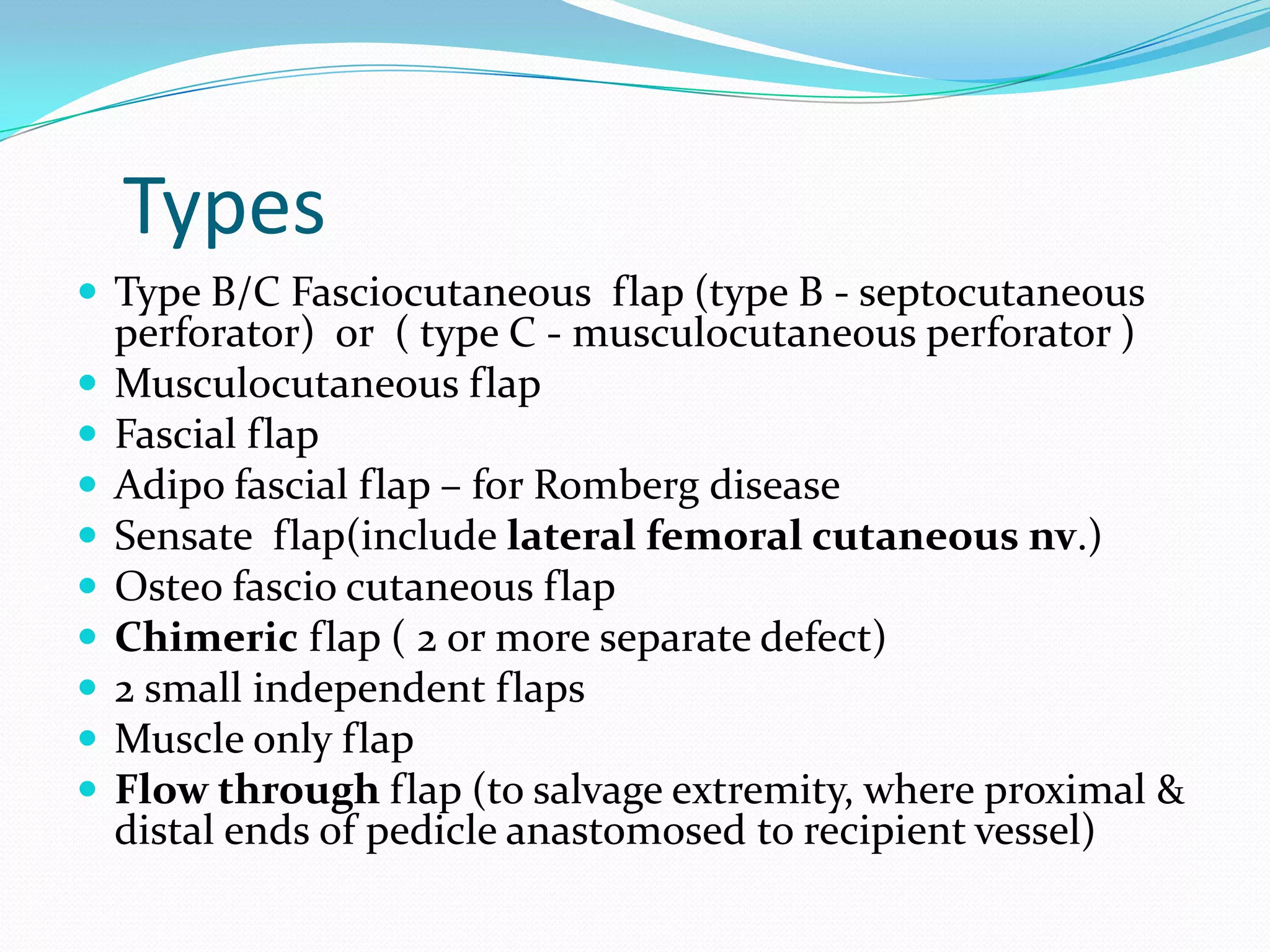
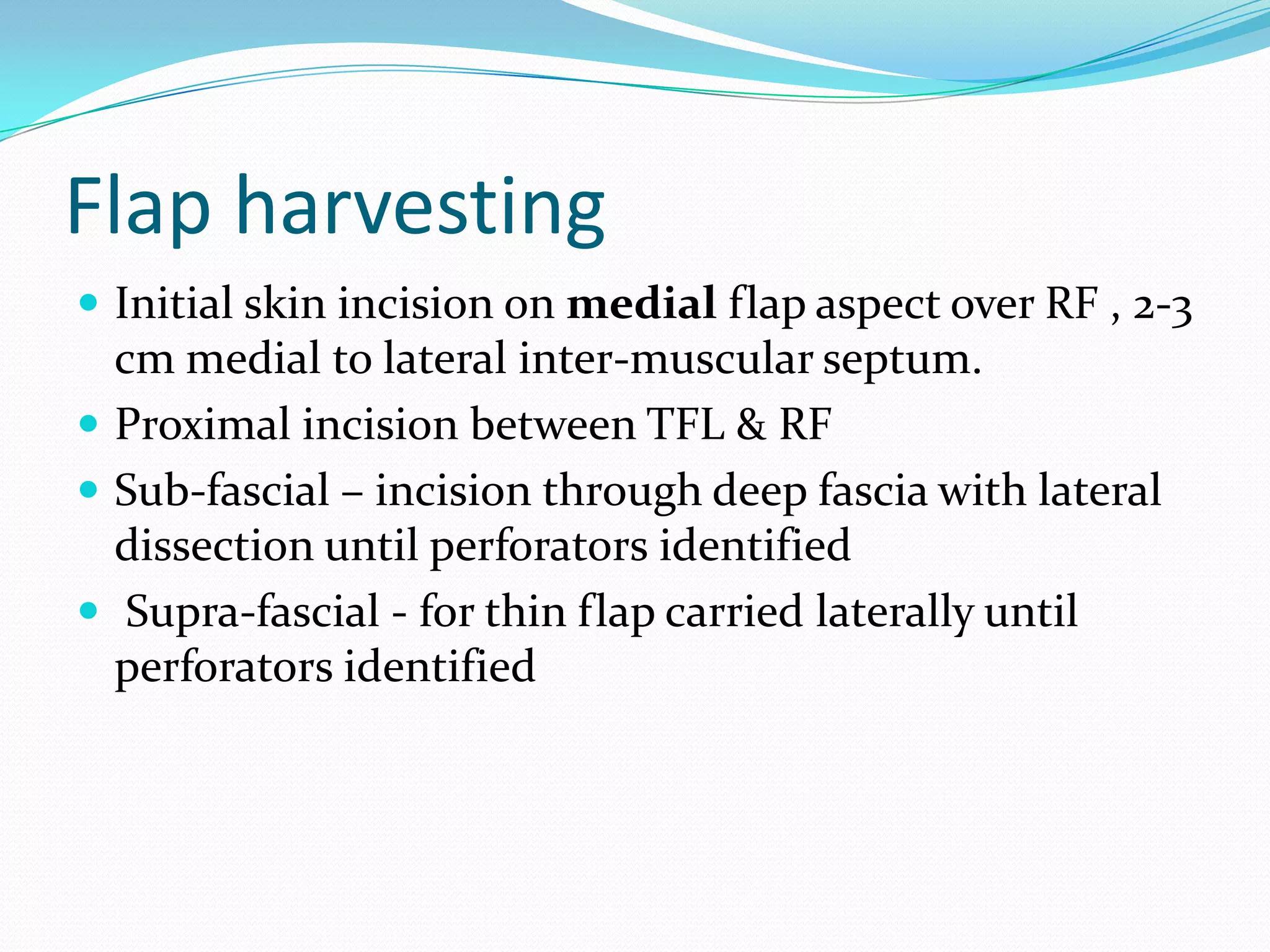
The document summarizes the anterolateral thigh (ALT) flap, which has become a popular reconstructive option. It describes the history and indications of the ALT flap, including head and neck and extremity reconstruction. The key aspects of evaluating patients, raising the flap, and post-operative care and complications are covered. The advantages include a long vascular pedicle and ability to harvest a large skin paddle, while disadvantages include a bulky flap and potential donor site morbidity. Variations in anatomy are also discussed.