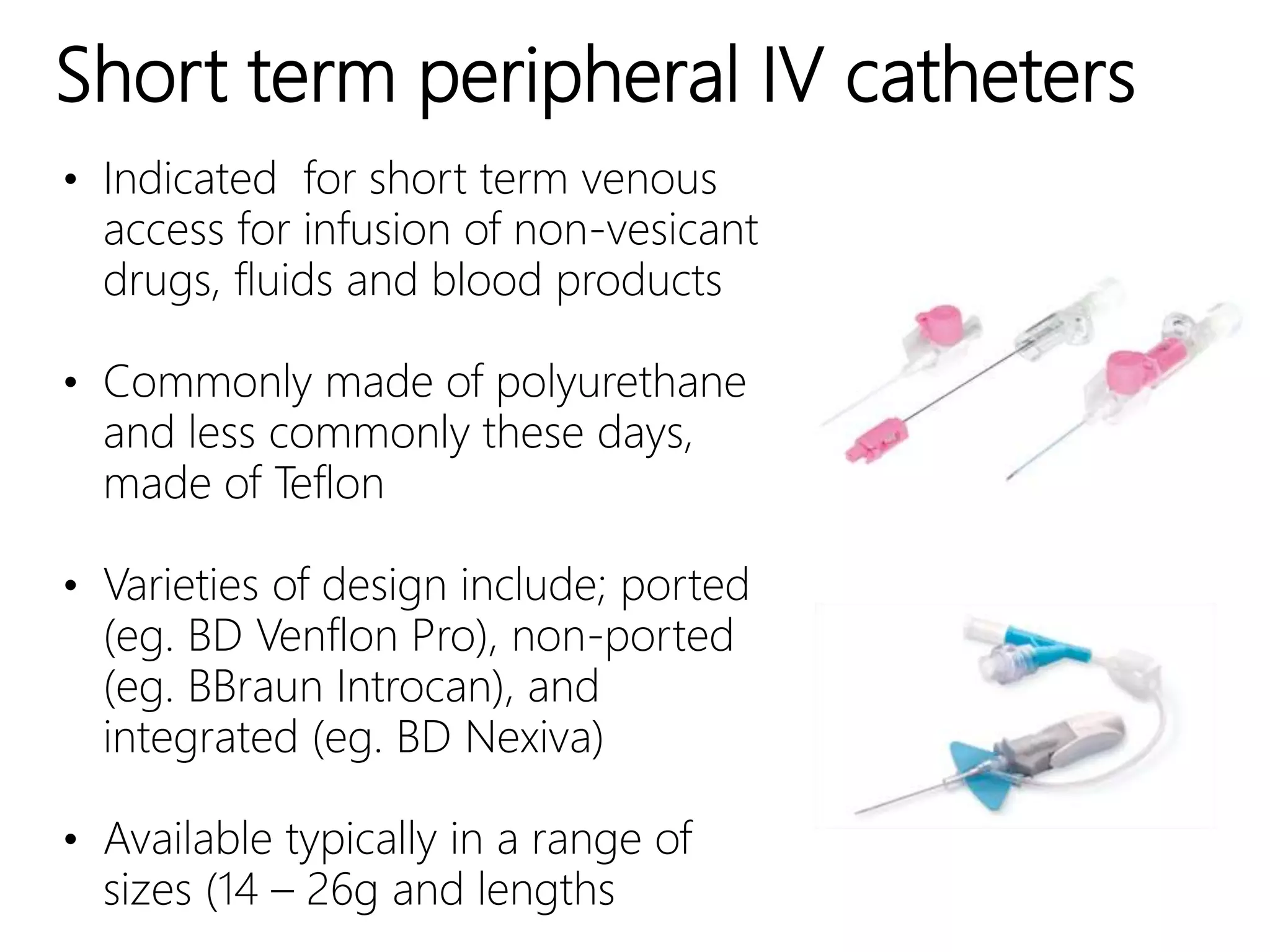
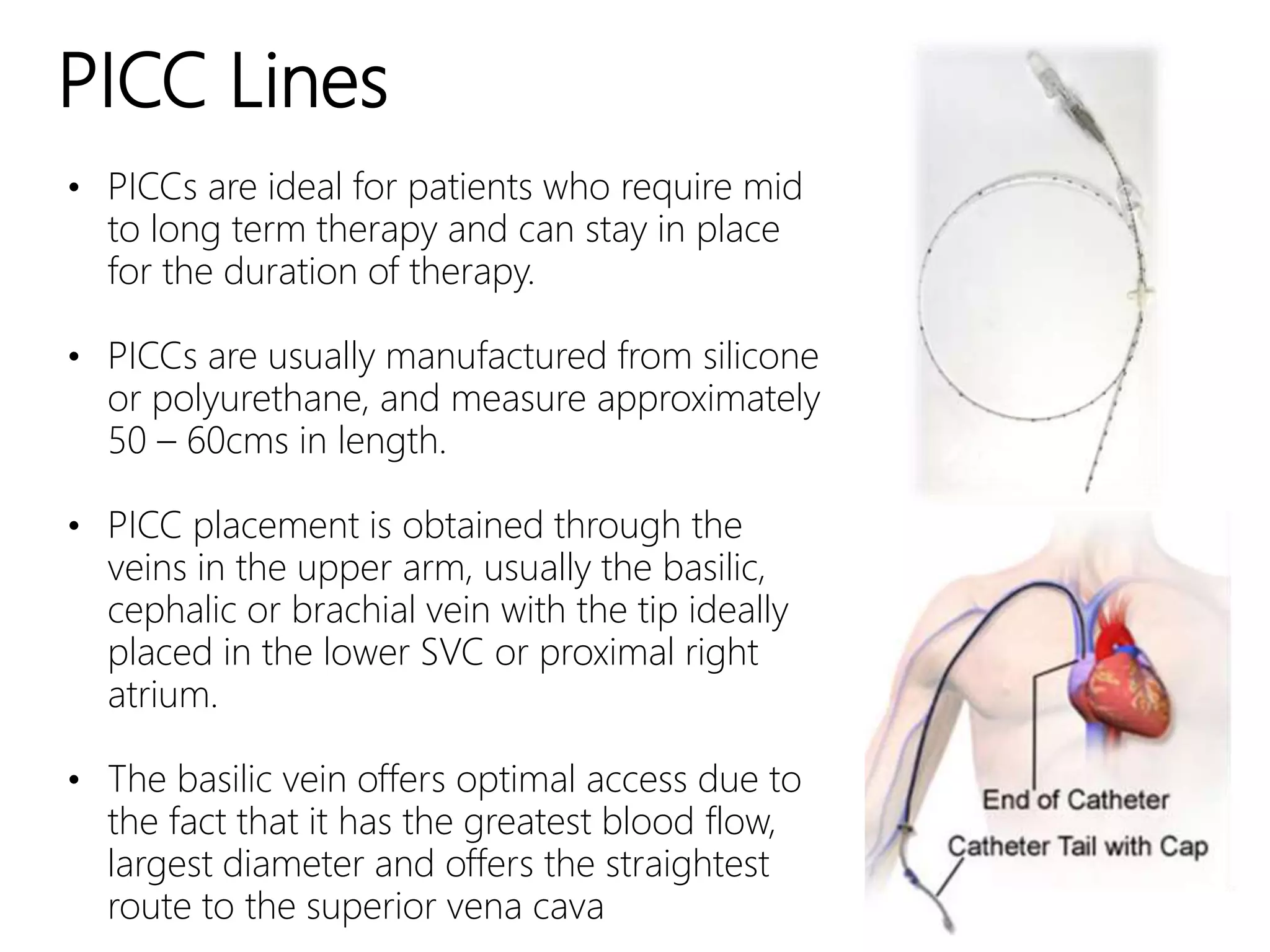
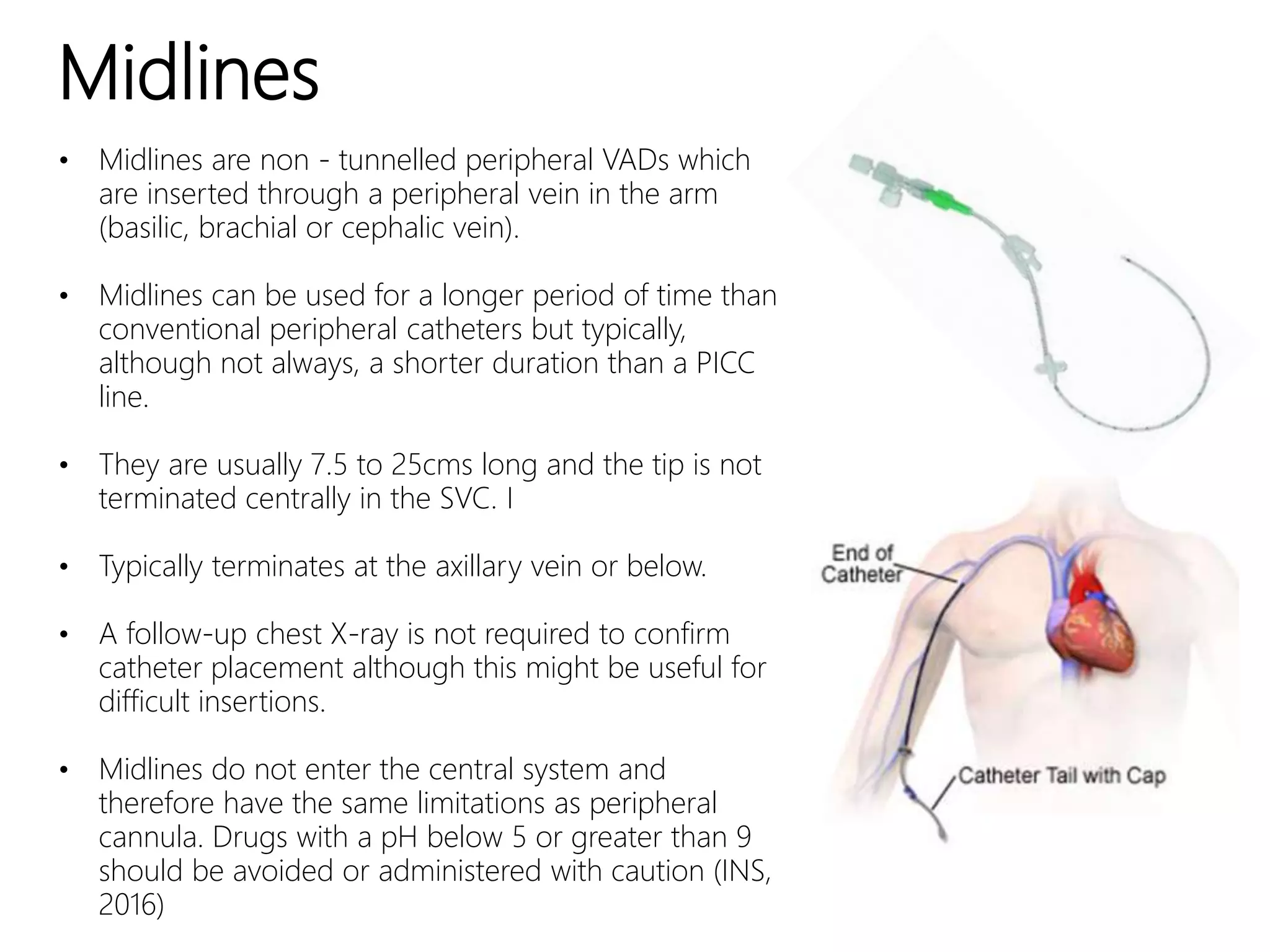
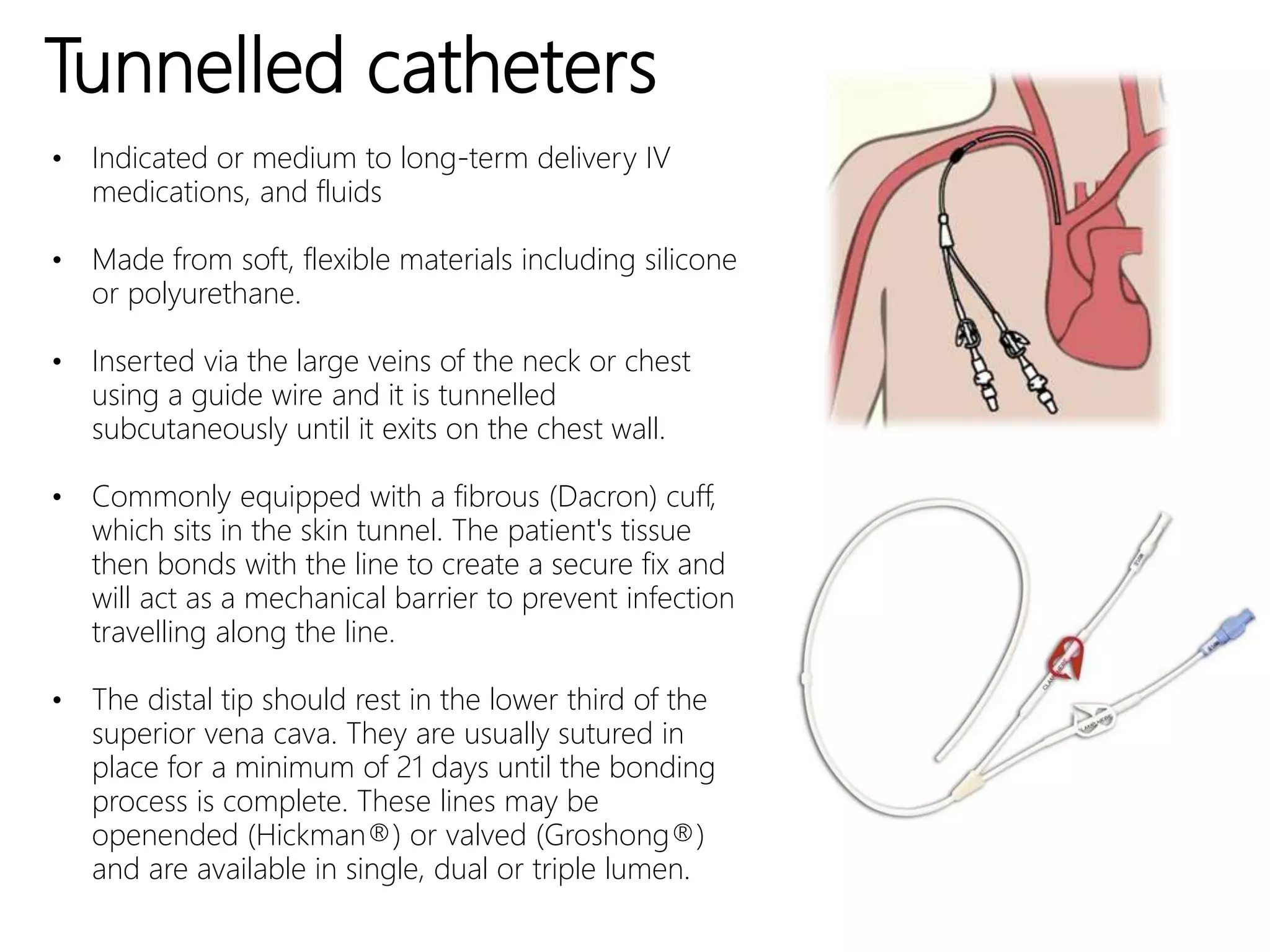
This document discusses various types of venous access devices, including their indications, considerations, and characteristics. Short-term peripheral IV catheters are indicated for infusion of non-vesicant drugs, fluids, and blood products. PICCs are ideal for mid- to long-term therapy and can stay in place for the duration of therapy. Midlines can be used for a longer period than conventional peripheral catheters but shorter than PICCs, terminating below the axillary vein. Non-tunnelled central venous catheters are used for short-term access and infusion of vesicant medications or fluids. Implantable ports are typically indicated for extended IV therapy and preferred by patients concerned about body image. Tunnel