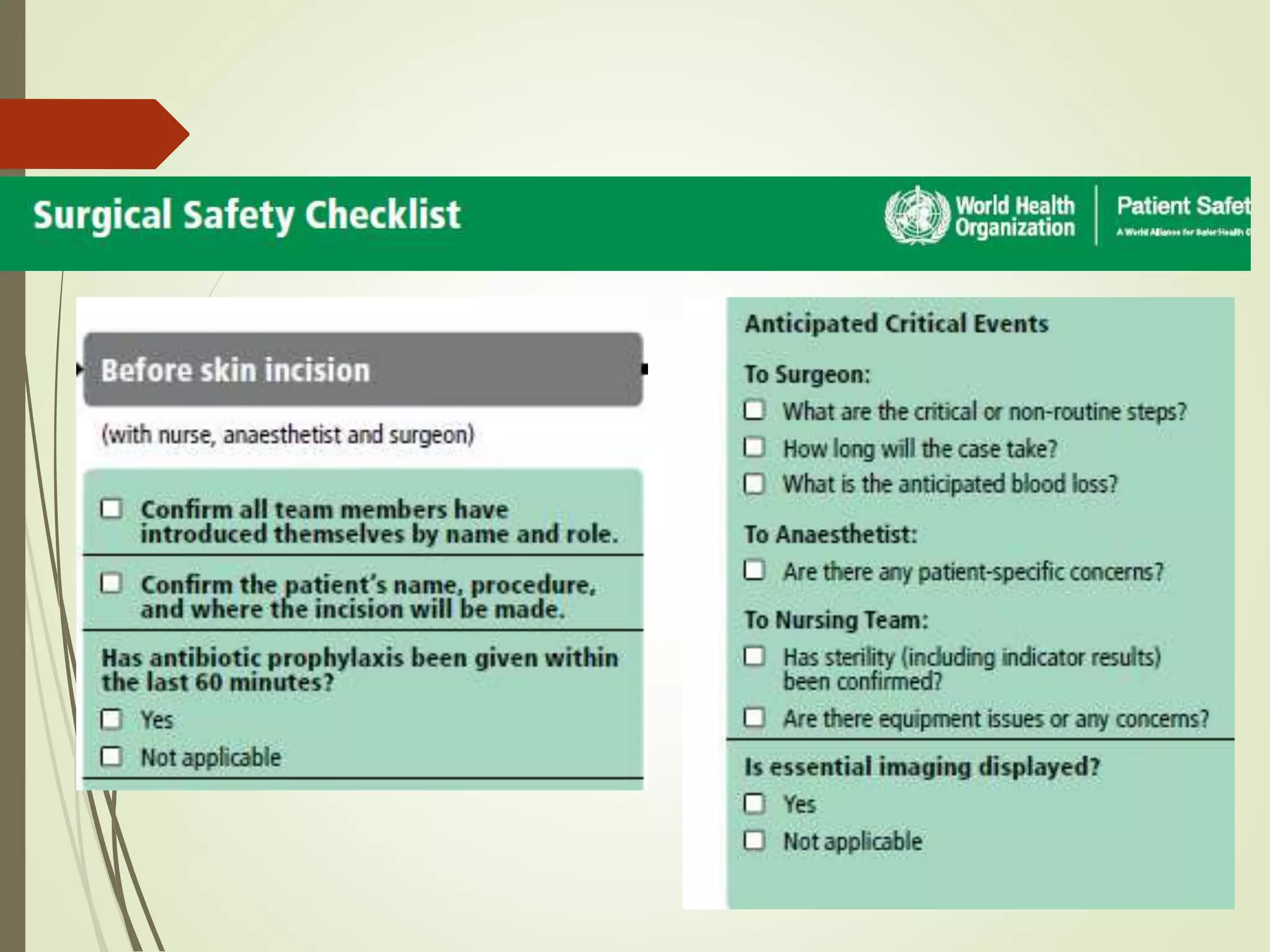
The document discusses the surgical safety checklist recommended by the World Health Organization (WHO). It was created to improve communication among surgical teams and reduce avoidable complications and deaths associated with surgery. The checklist is intended to be used at three critical times: before anesthesia, before incision, and before the patient leaves the operating room. It contains steps to confirm the correct patient, prevent errors, and ensure key safety practices are followed. Studies have found the checklist significantly improves surgical outcomes when properly implemented.