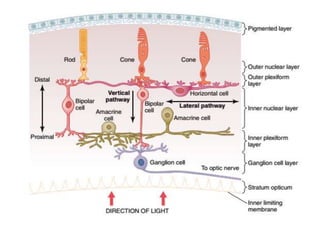
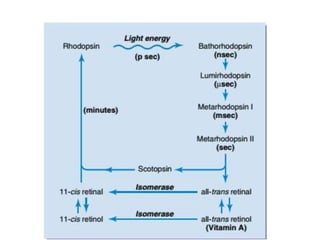
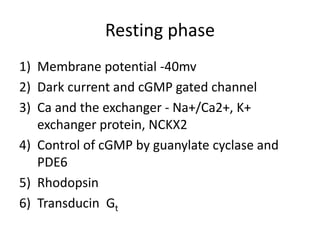
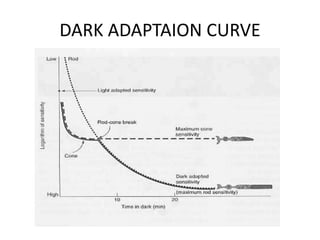
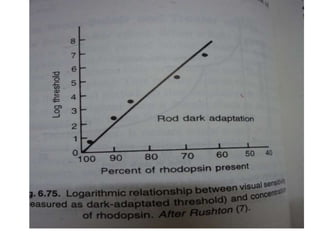
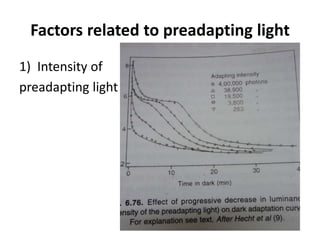
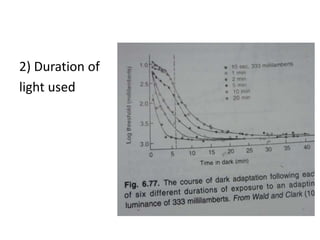
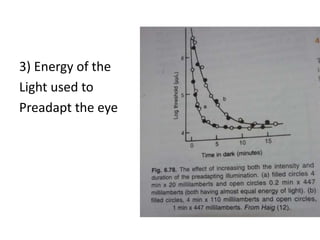
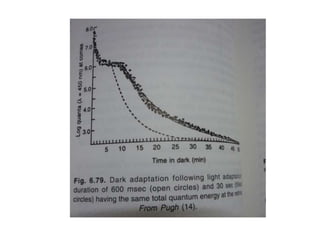
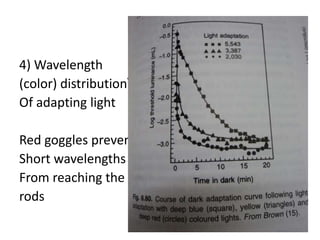
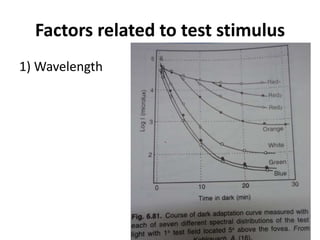
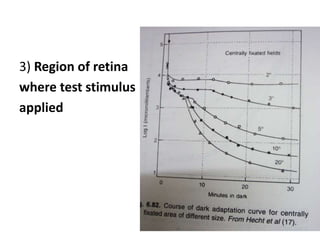
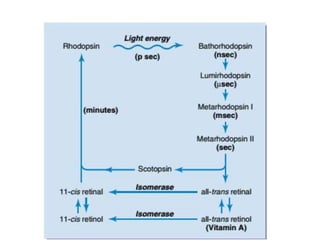
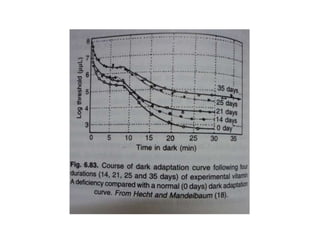
This document discusses dark adaptation, which is the ability of the eye to adapt to decreasing levels of illumination. It describes the mechanisms and factors that affect dark adaptation. The mechanisms involve restoration of visual pigments in rods and cones as well as neural and pupillary adaptations. Factors that influence dark adaptation include characteristics of the pre-adapting light, test stimulus used, and individual differences such as vitamin A levels, ocular diseases, and genetic disorders that impact night vision. Several genetic disorders that impact dark adaptation are also discussed such as congenital stationary night blindness and Stargardt's disease.