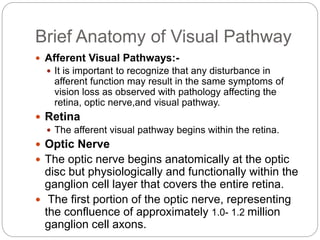
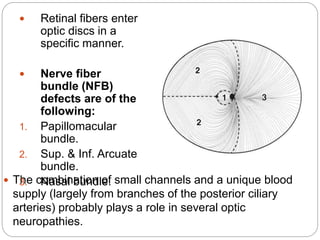
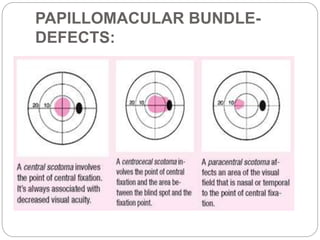
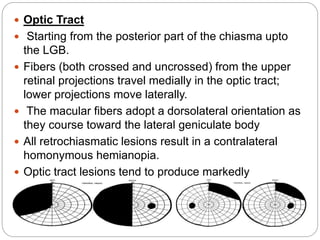
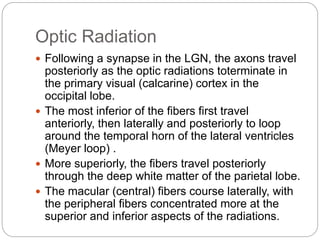
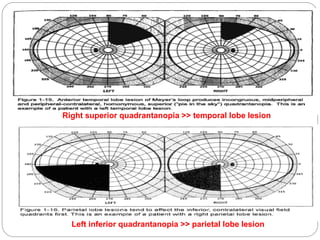
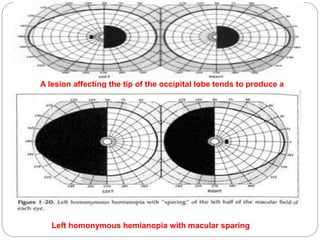
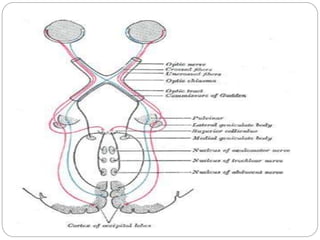
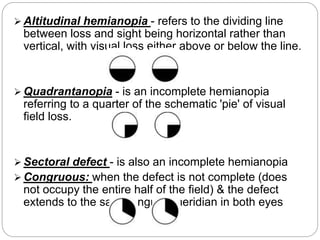
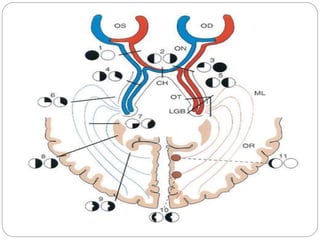
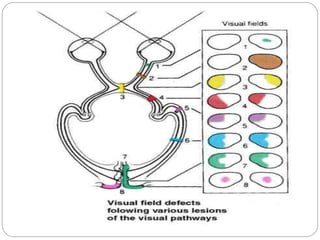
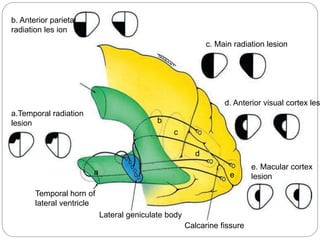
The visual pathway begins in the retina and passes through the optic nerve, optic chiasm, optic tract, lateral geniculate nucleus, optic radiation, and visual cortex before terminating in the occipital lobe. Lesions in different parts of the visual pathway can cause different visual field defects, such as hemianopia or quadrantanopia. The more posterior the lesion, the more likely the visual field defects will be congruous between the two eyes.