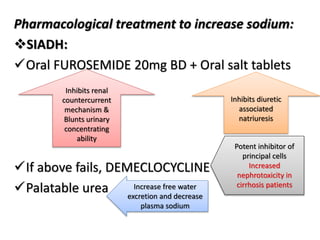
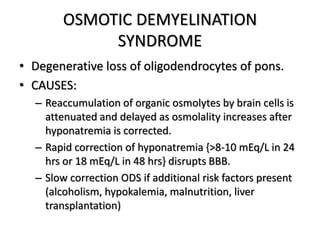
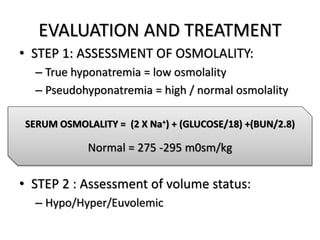
The document presents an overview of hyponatremia, discussing its causes, types, clinical features, and management strategies. It emphasizes the physiological mechanisms affecting sodium concentration and provides treatment guidelines for acute and chronic hyponatremia, including specific medications and correction rates. Key points highlight the risks associated with rapid correction and complications such as osmotic demyelination syndrome.






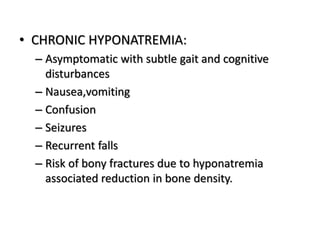




![• Chronic euvolemic hyponatremia (post 48hrs)
– If symptomatic similar management as acute one.
– If stable or mild neurological symptoms water restriction
based on
>1 = <500ml/day
~1 = 500-700 ml/day
>1 = <1L/day
o If corrected with 3%NaCl, central pontine myelinosis/osmotic
demyelination syndrome occurs due further shrinkage of brain.
Associated hypokalemia correction tends to overcorrect
sodium.
increase in dietary solute intake: oral salt tablets,
palatable urea
Urine-to-plasma electrolyte ratio={Urine [Na+]+[K+]} / Plasma [Na+]](https://image.slidesharecdn.com/hyponatremia092229-230824165905-f463a249/85/HYPONATREMIA-pptx-17-320.jpg)