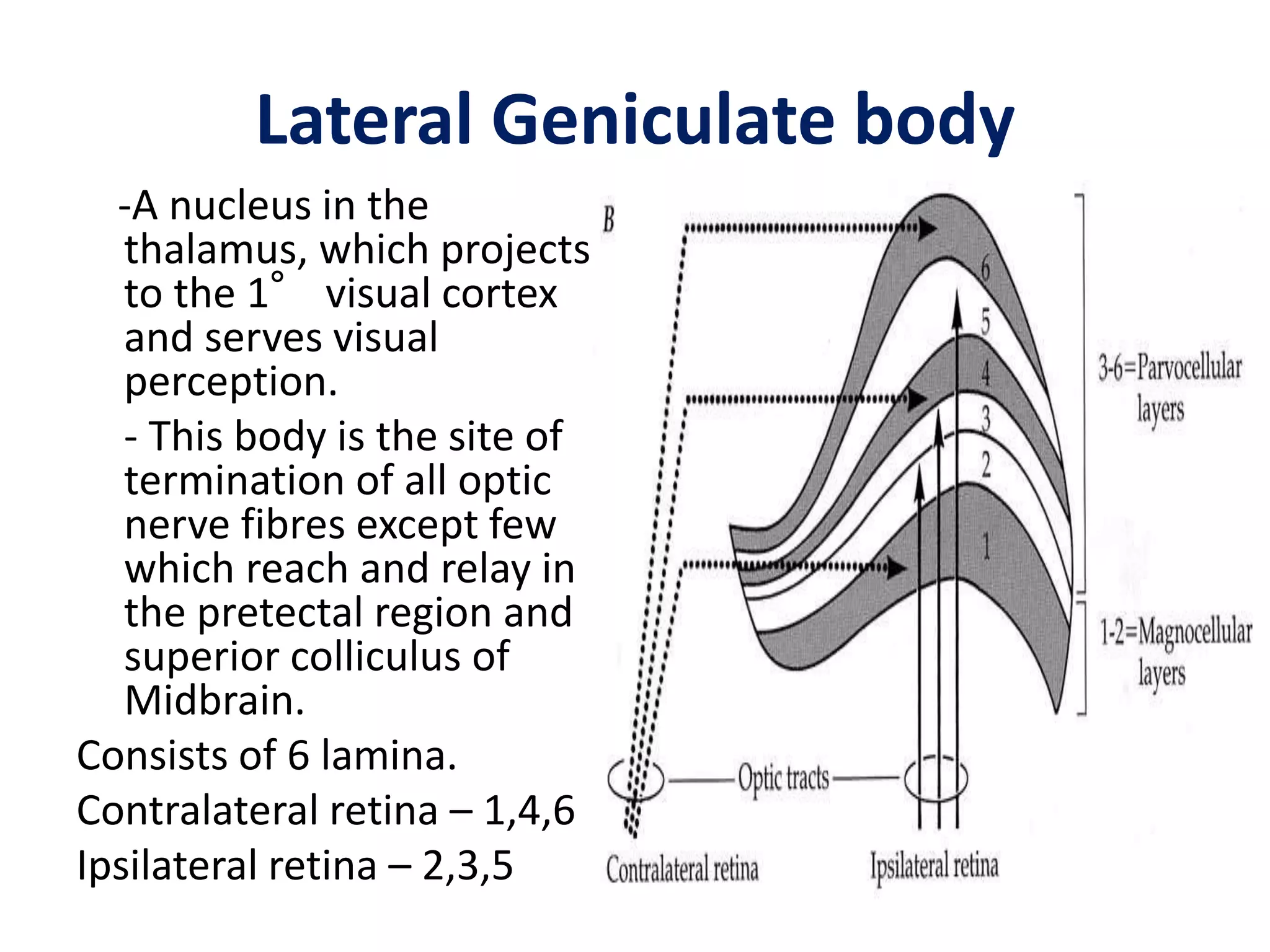
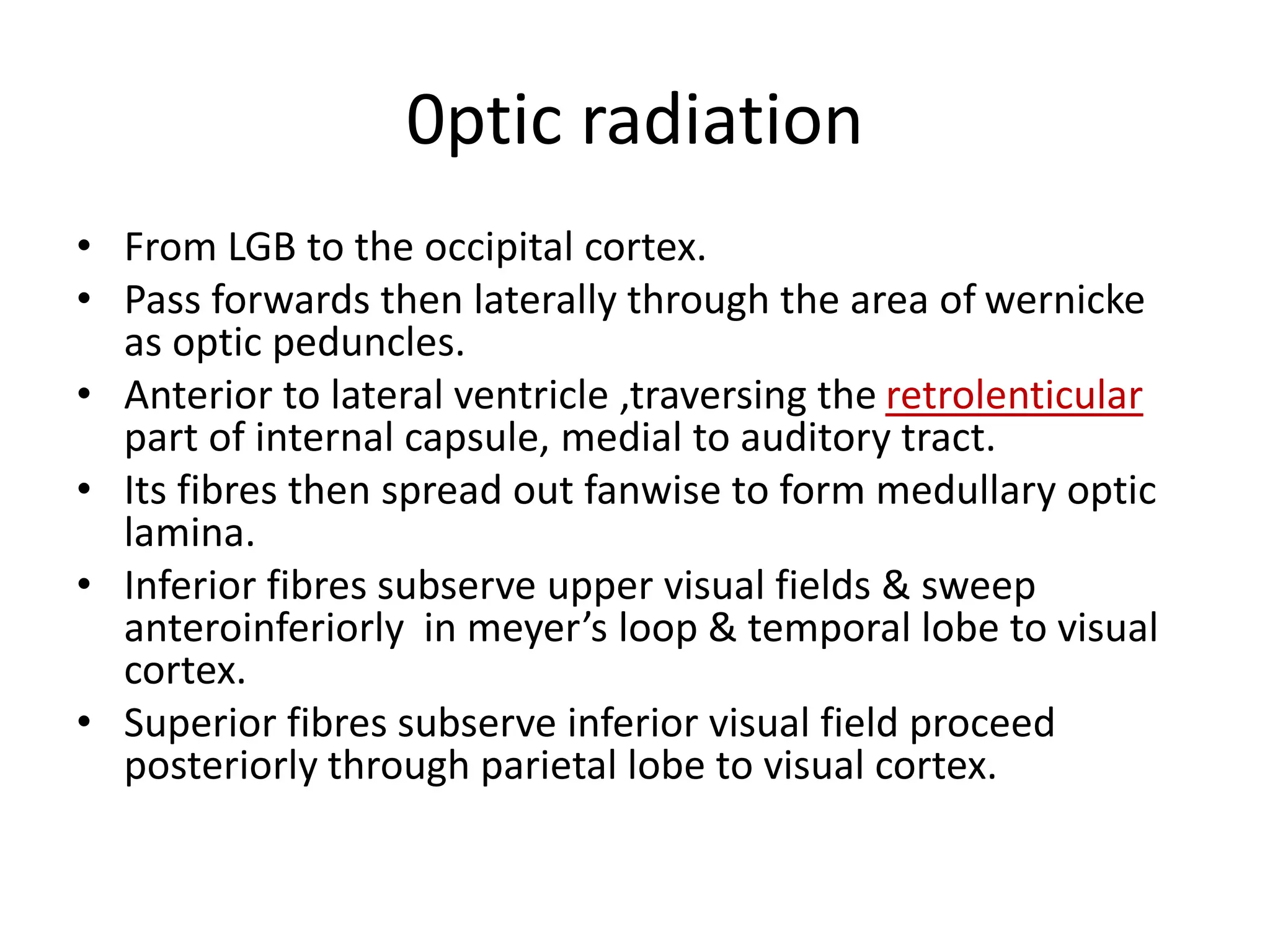
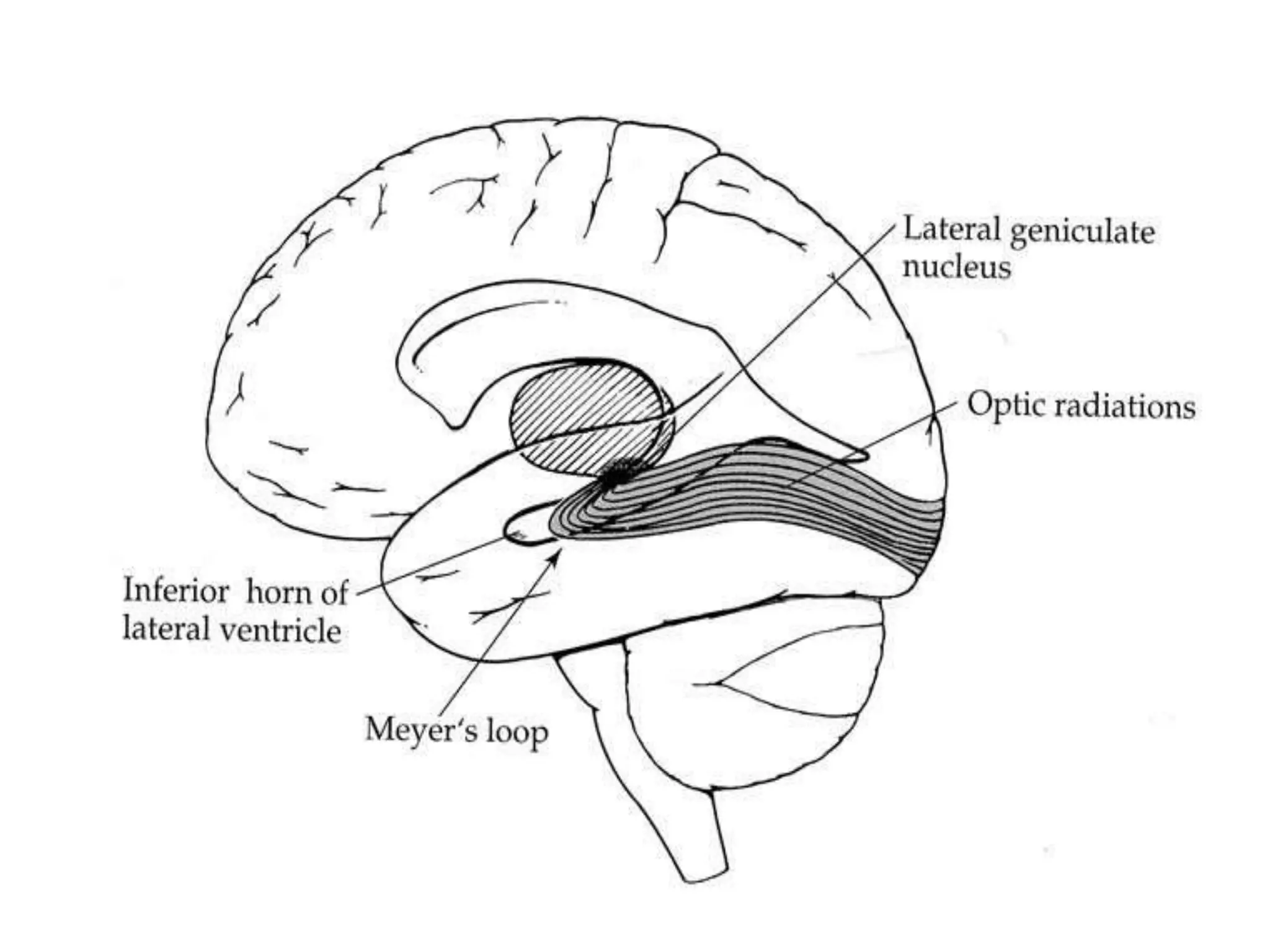
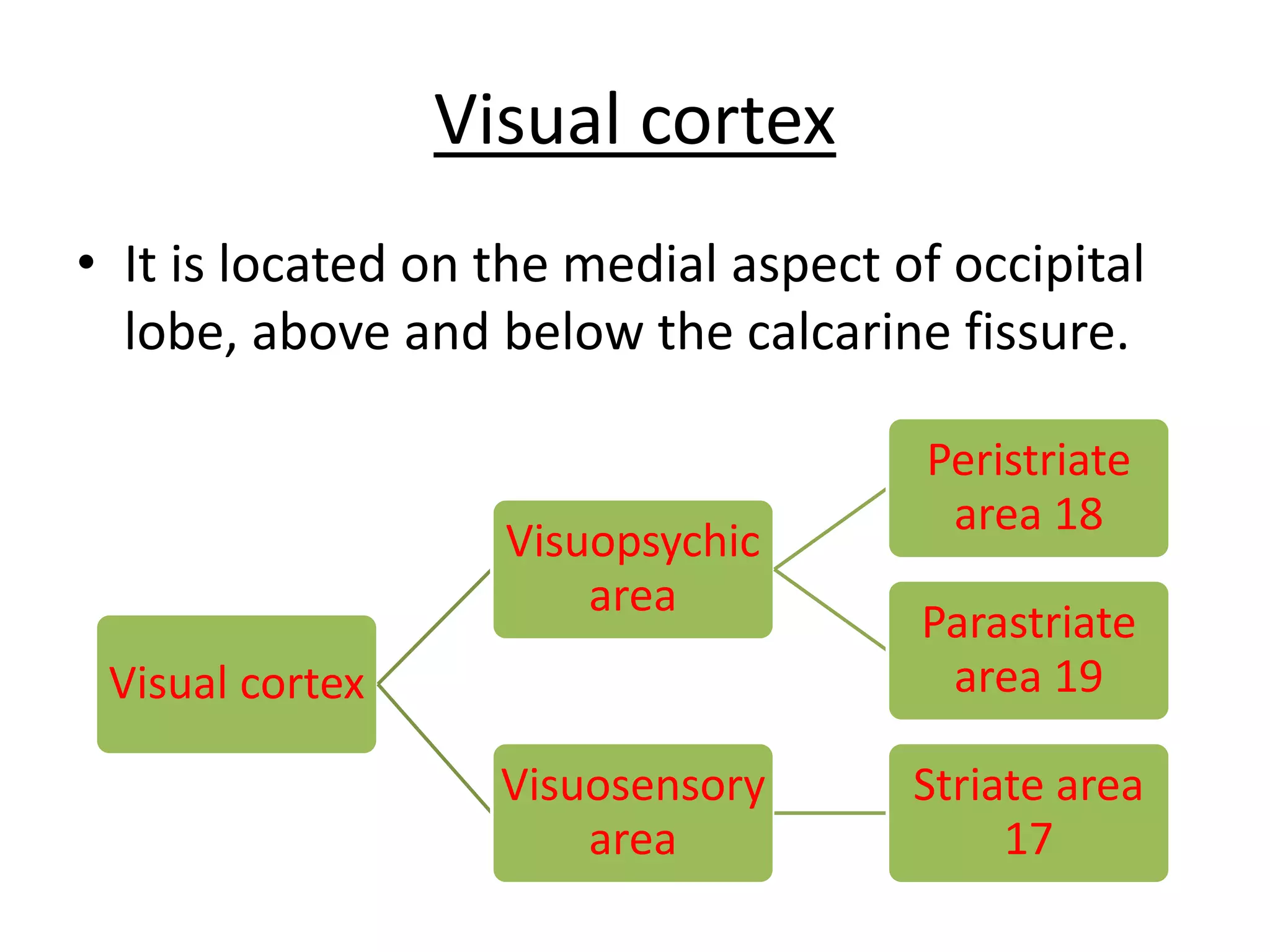
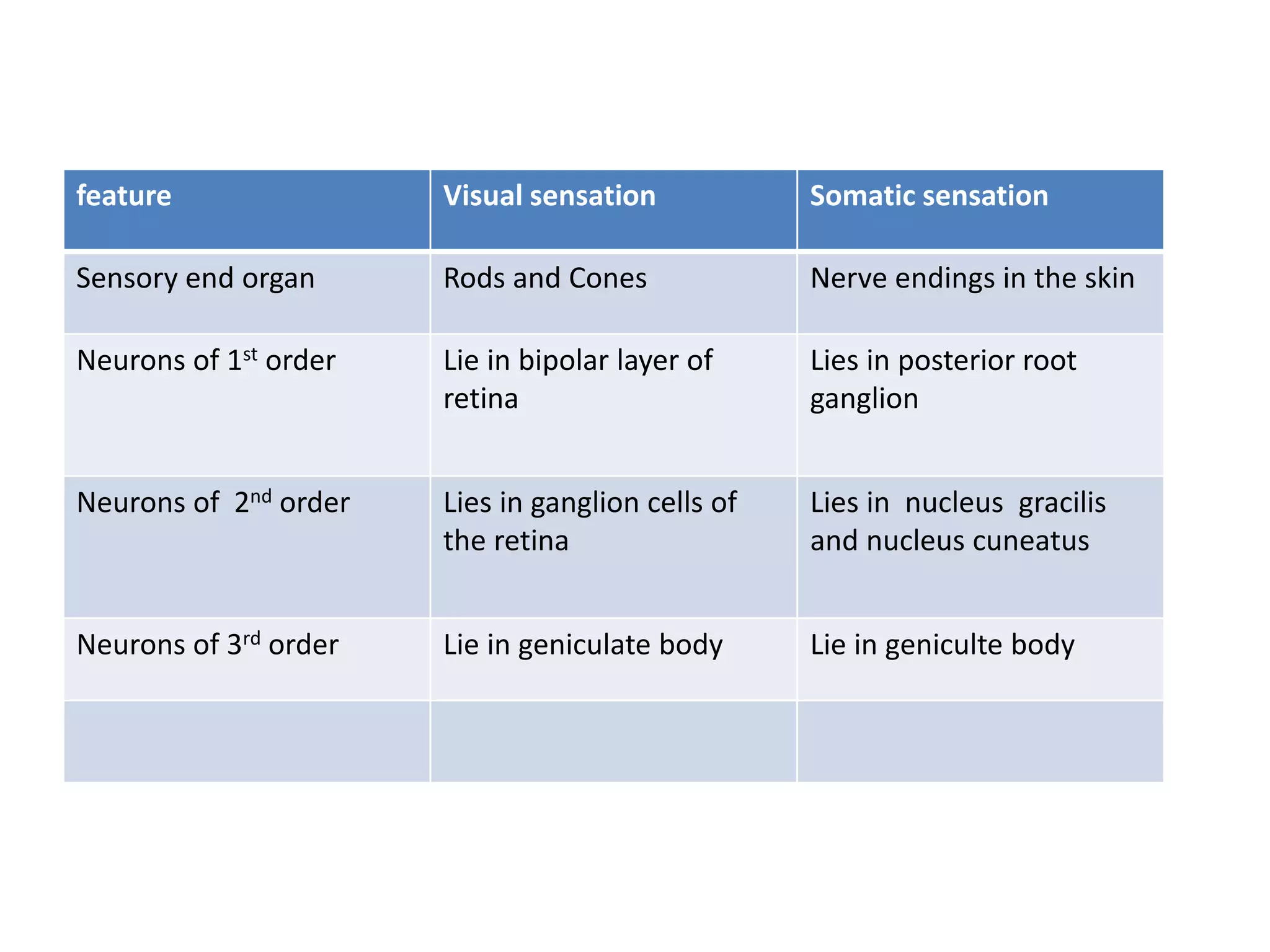
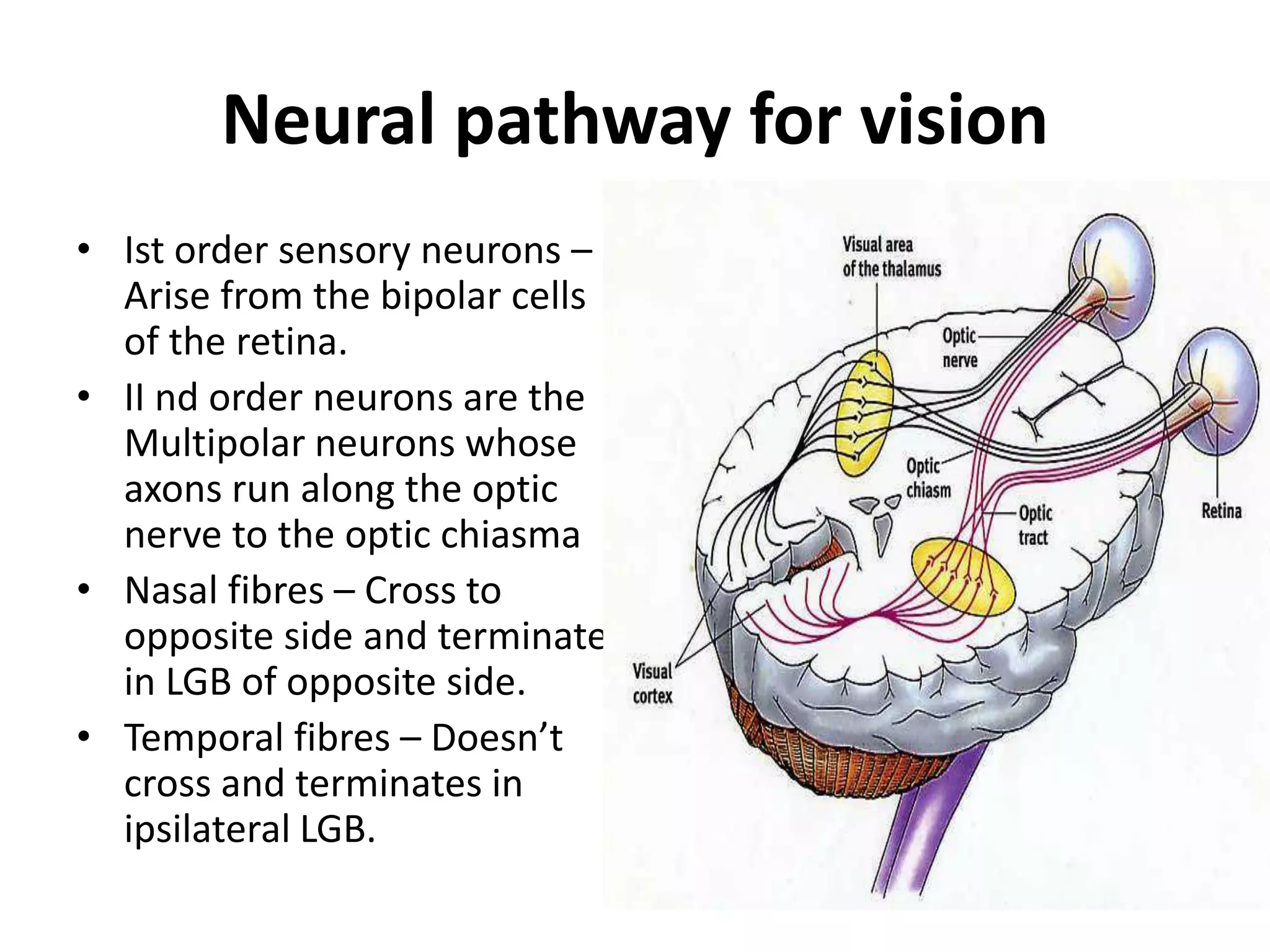
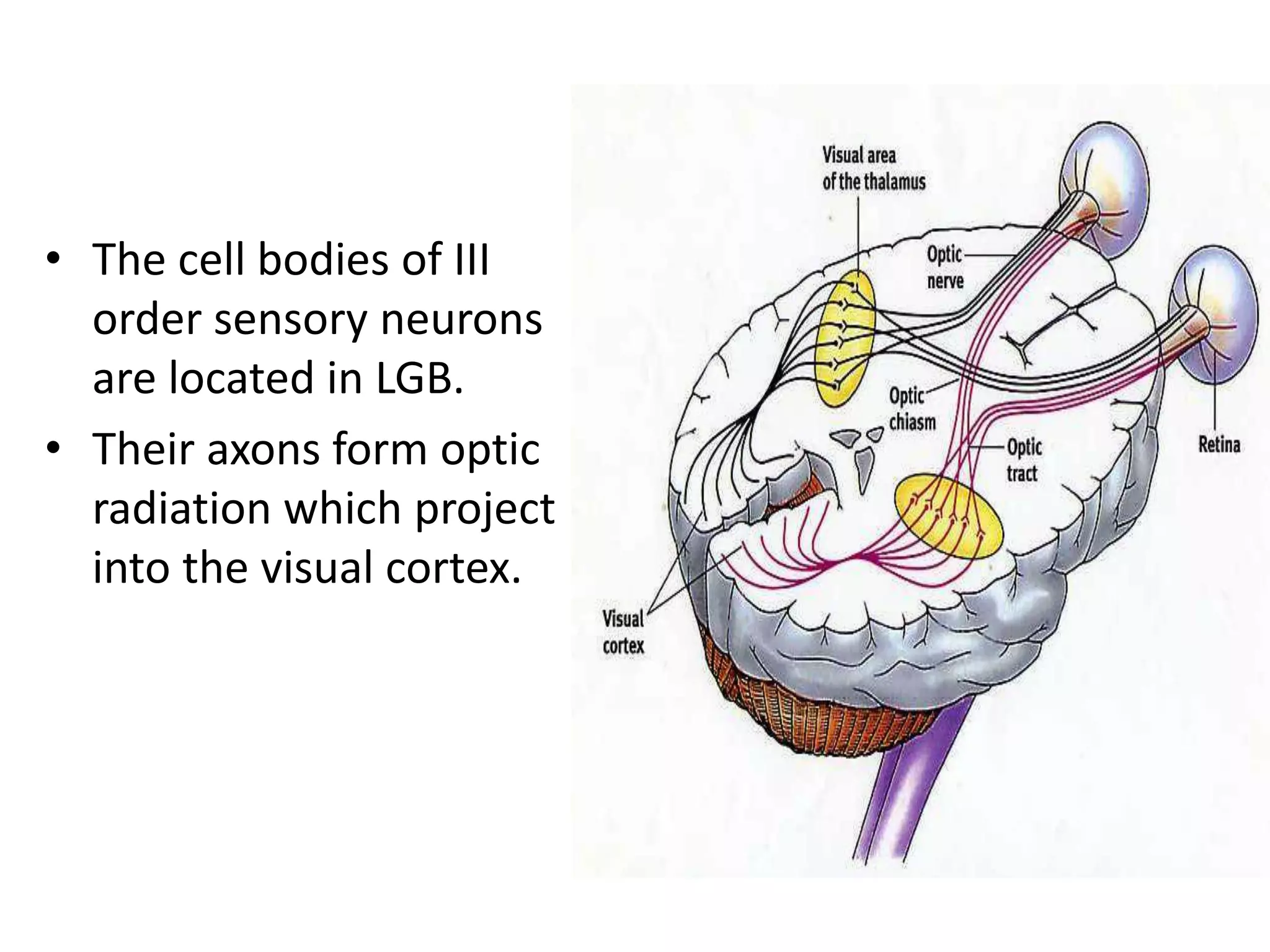
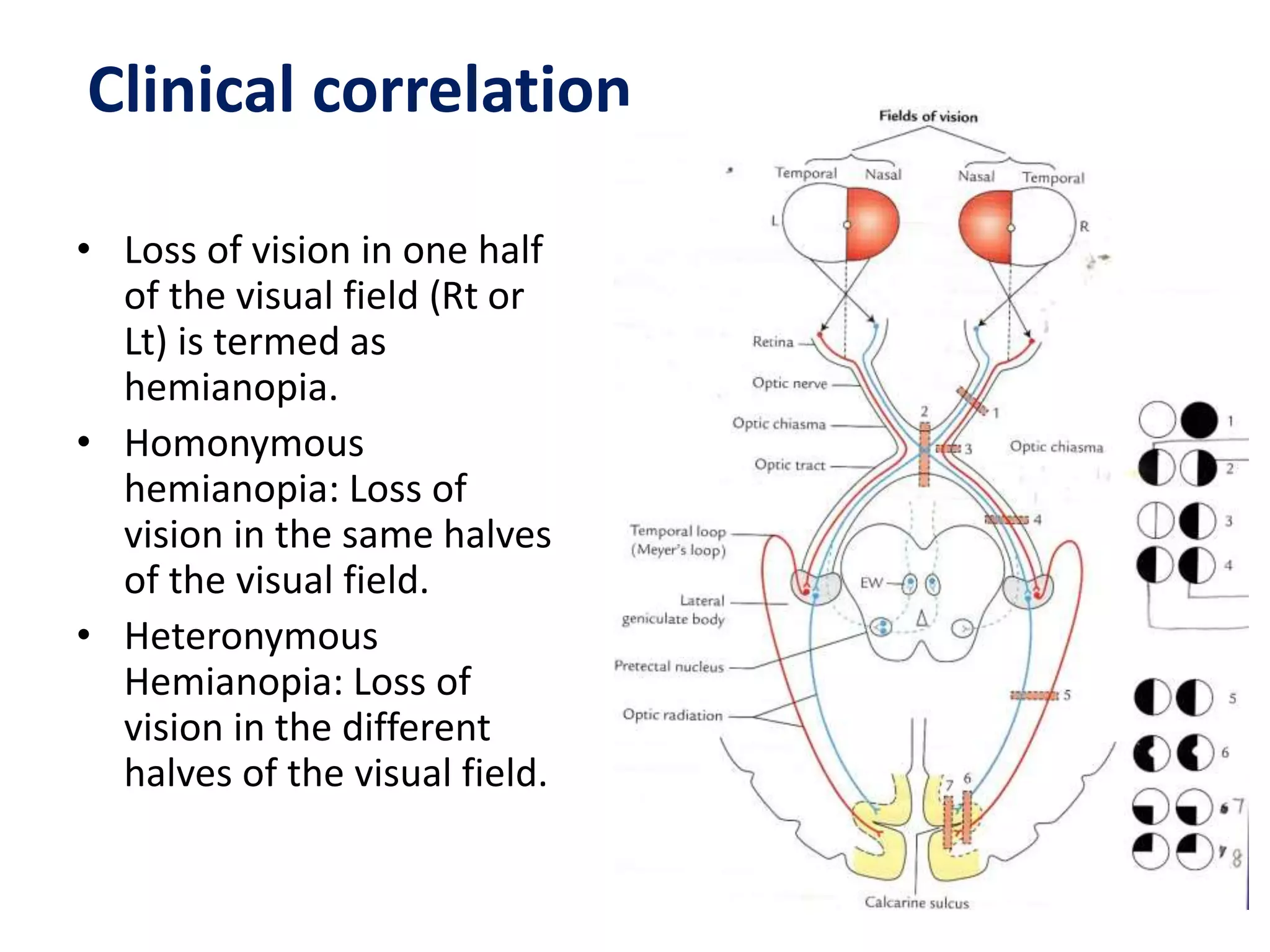
1. The visual pathway begins in the retina and passes through the optic nerve, optic chiasm, optic tract, lateral geniculate body, optic radiations, and visual cortex.
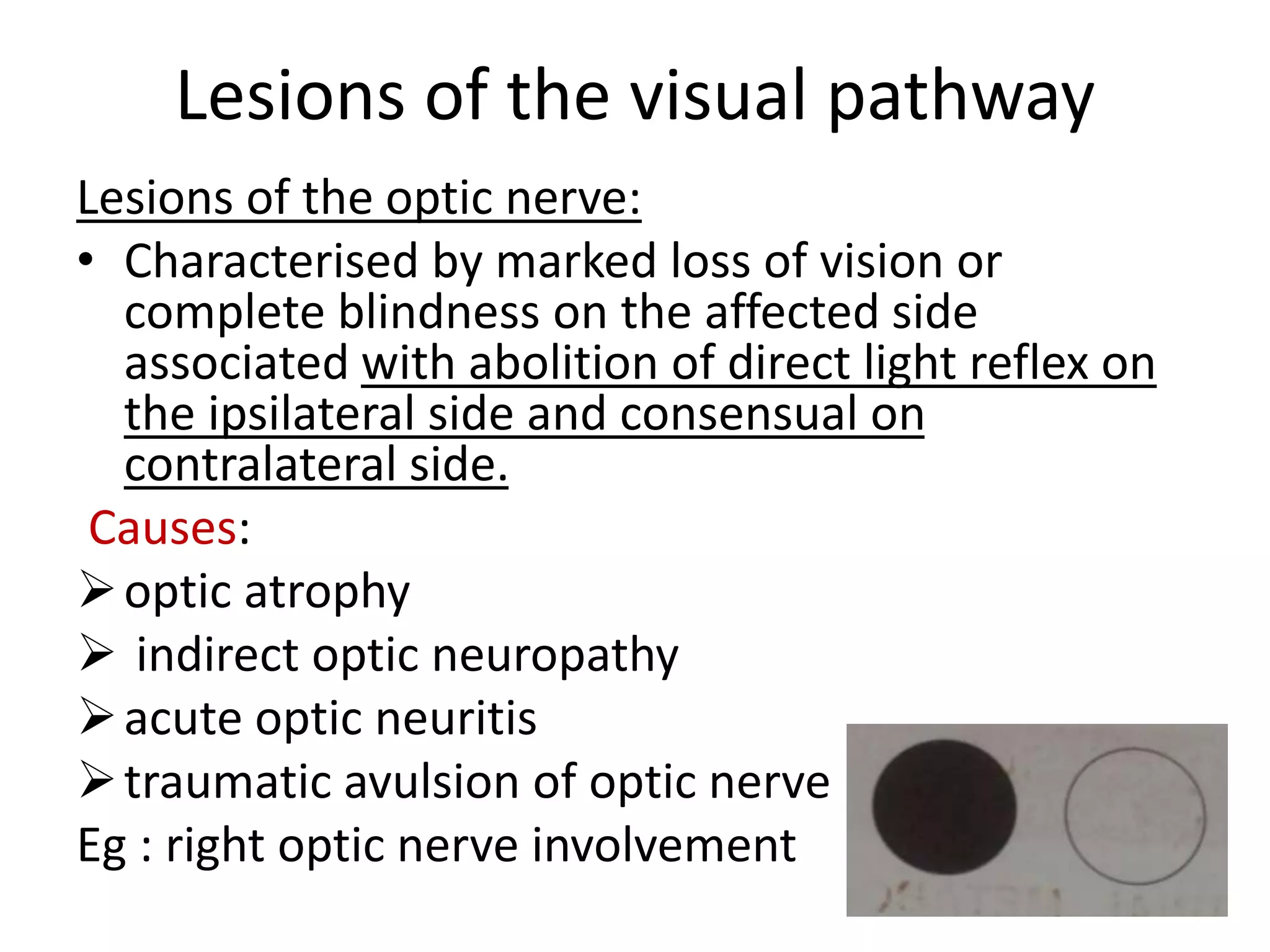
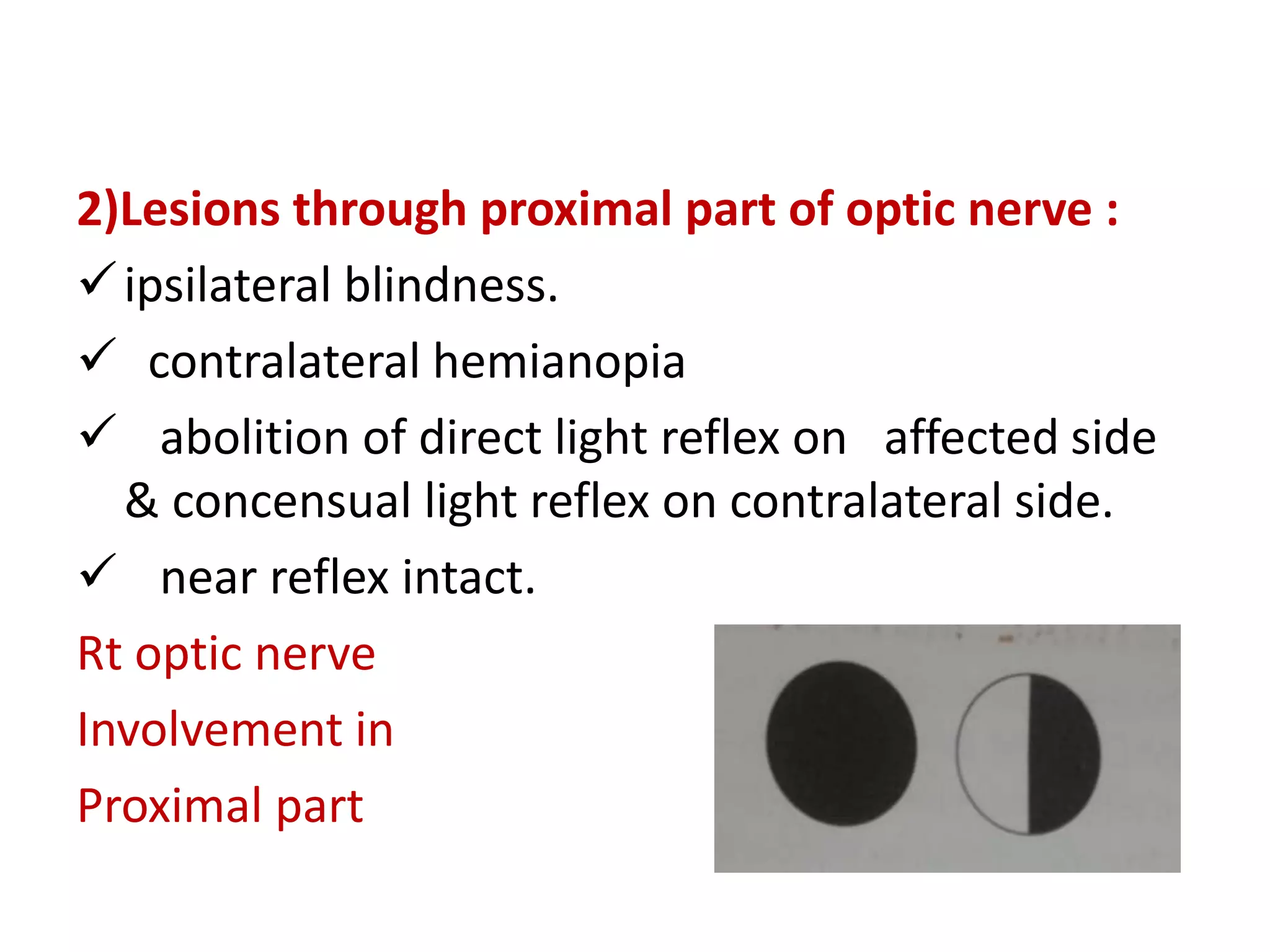
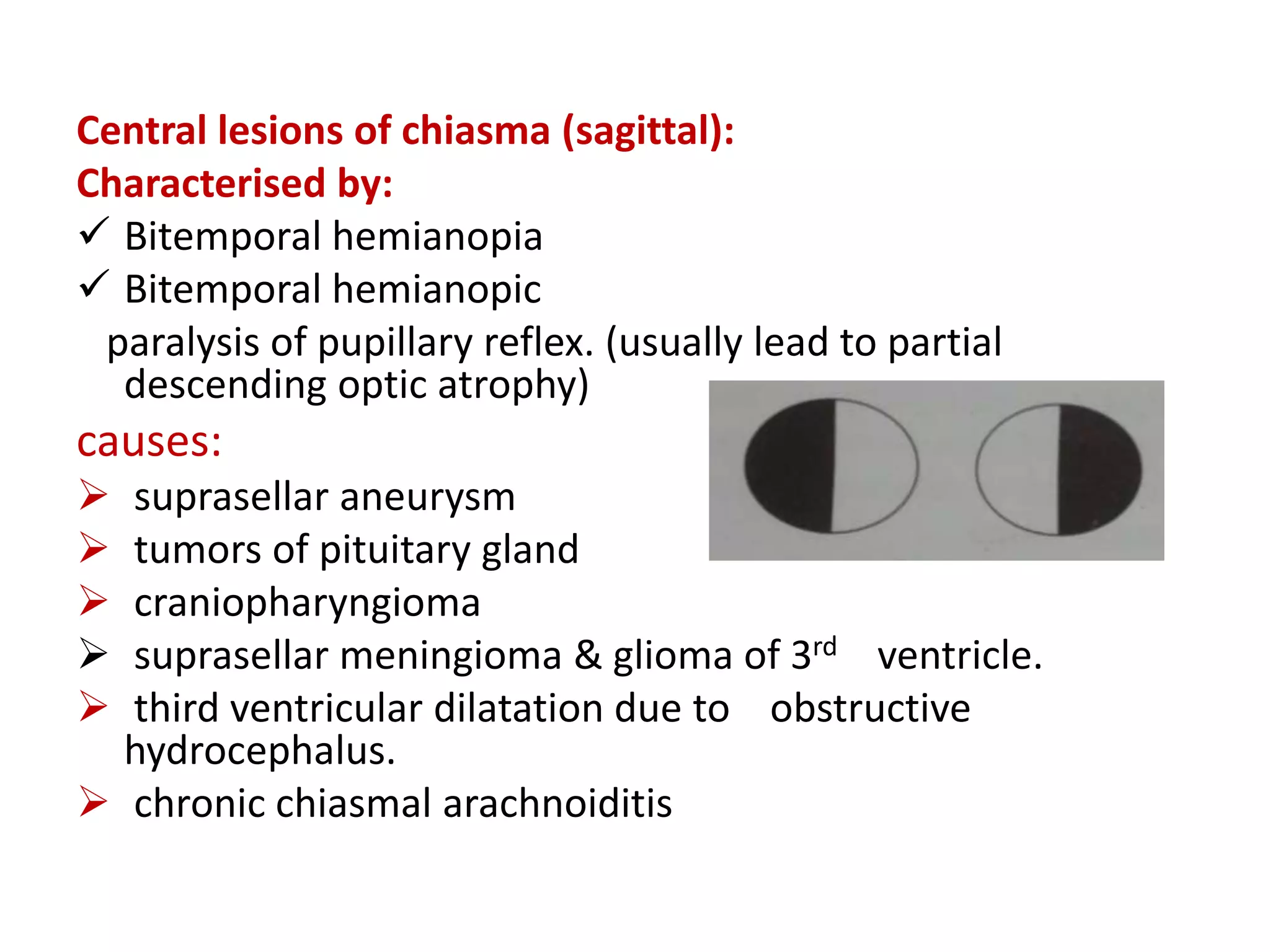
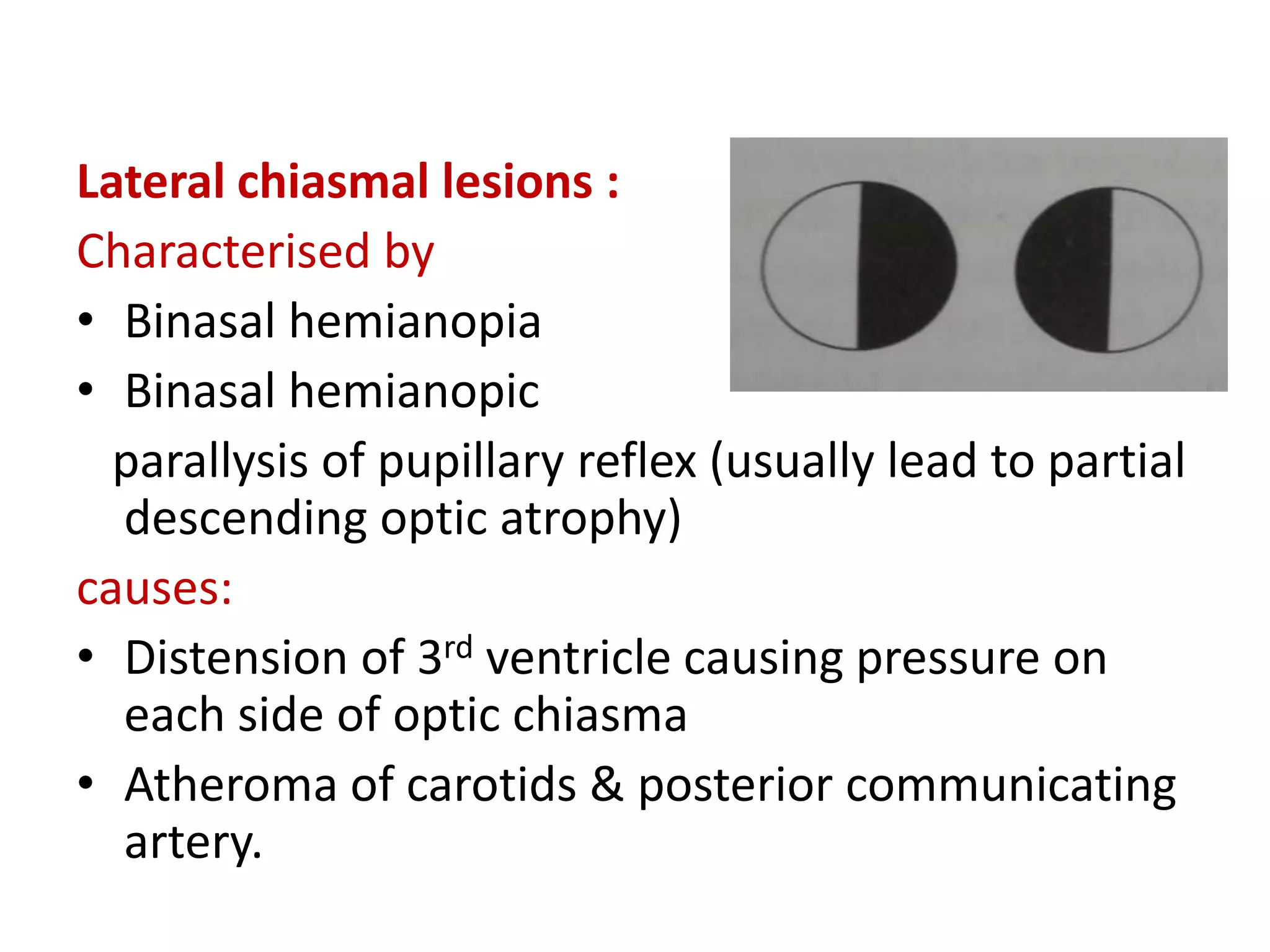
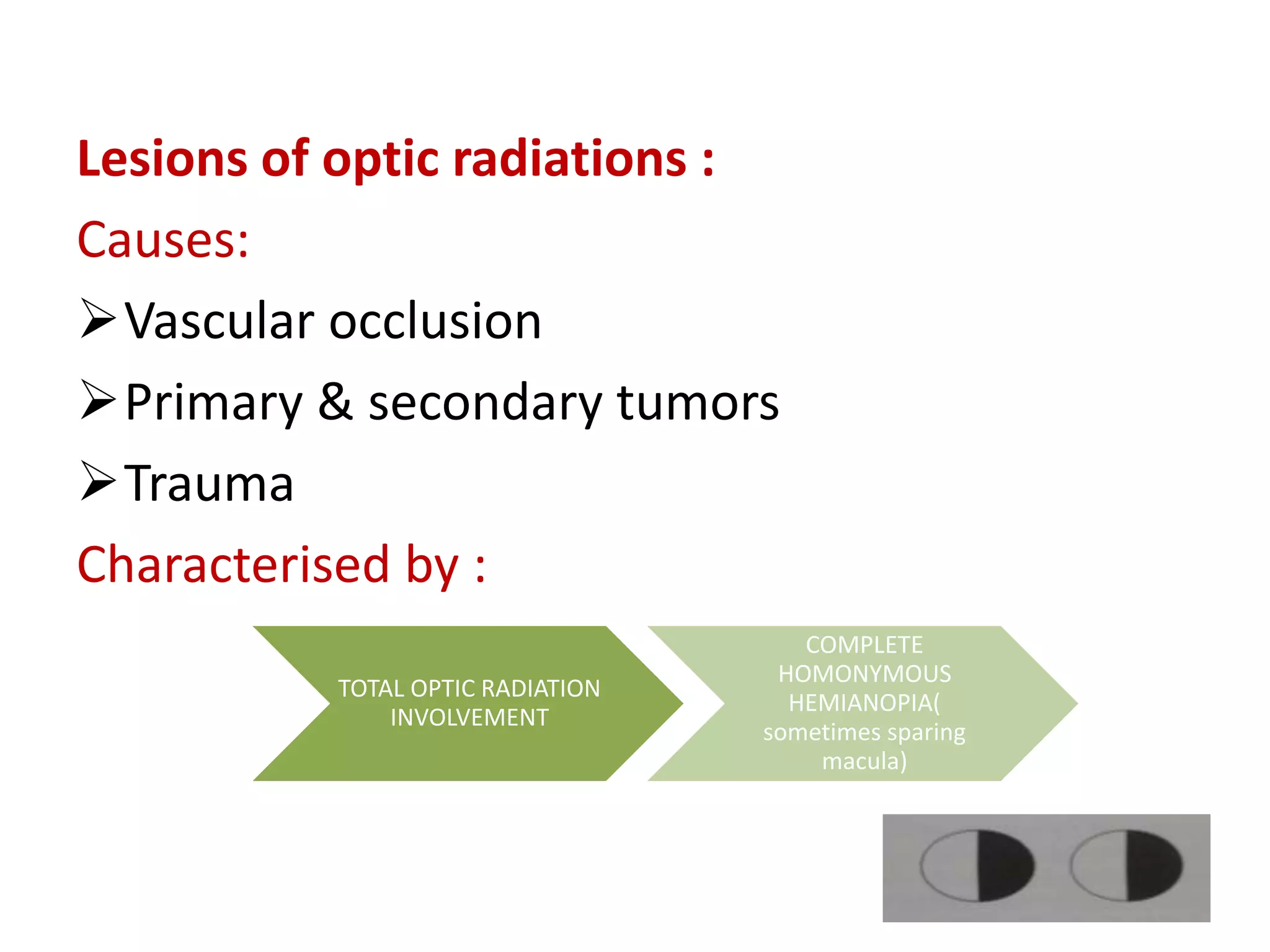
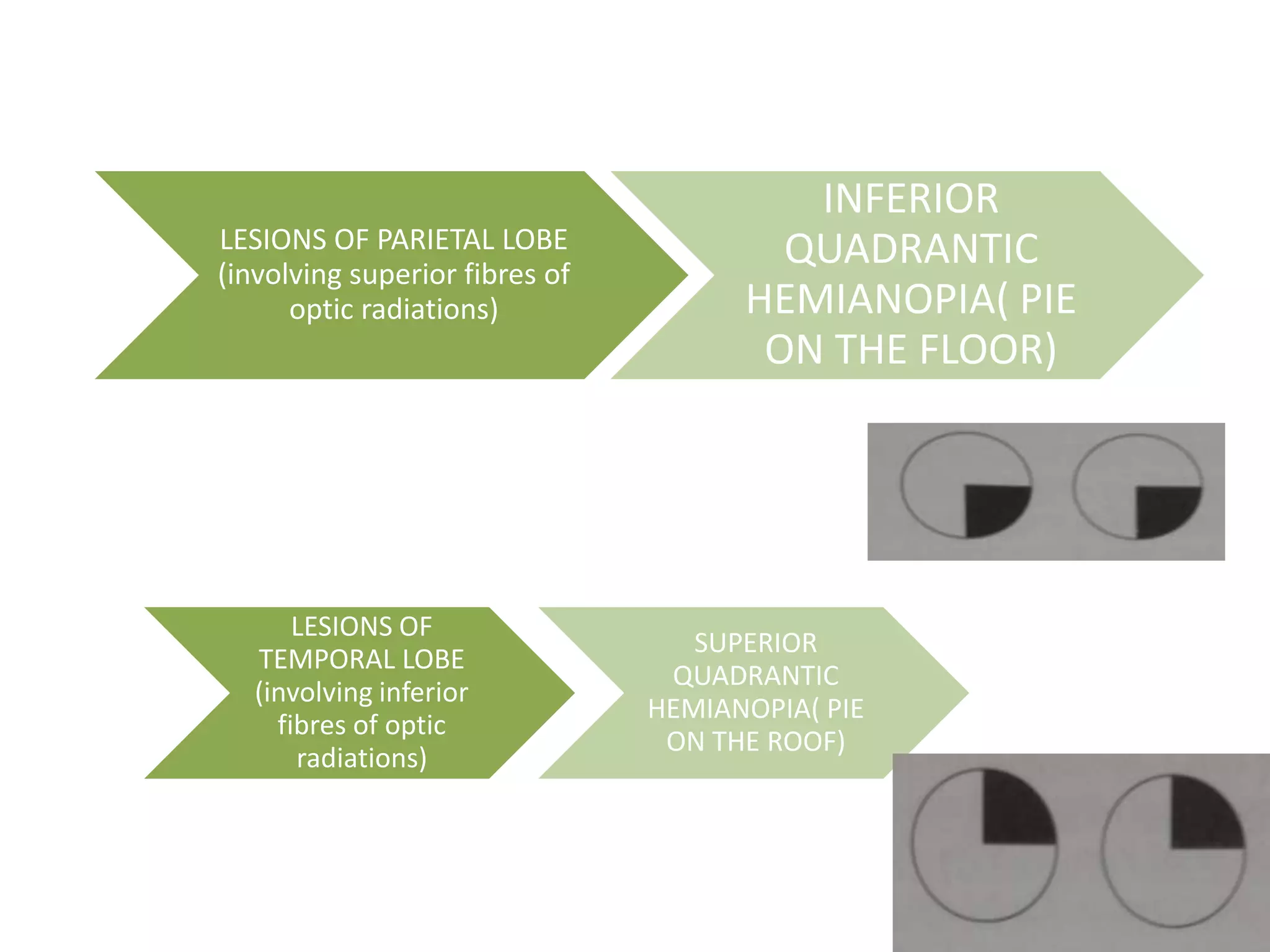
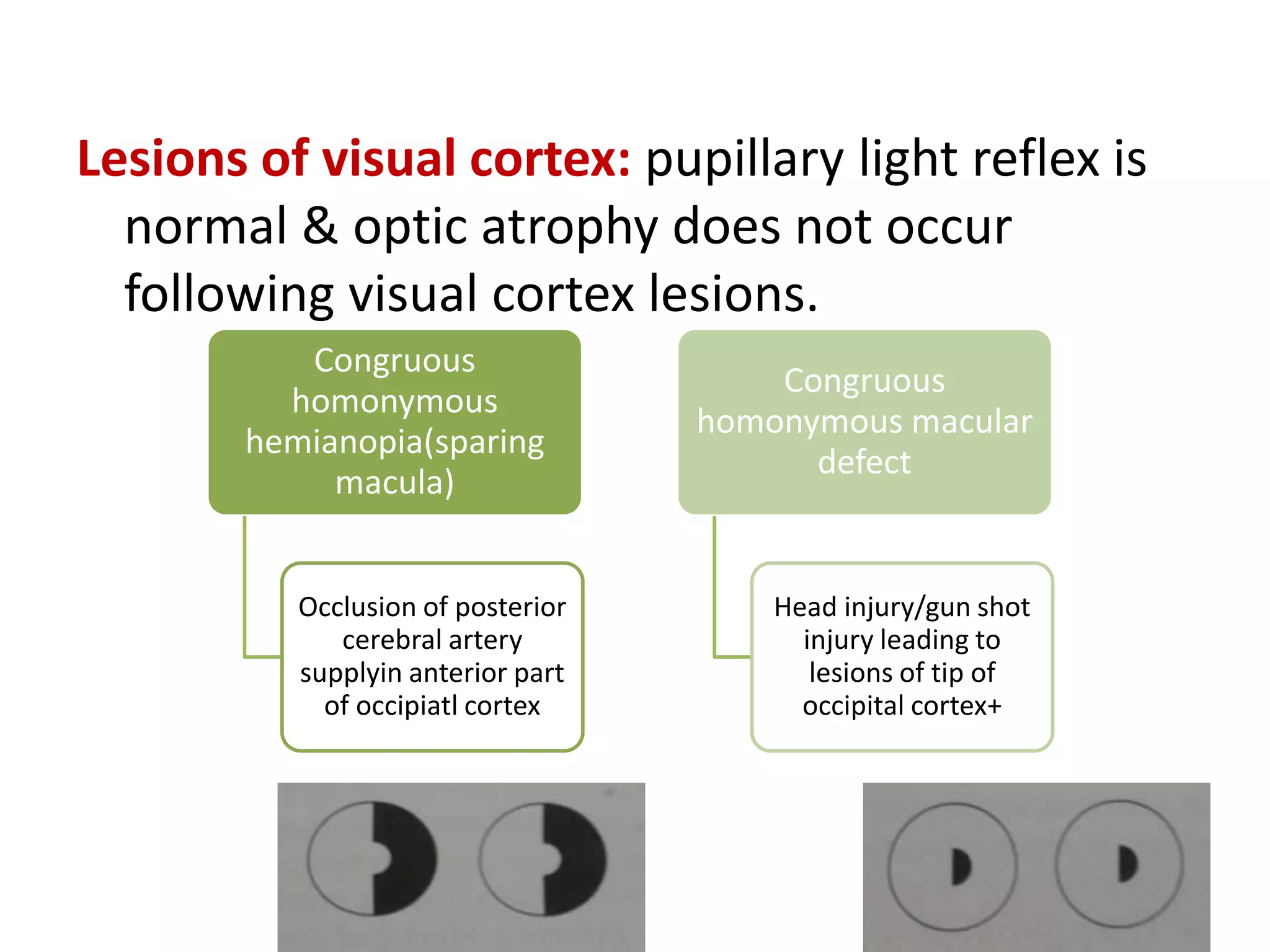
2. Lesions in different parts of the visual pathway cause specific visual field defects such as hemianopia. For example, a lesion in the optic chiasm causes bitemporal hemianopia.
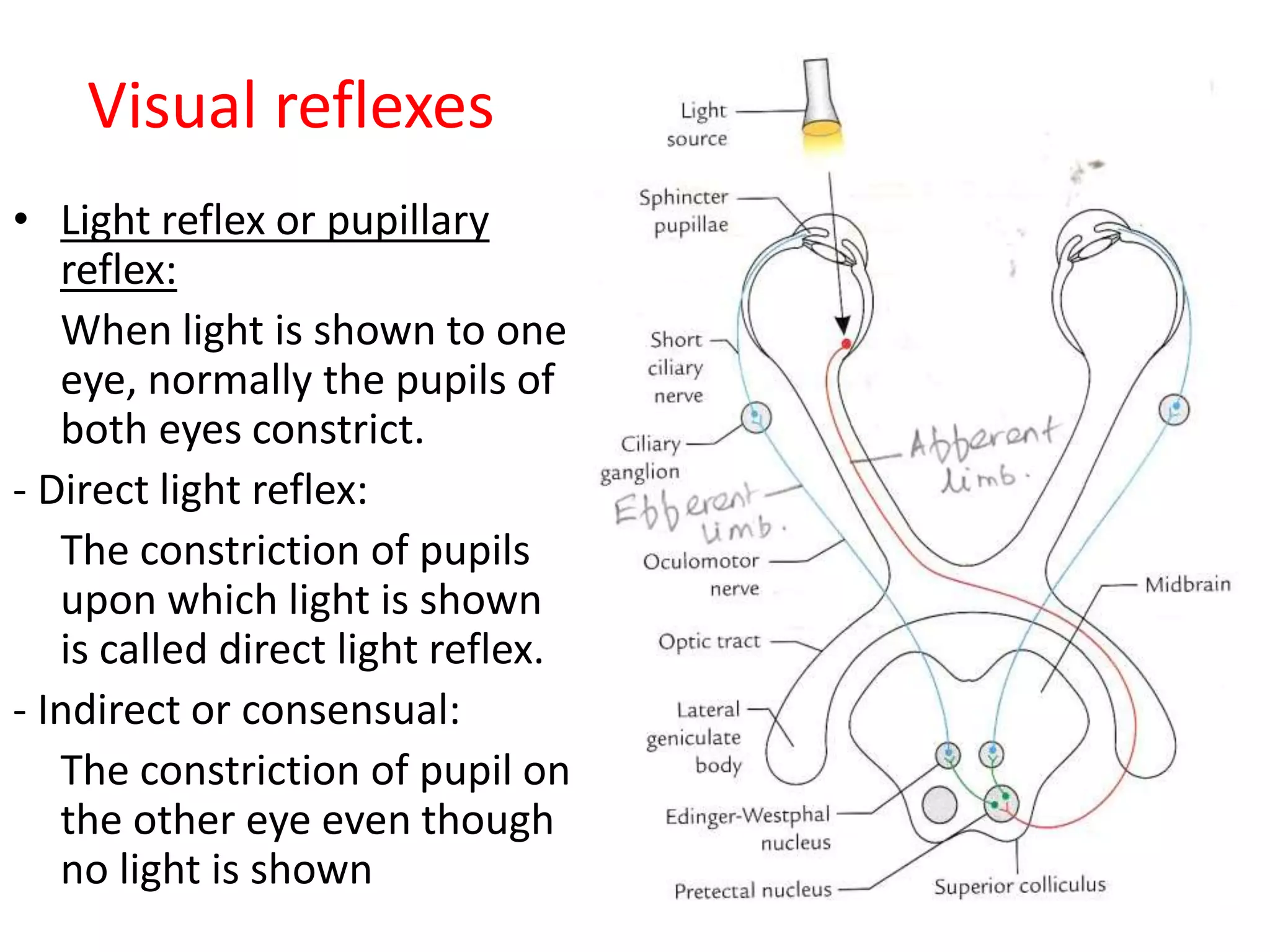
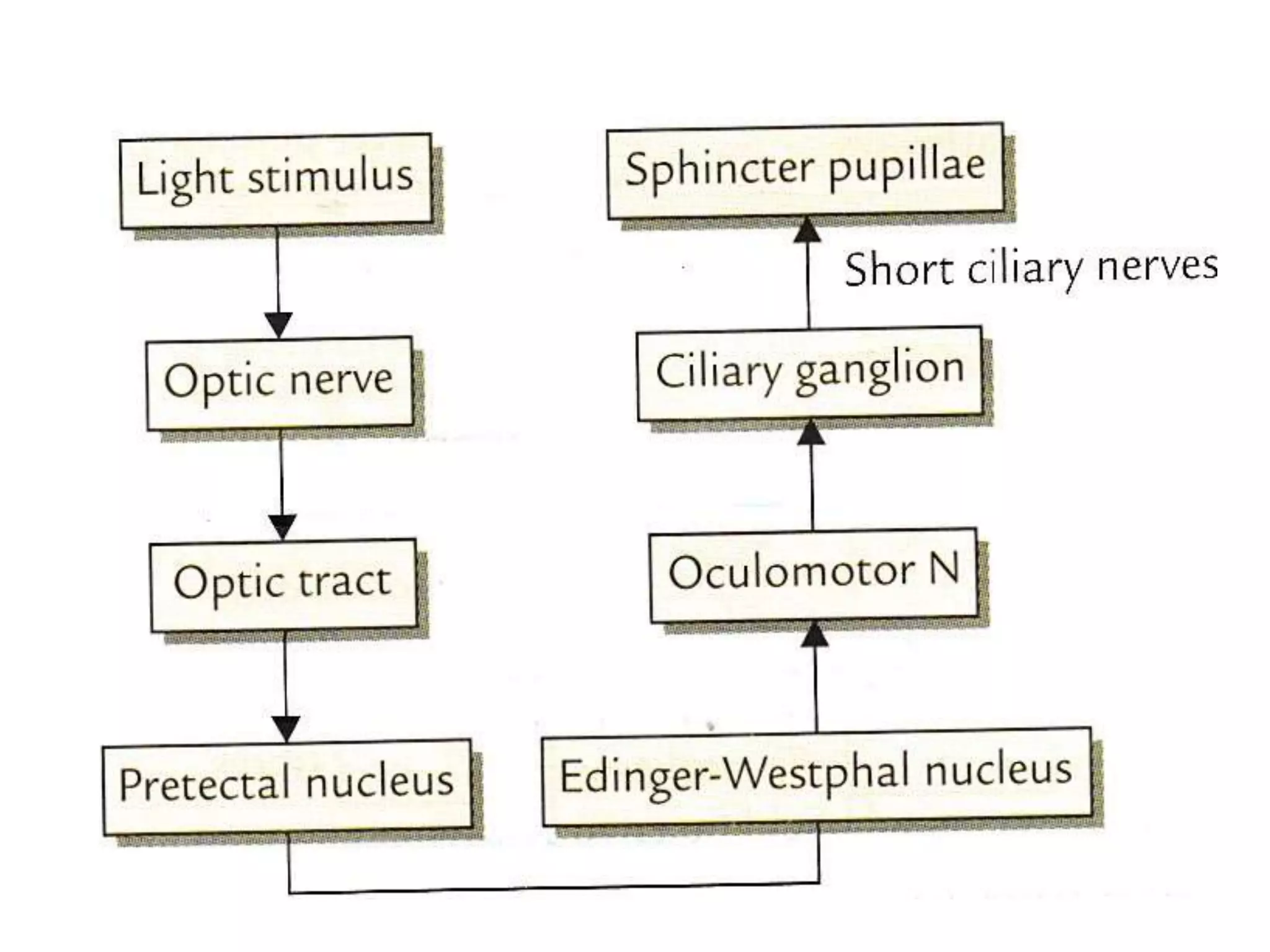
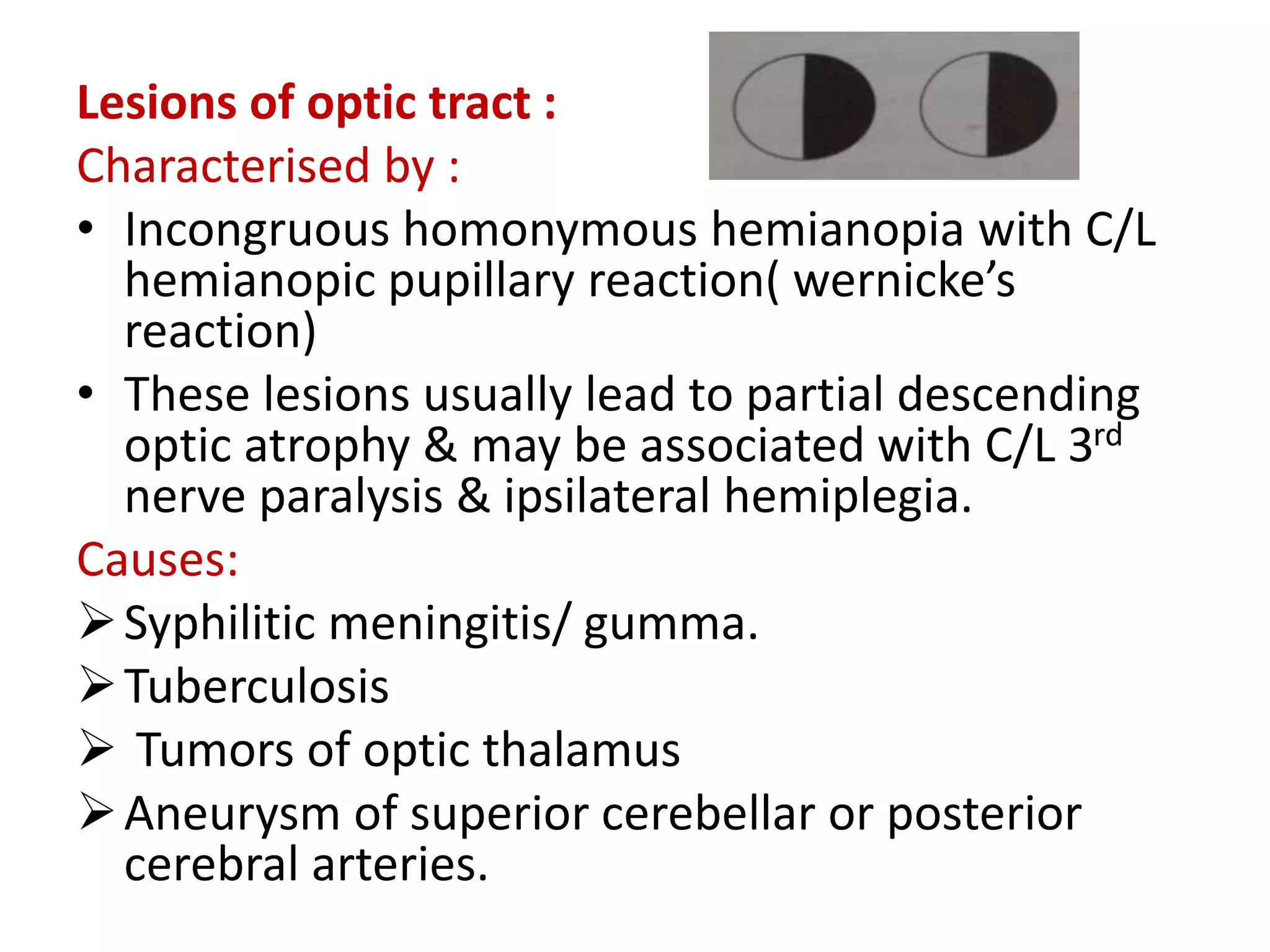
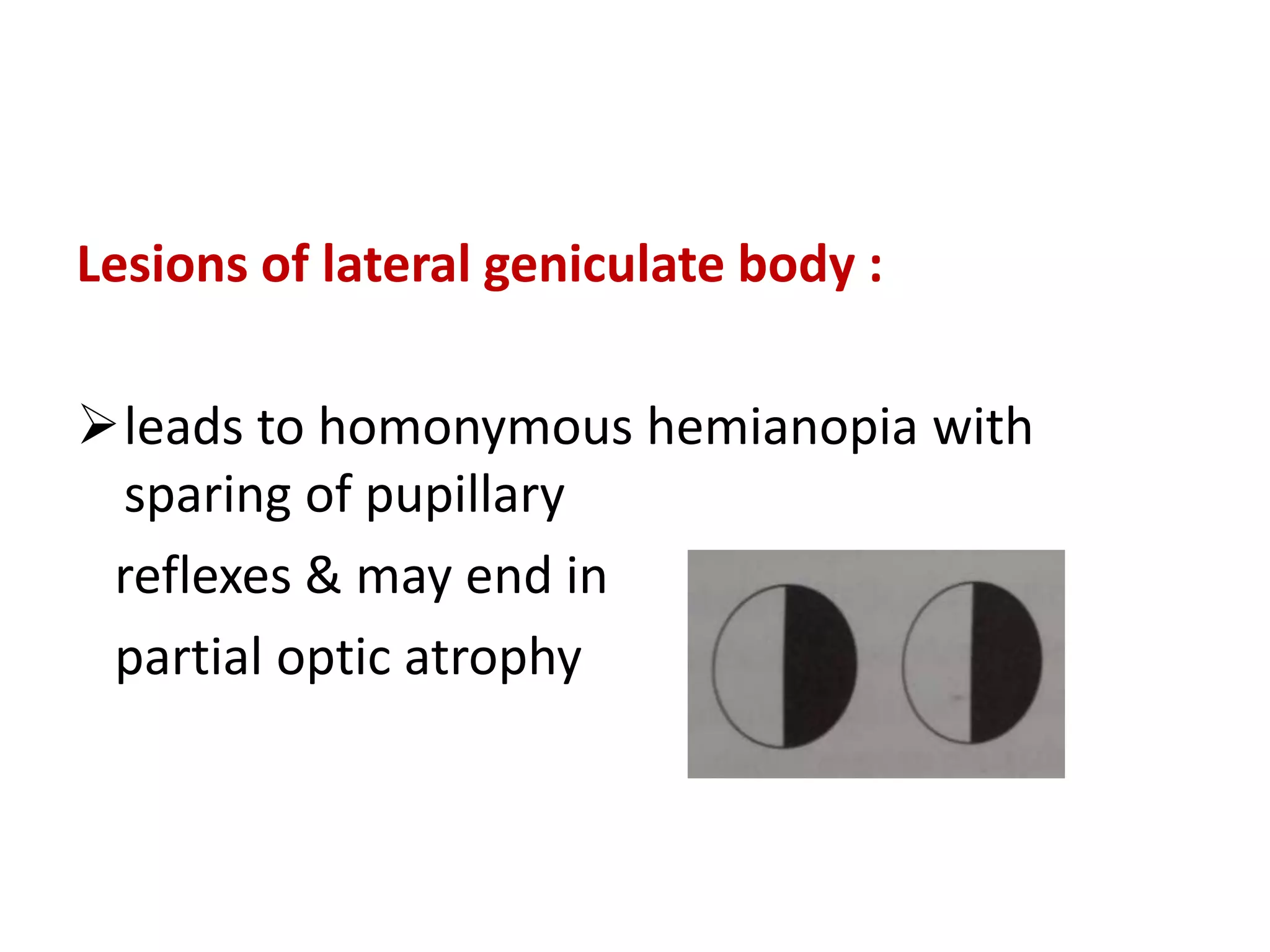
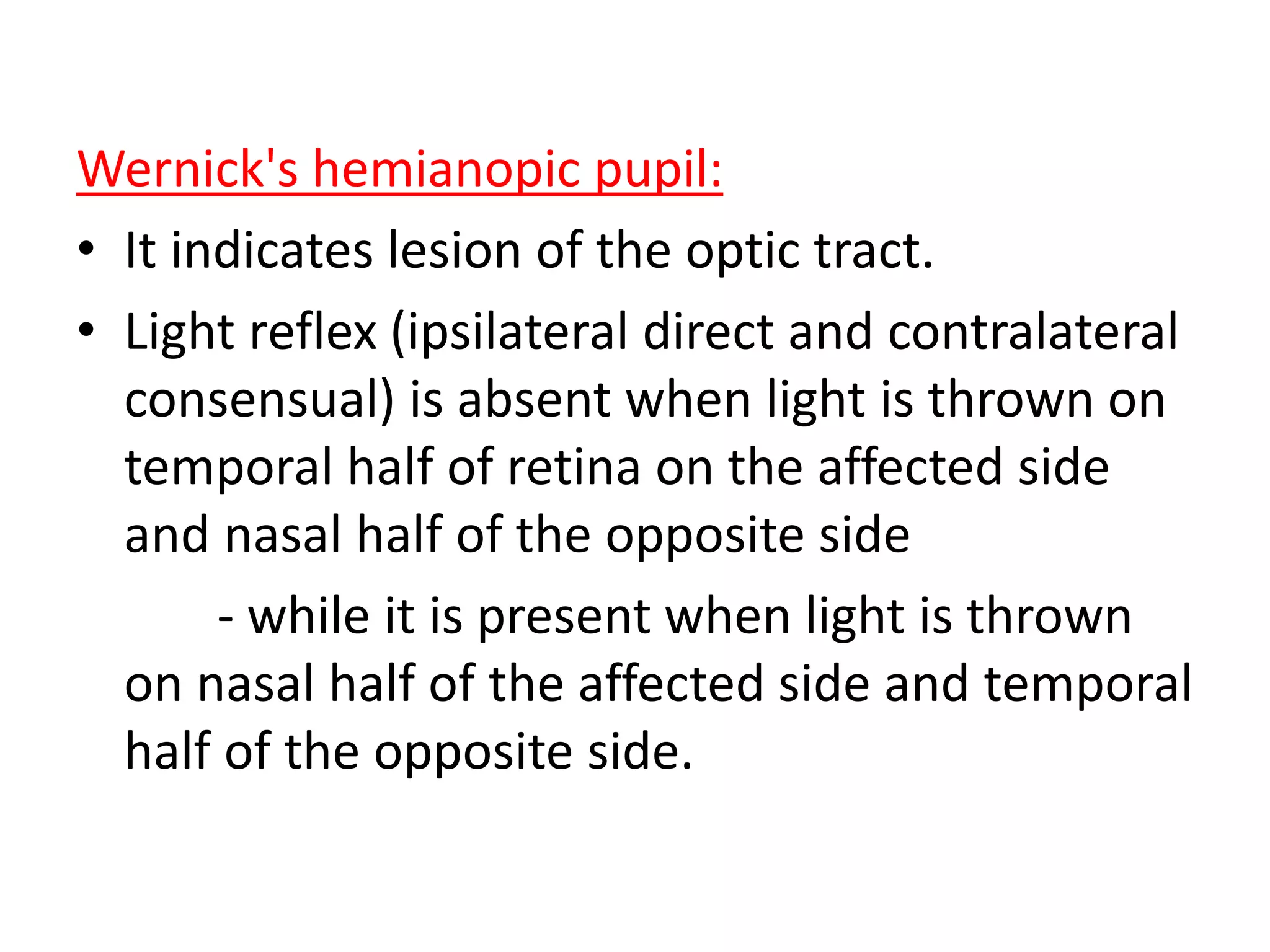
3. Pupillary reflexes can localize lesions, such as Wernicke's hemianopic pupil indicating an optic tract lesion.