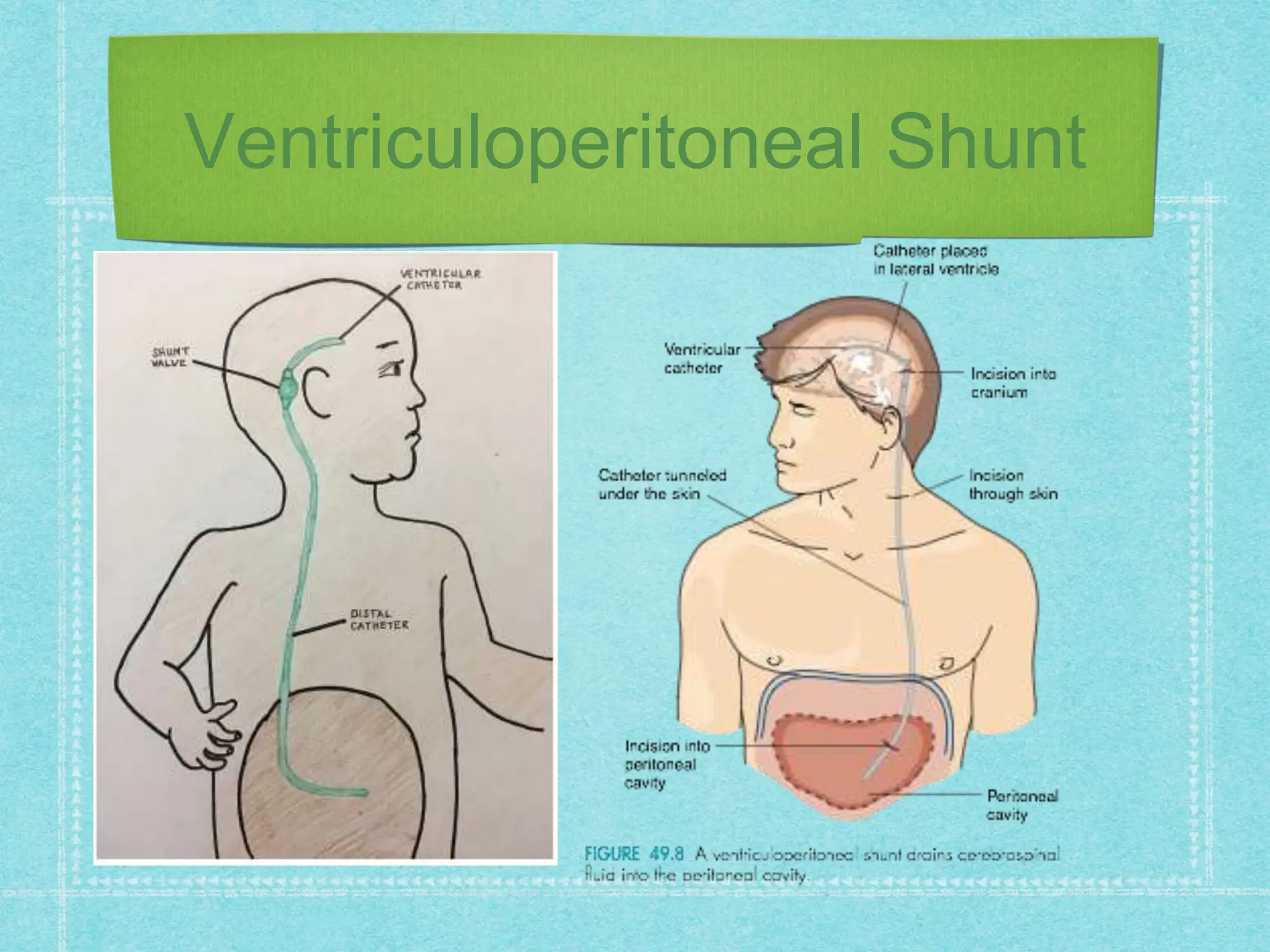
The document provides a comprehensive overview of hydrocephalus, its causes, treatment options, and the specifics of ventriculoperitoneal shunt (VPS) placement as a solution for excess cerebrospinal fluid. It details indications for shunt placement, potential complications, and the nursing care necessary for patients post-surgery, emphasizing the importance of monitoring for signs of infection and increased intracranial pressure. Important procedural steps and patient education for ongoing care are highlighted, ensuring that families are informed about shunt management and potential complications.