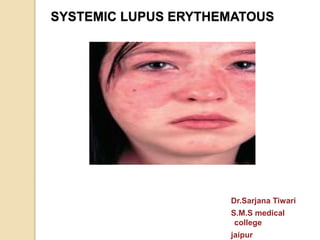
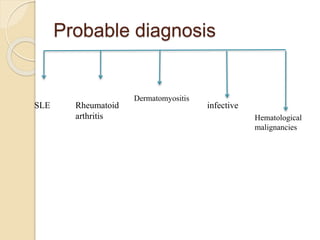
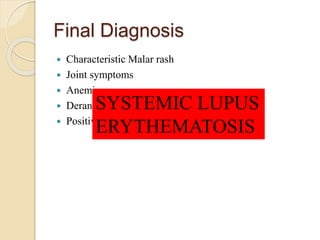
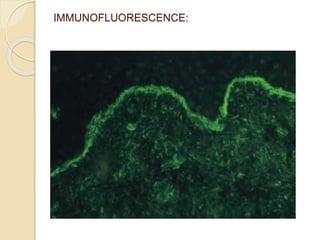
This document presents a case of a 30-year-old female with a 3 month history of fever, 2 month history of multiple joint pains and swelling, and 1 month history of rash over her face and body. Physical examination revealed a febrile patient with erythematous rash, joint swelling and limitation of movement. Laboratory tests showed pancytopenia, elevated ESR and creatinine, low complement levels, and positive ANA and dsDNA antibodies. A renal biopsy was consistent with lupus nephritis. Based on her presentation and test results, the patient was diagnosed with systemic lupus erythematosus.