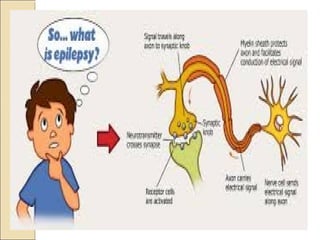
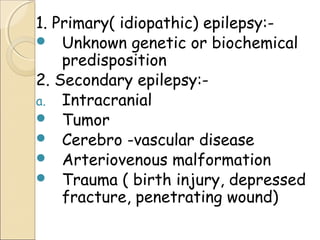
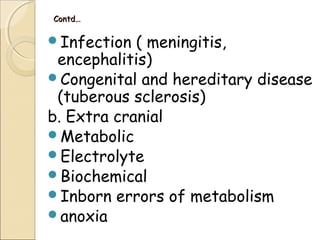
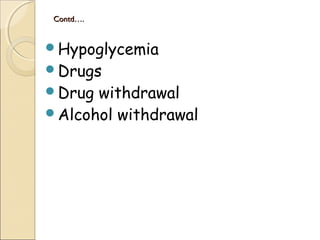
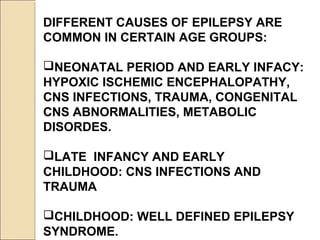
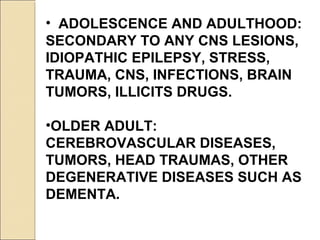
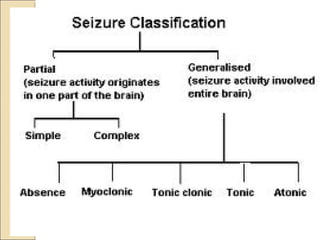
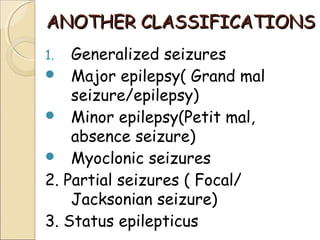
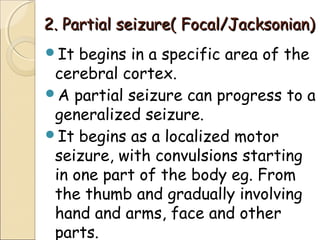
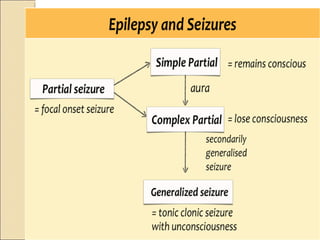
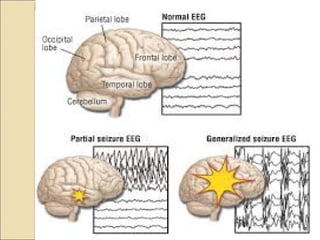
Epilepsy is a disorder caused by abnormal electrical activity in the brain that causes seizures. Seizures occur when groups of nerve cells, or neurons, in the brain send out abnormal burst of electrical activity. The main types of seizures are generalized seizures, which involve the whole brain, and partial seizures, which originate in one area of the brain. Epilepsy has many potential causes including genetic factors, brain injury, infections, tumors, and metabolic imbalances. Treatment involves medications to control seizures and lifestyle modifications to prevent injury during seizures.