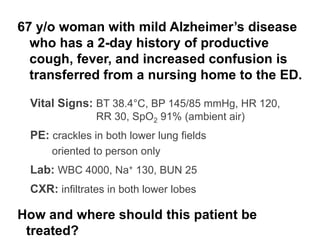
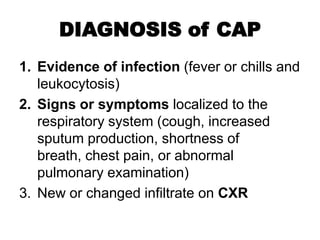
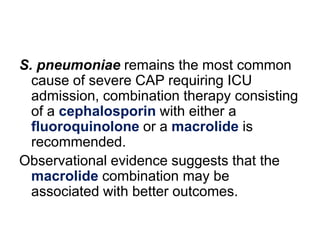
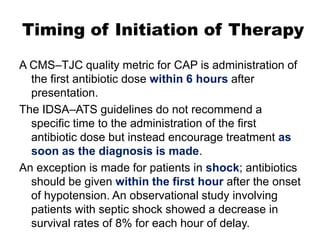
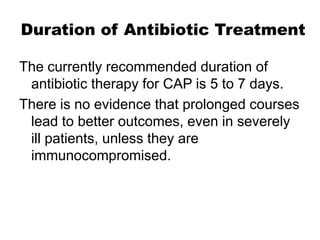
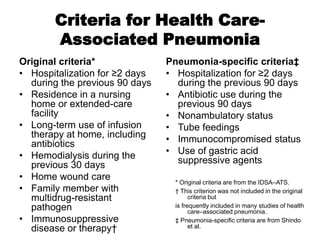
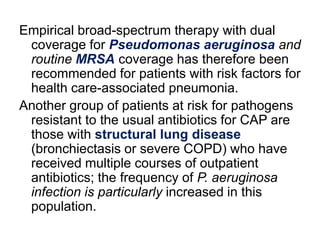
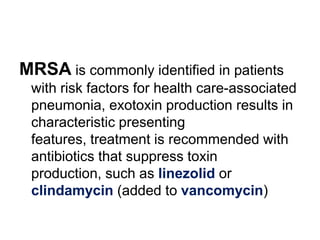
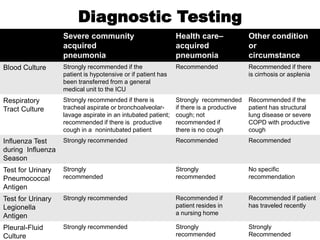
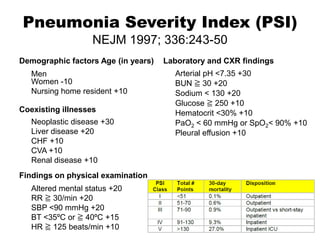
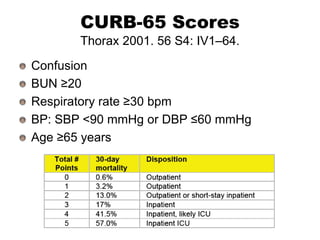
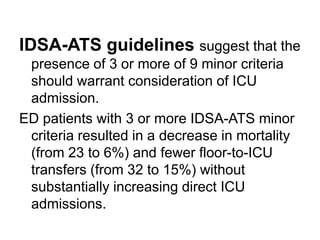
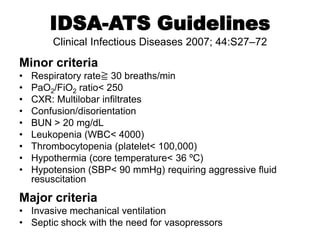
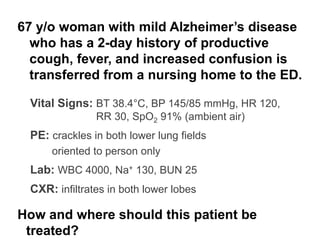
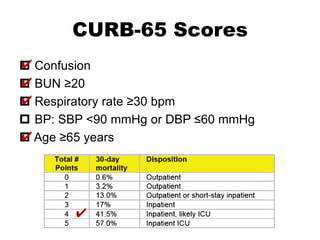
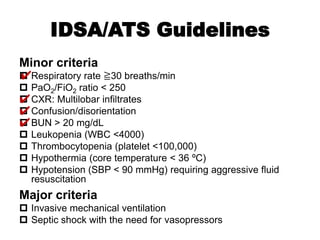
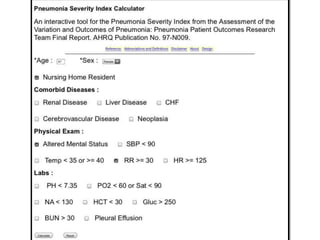
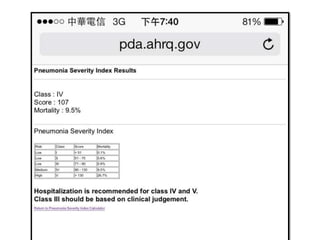
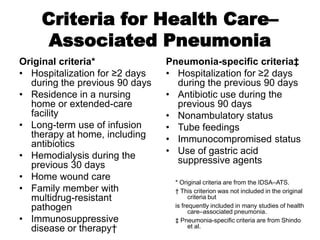
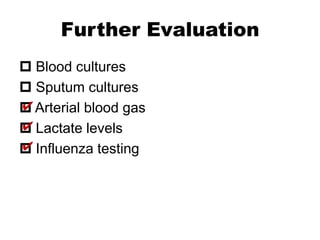
This 67-year-old woman with mild Alzheimer's disease presents with community-acquired pneumonia based on symptoms of productive cough, fever, confusion and exam findings of crackles in both lower lung fields and CXR infiltrates. She meets 3 CURB-65 criteria (confusion, RR≥30, age≥65) and 4 IDSA-ATS minor criteria (RR≥30, confusion, BUN>20, PaO2/FiO2<250) warranting consideration of ICU admission given risk of deterioration. Based on her nursing home residence and recent hospitalization, she also meets criteria for possible healthcare-associated pneumonia and should receive broad-spectrum antibiotics with MRSA and Pseudomonas coverage along with diagnostic