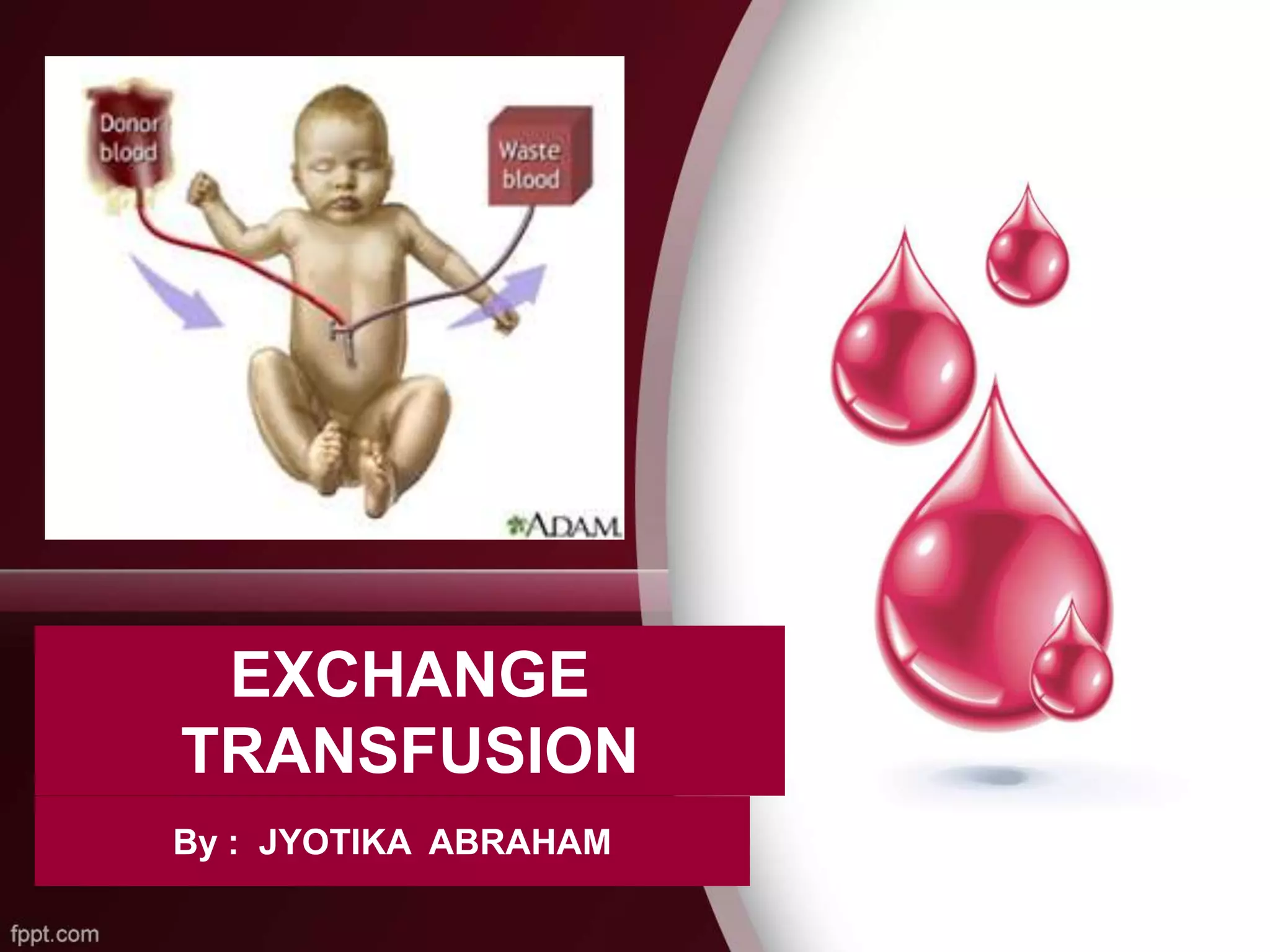
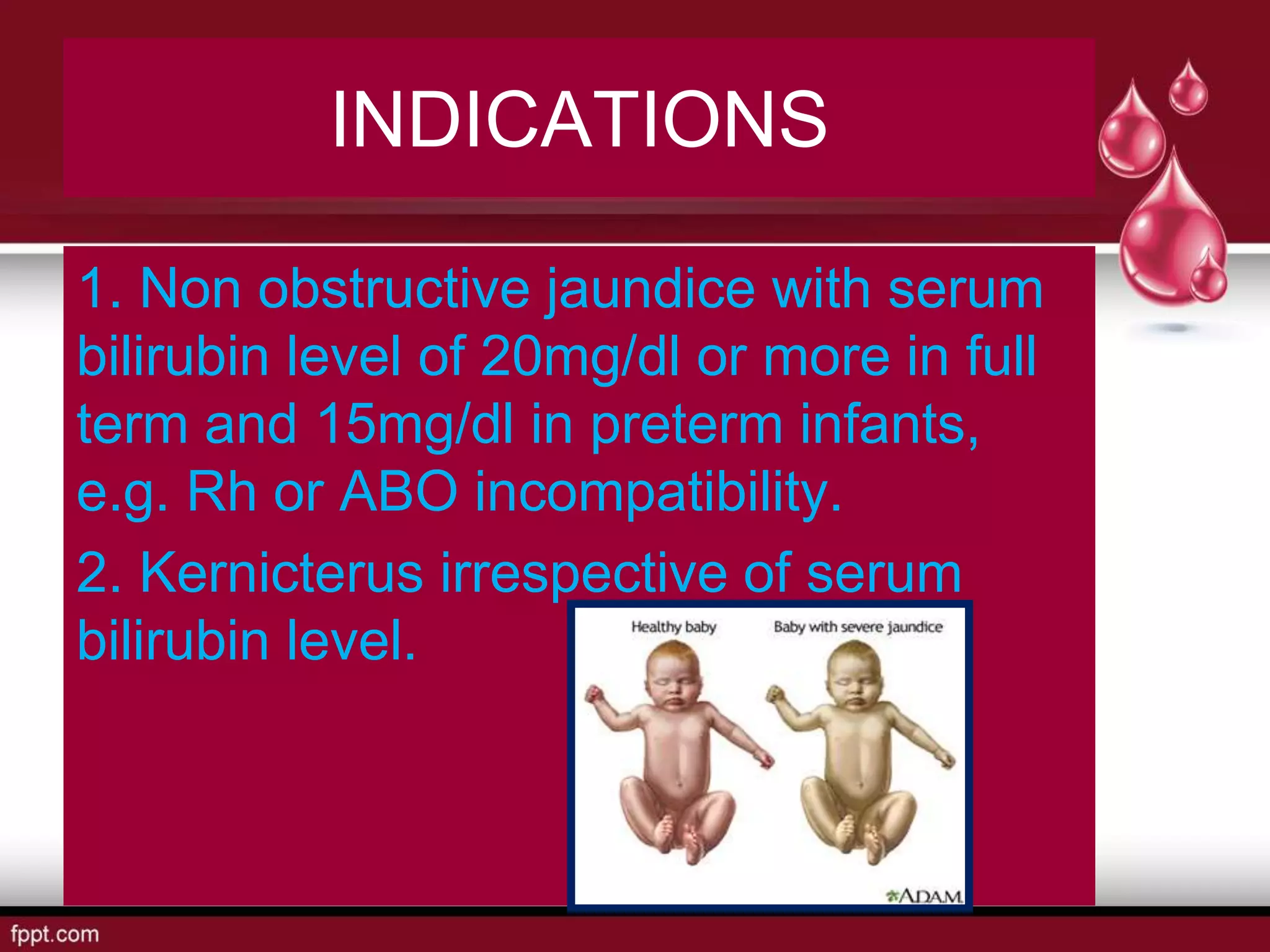
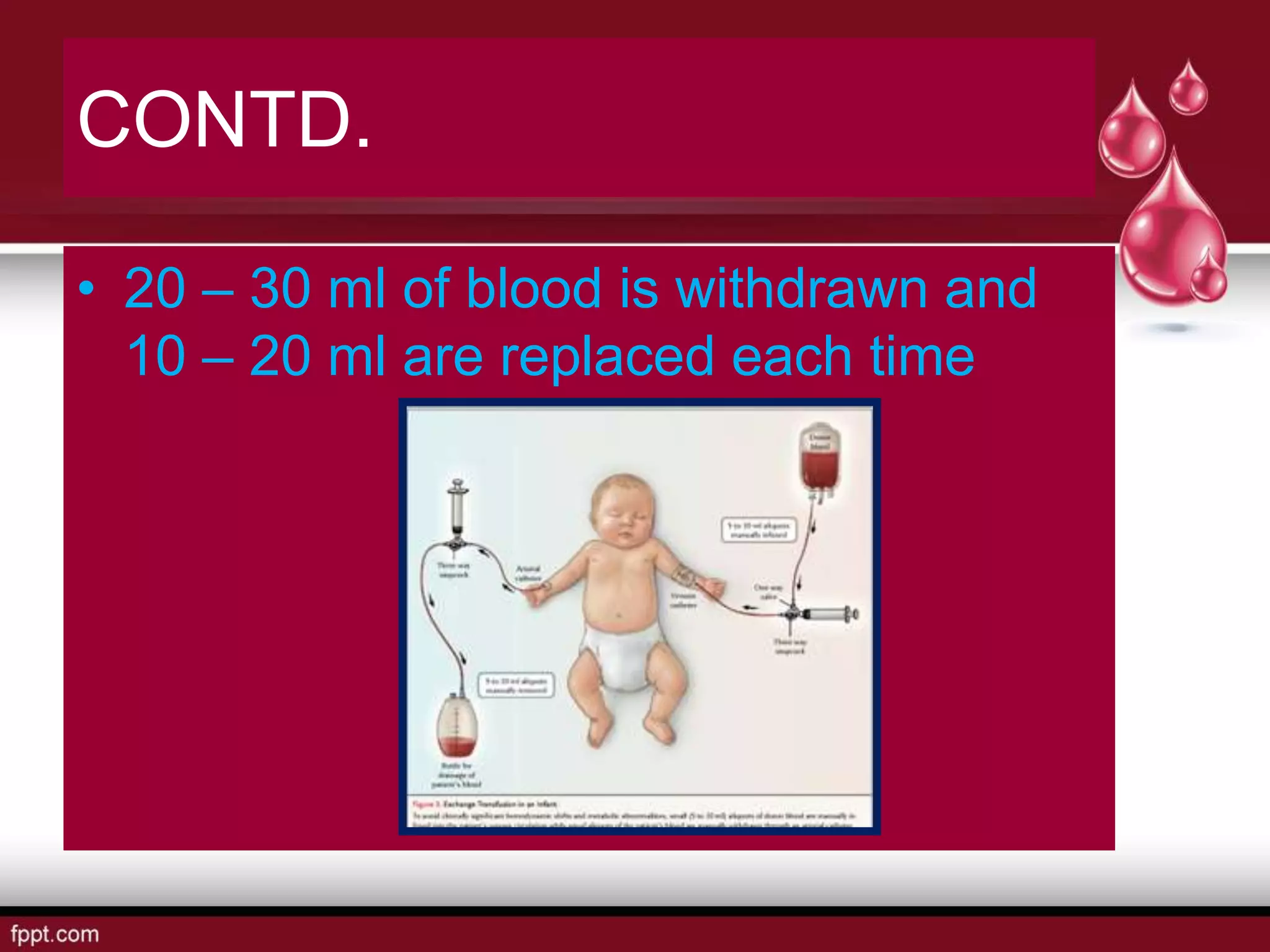
Exchange transfusion is a medical procedure for infants aimed at correcting anemia and removing high bilirubin levels by replacing blood through the umbilical vein. It is indicated for severe jaundice, kernicterus, and specific hemolytic diseases with defined criteria. The procedure requires careful preparation, including equipment collection, informed consent, and monitoring during and after the transfusion to prevent complications.