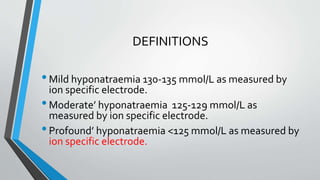
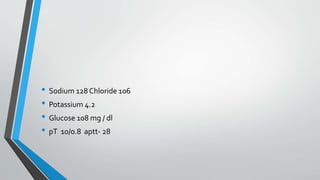
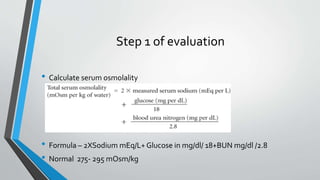
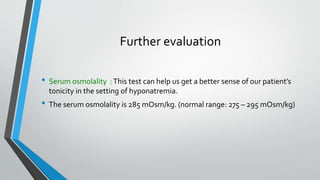
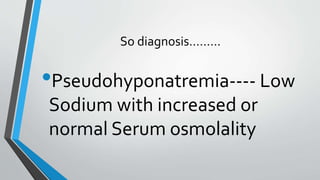
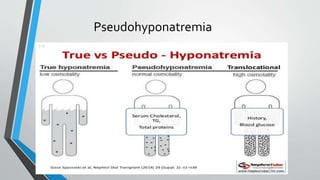
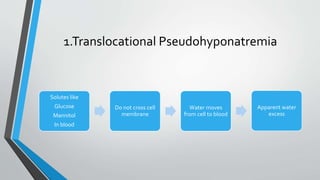
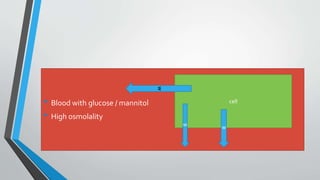
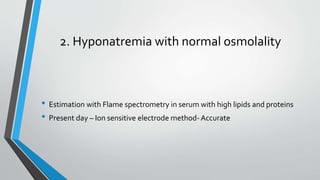
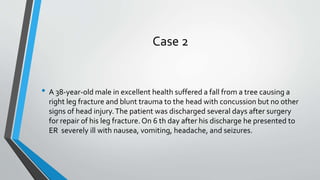
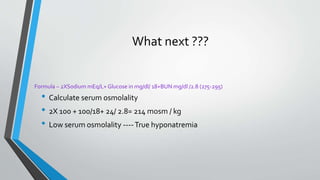
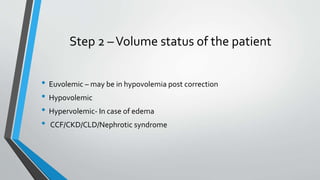
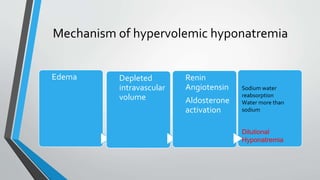
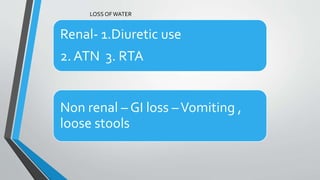
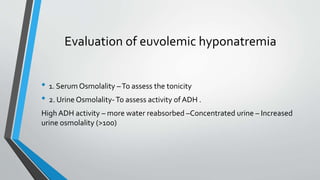
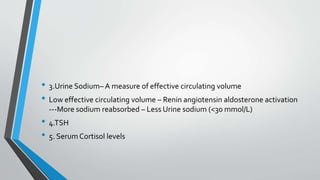
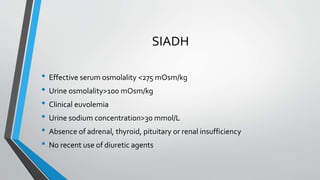
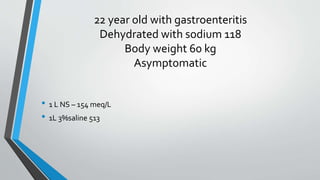
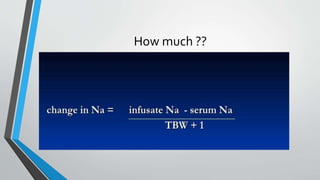
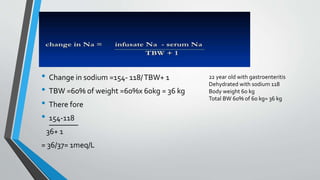
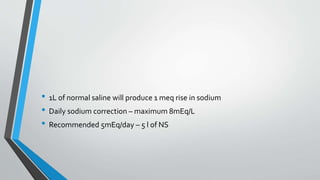
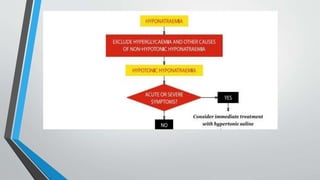
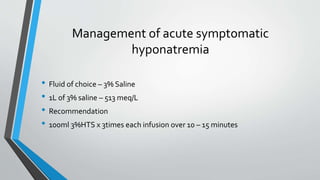
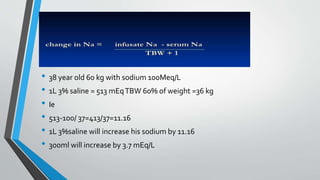
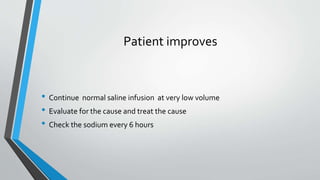
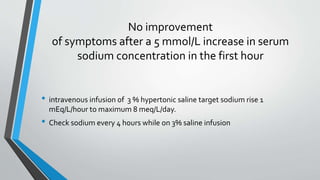
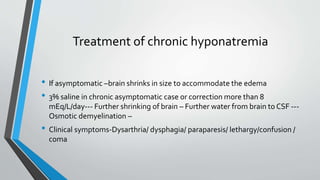
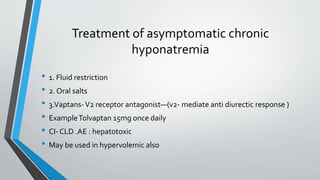
This document discusses hyponatremia, including definitions, causes, symptoms, evaluation and treatment. It defines hyponatremia as a serum sodium concentration <135 mmol/L. Evaluation involves assessing volume status, serum and urine osmolality and sodium levels. Causes include SIADH, hypothyroidism and medications. Treatment depends on severity and chronicity of hyponatremia and involves fluid restriction, oral salts or vaptans. Acute severe hyponatremia is treated with intravenous 3% saline while chronic asymptomatic hyponatremia can be managed with fluid restriction and oral salts.