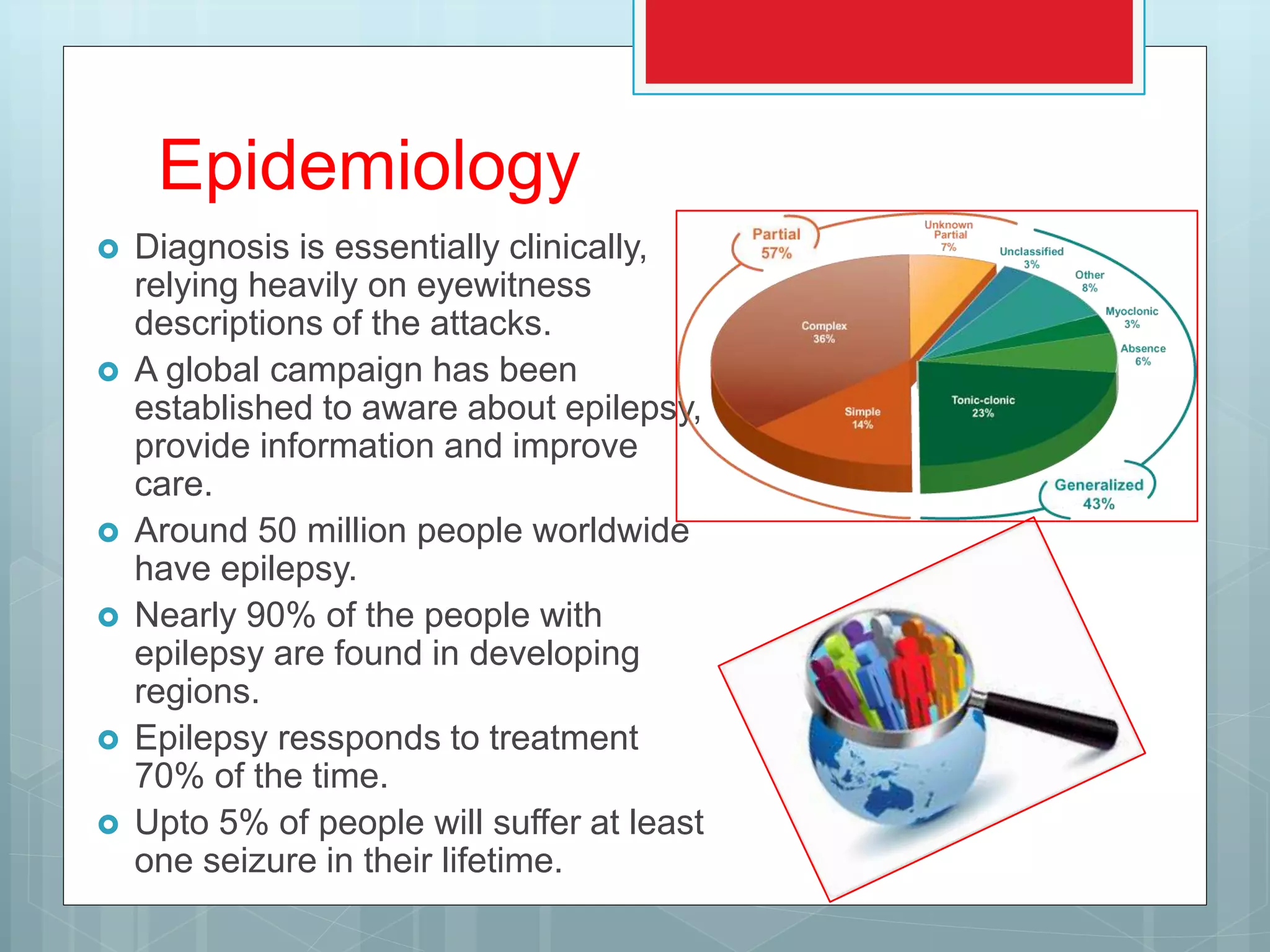
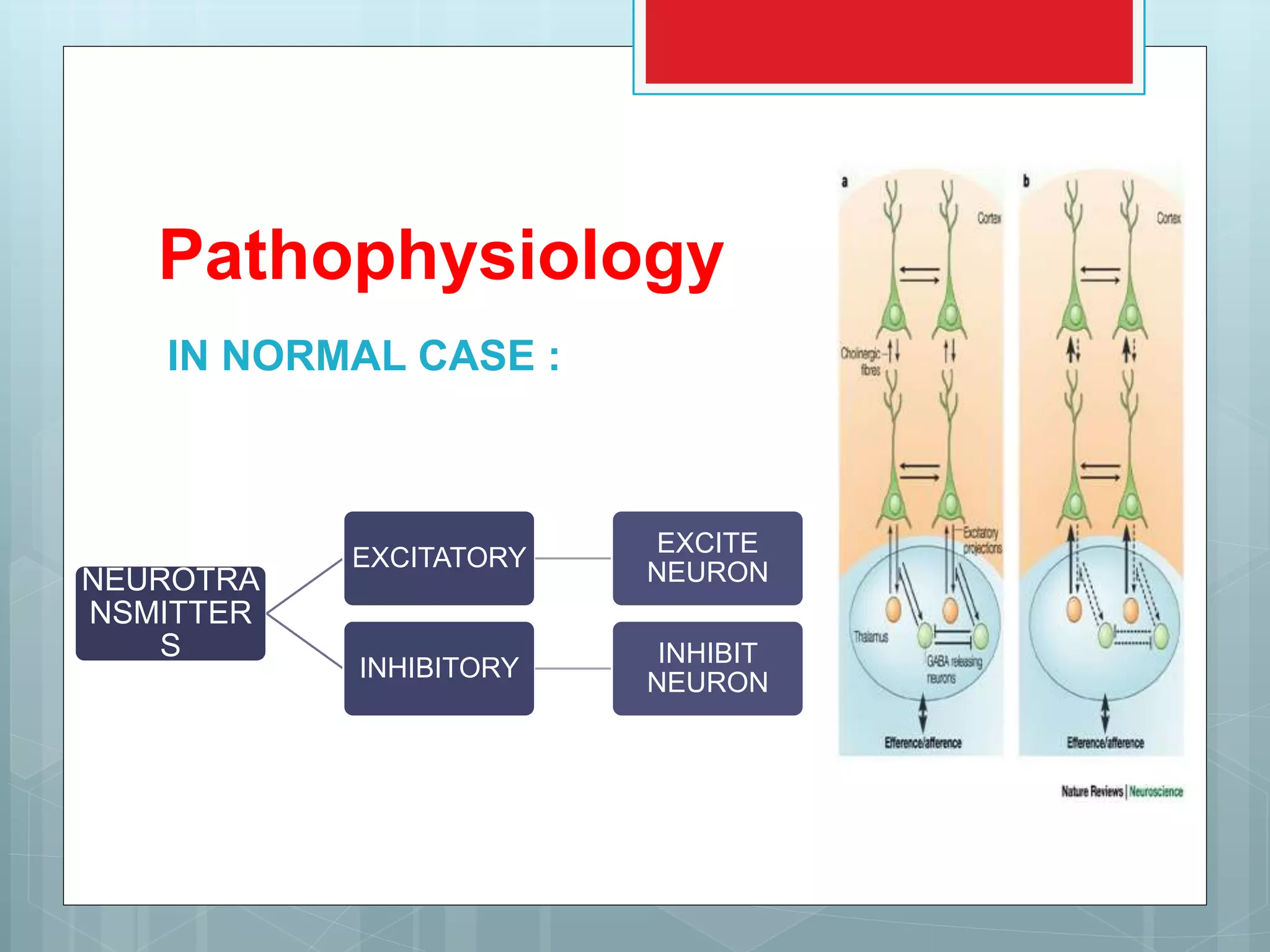
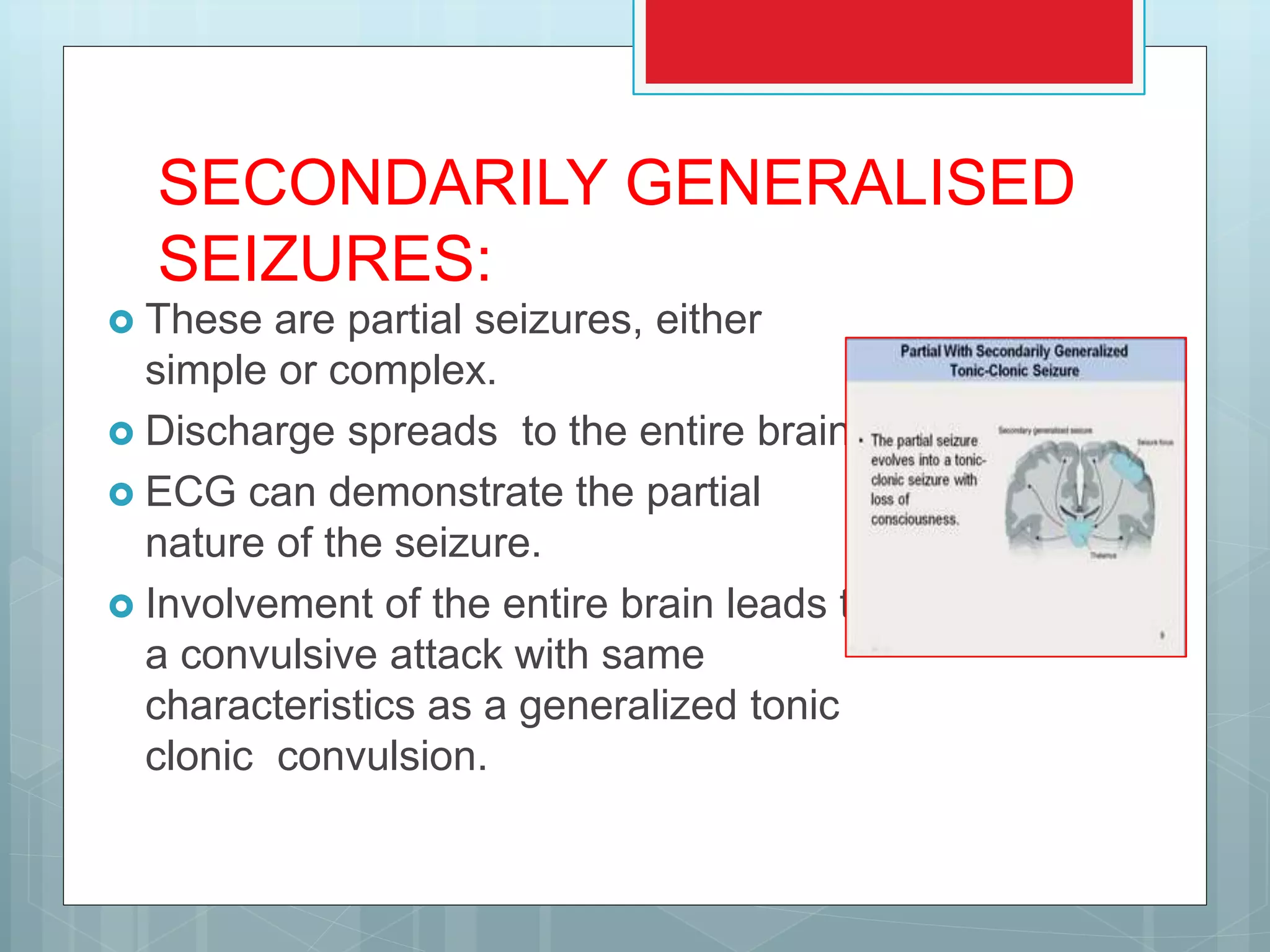
The document discusses epilepsy, a neurological disorder characterized by recurrent seizures due to abnormal neuronal discharges. It outlines the epidemiology, aetiology, types of seizures, diagnosis, treatment options, and various antiepileptic drugs available, emphasizing individualized treatment based on seizure type and patient needs. It also addresses management during seizures, long-term treatment strategies, and drug withdrawal protocols.