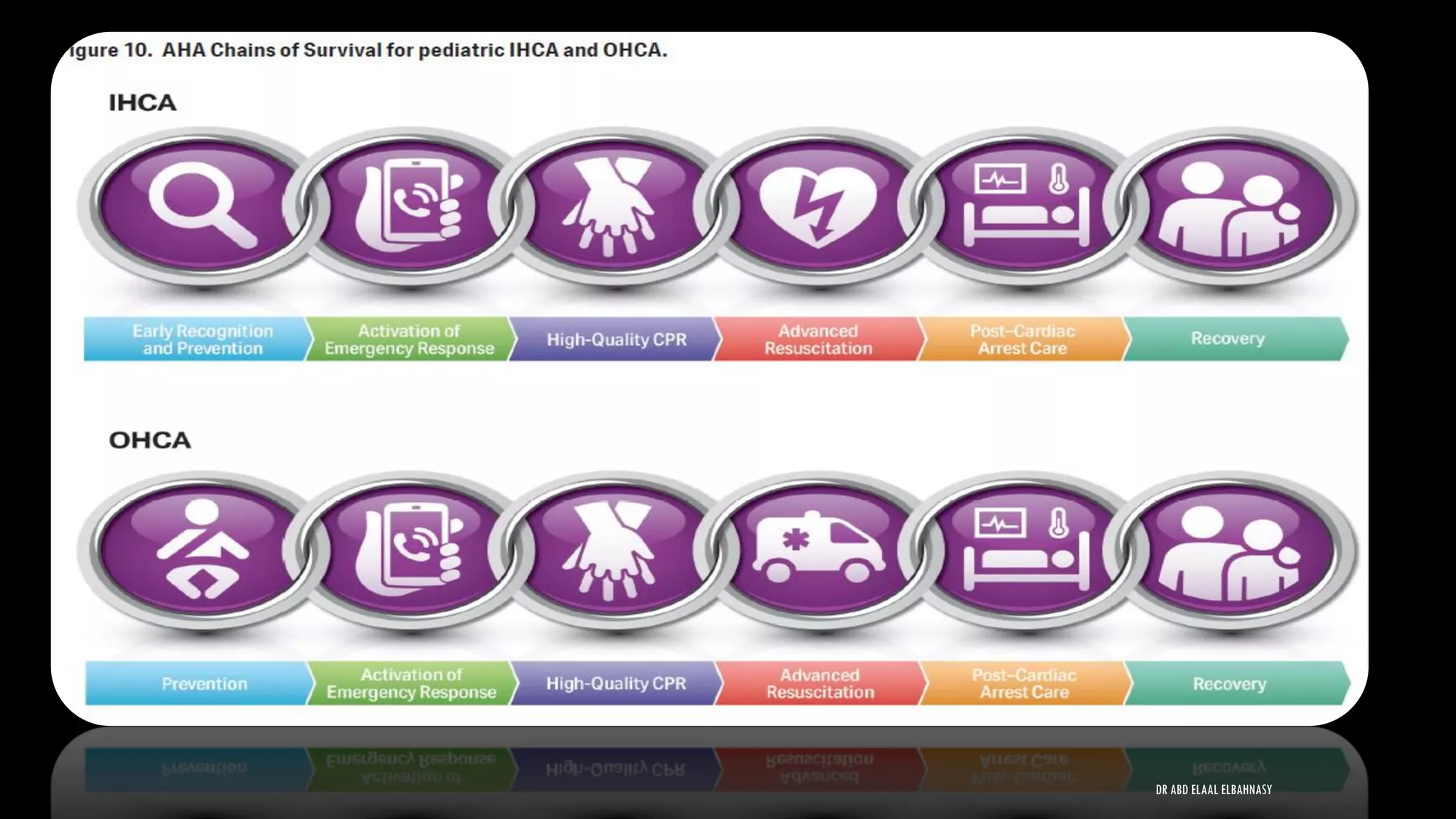
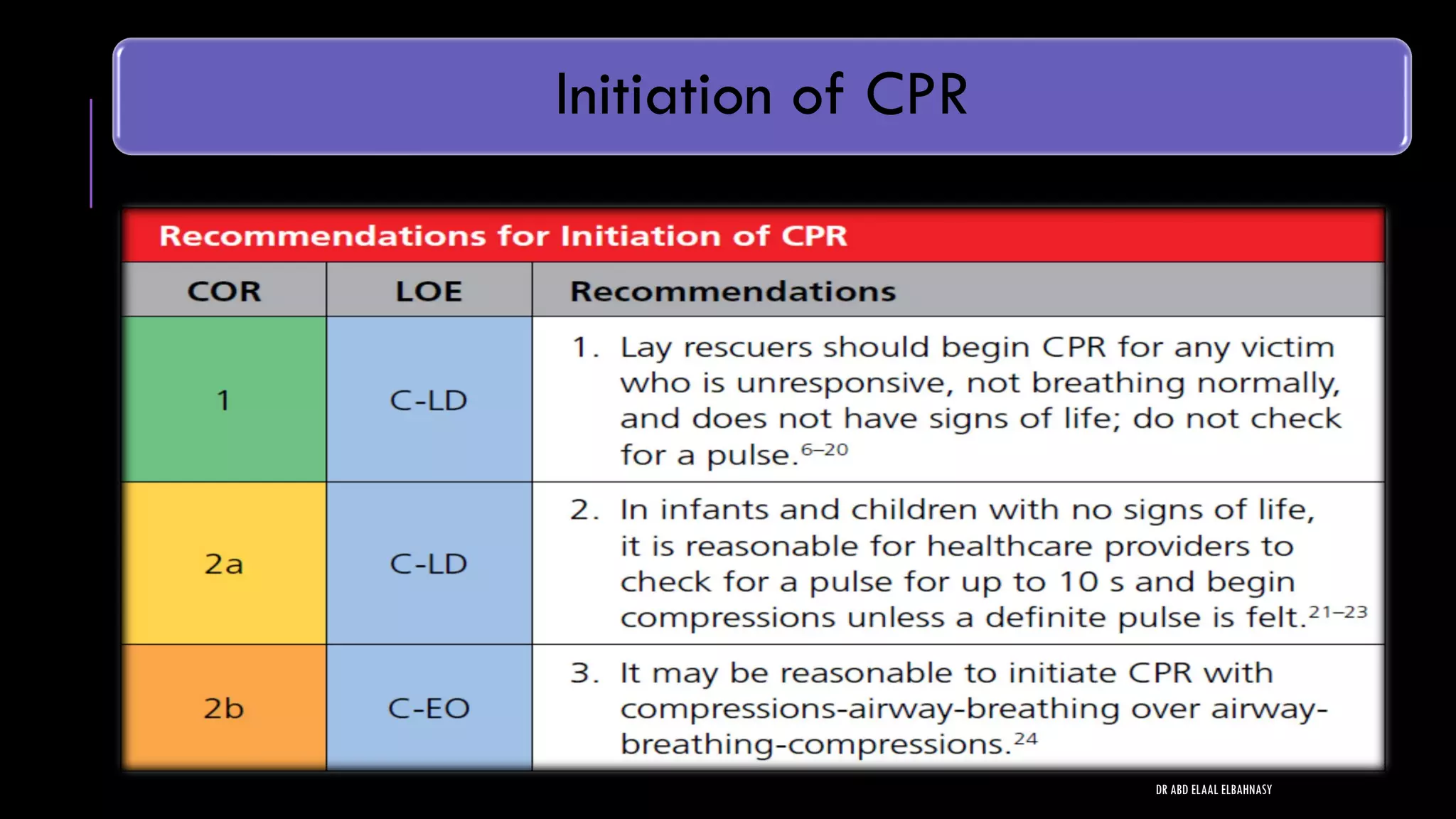
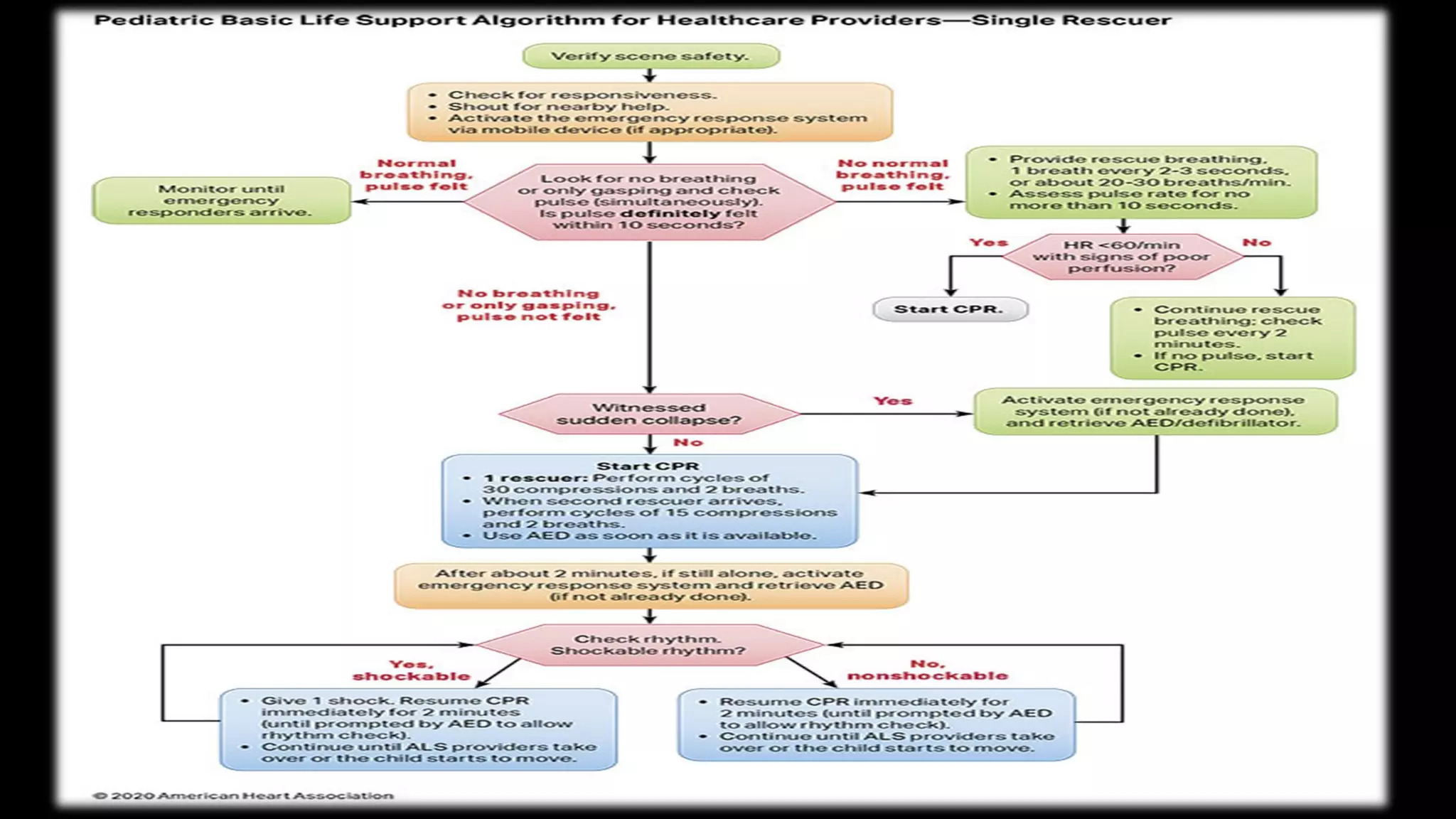
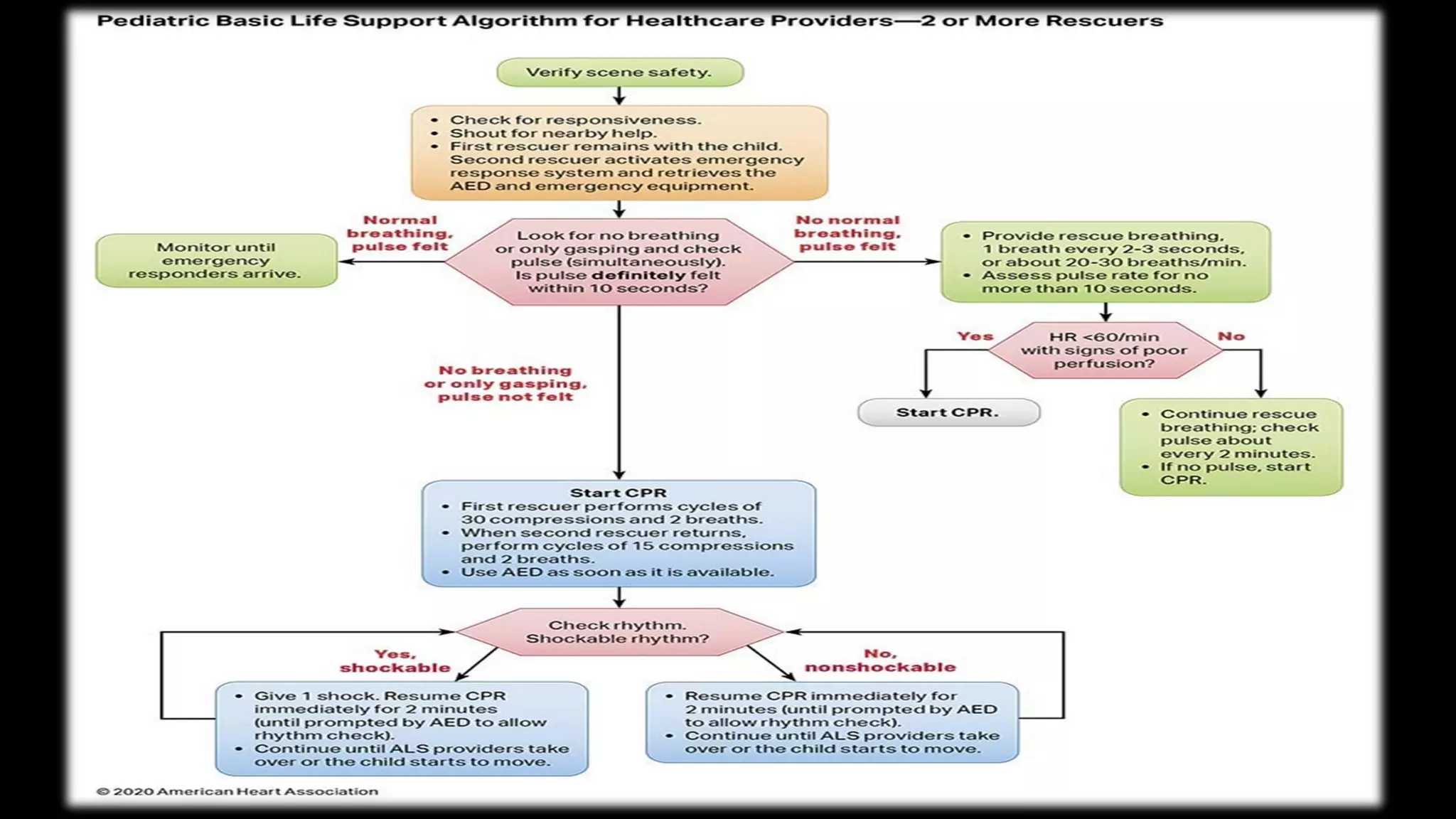
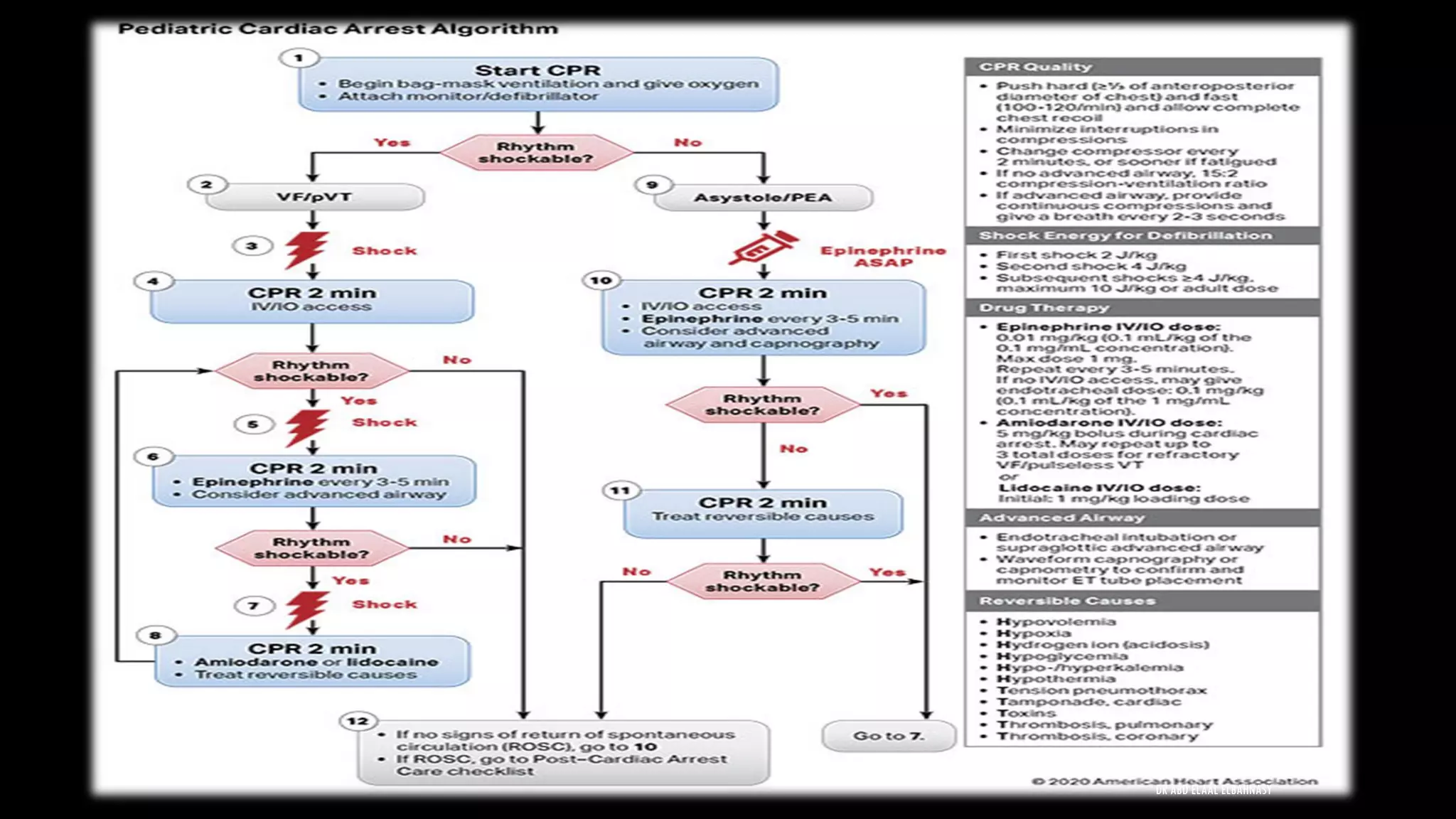
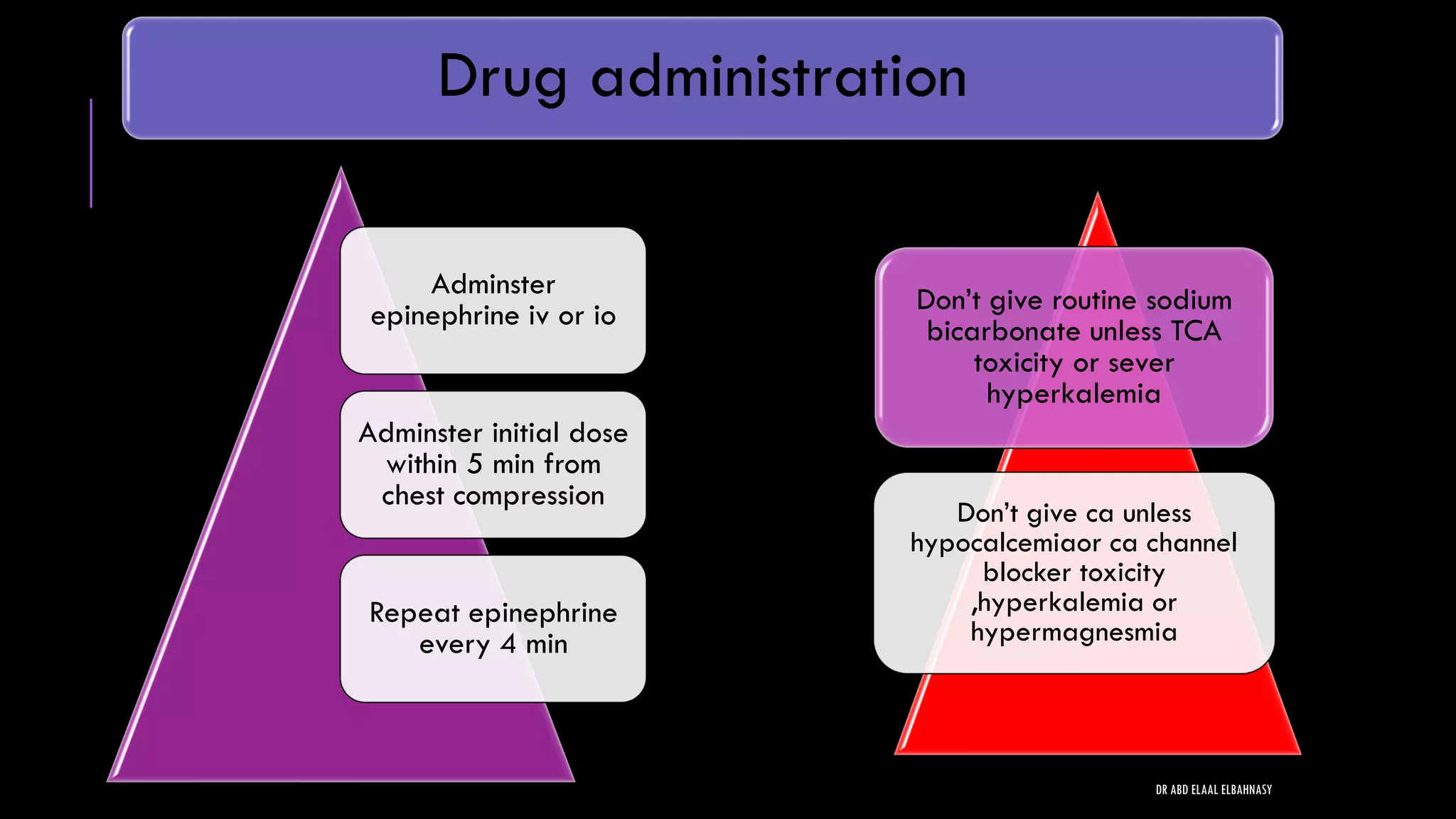
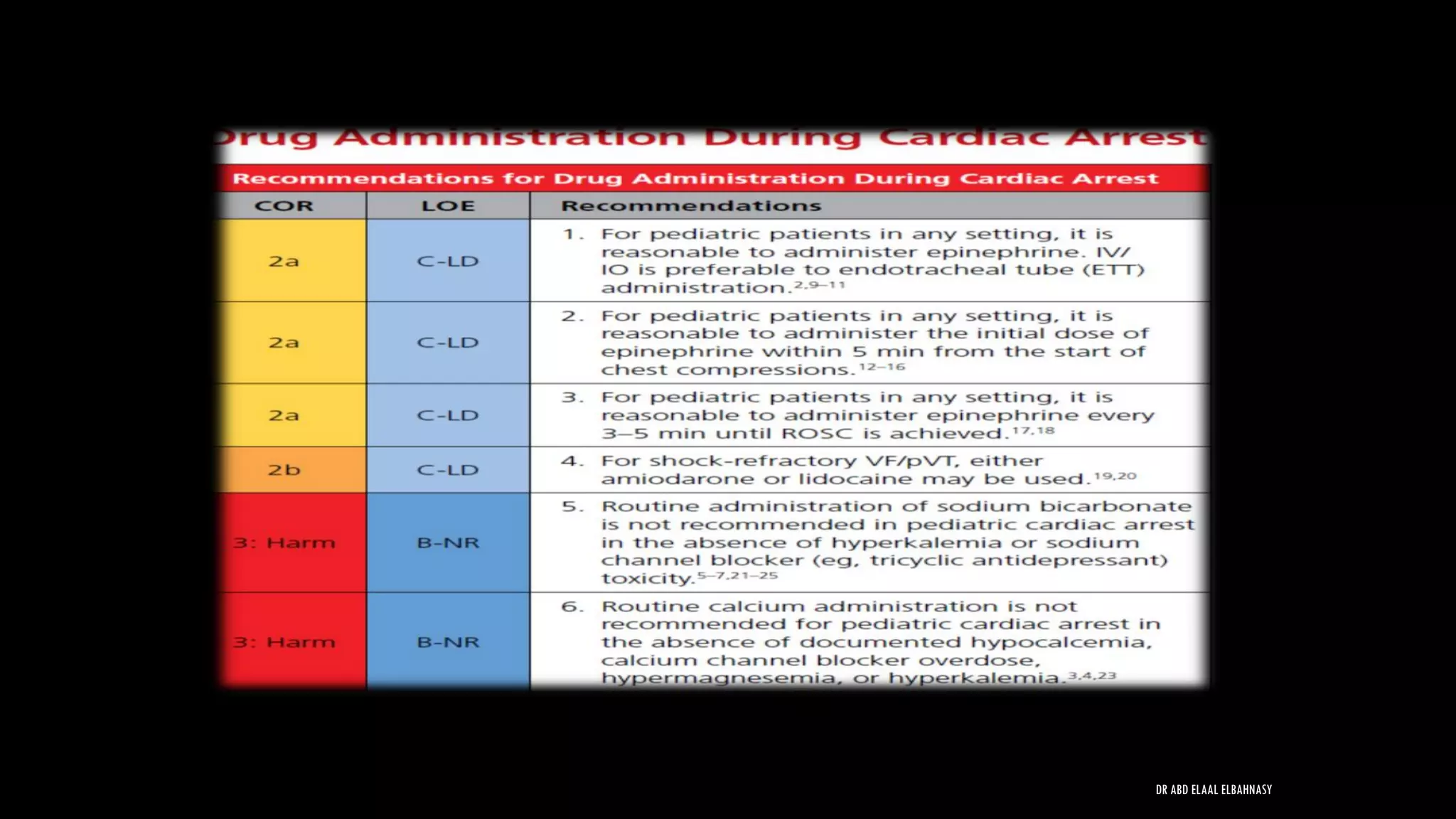
This document provides an overview and updates to pediatric life support in 2020. It discusses several key points:
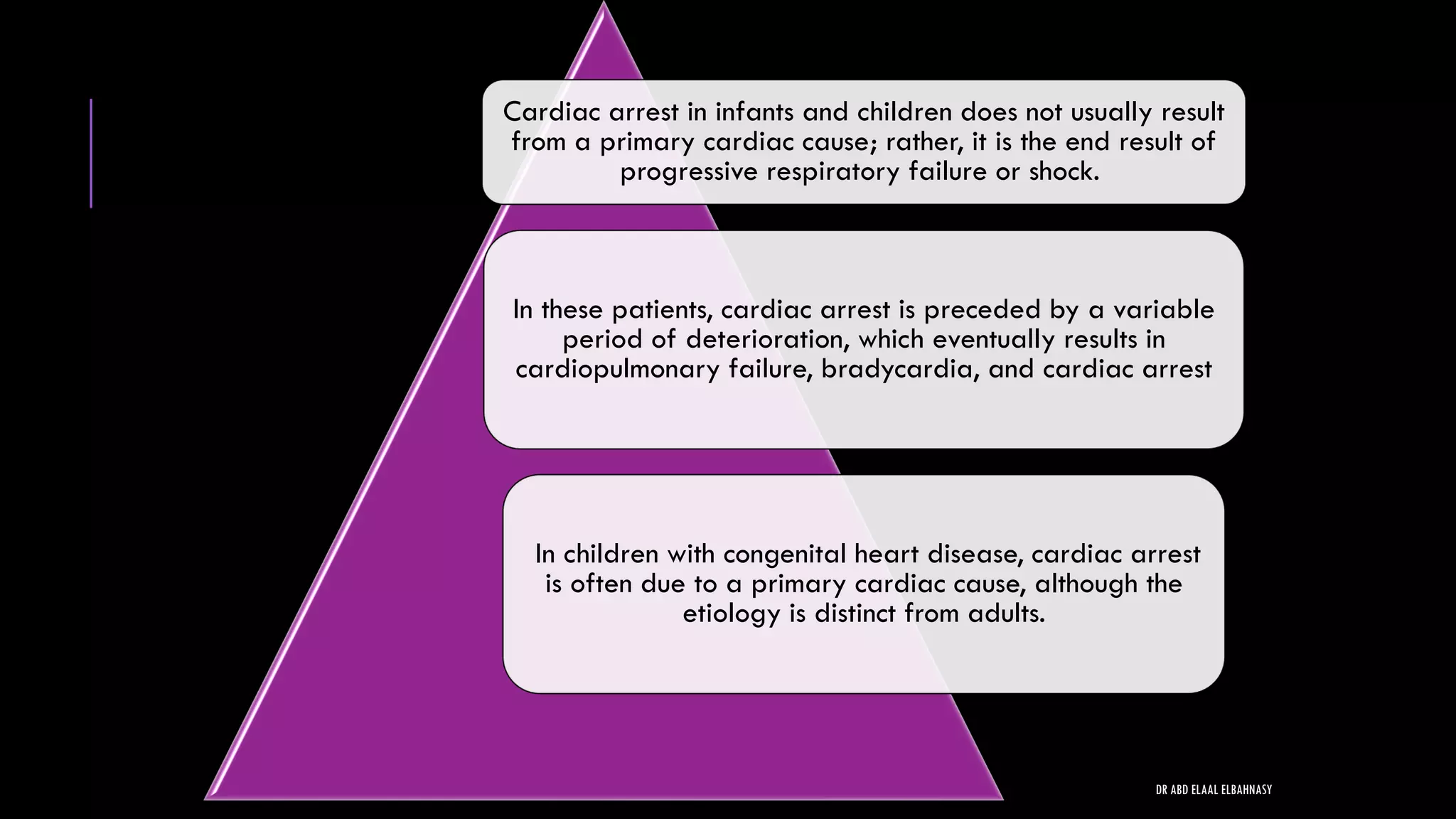
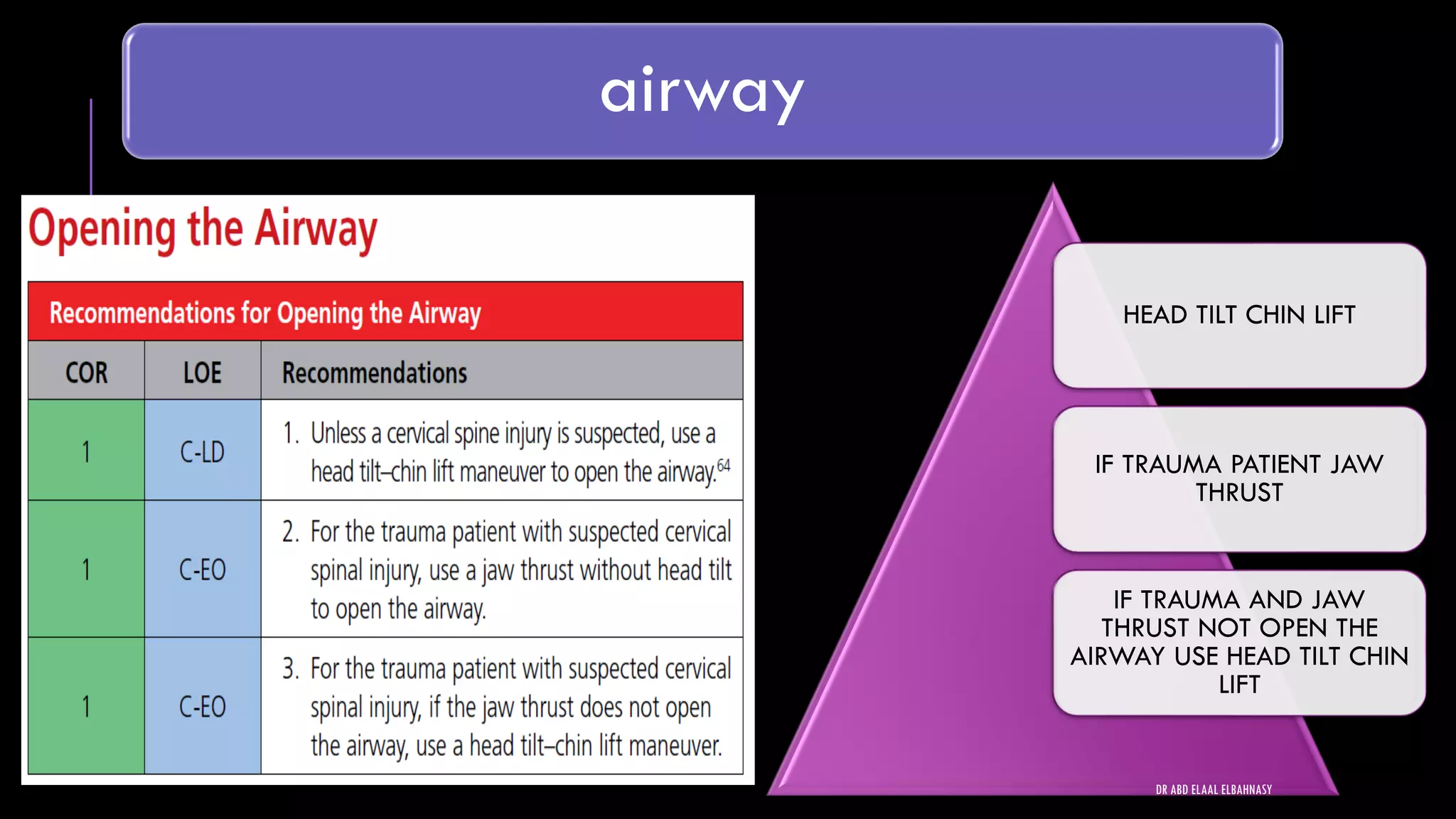
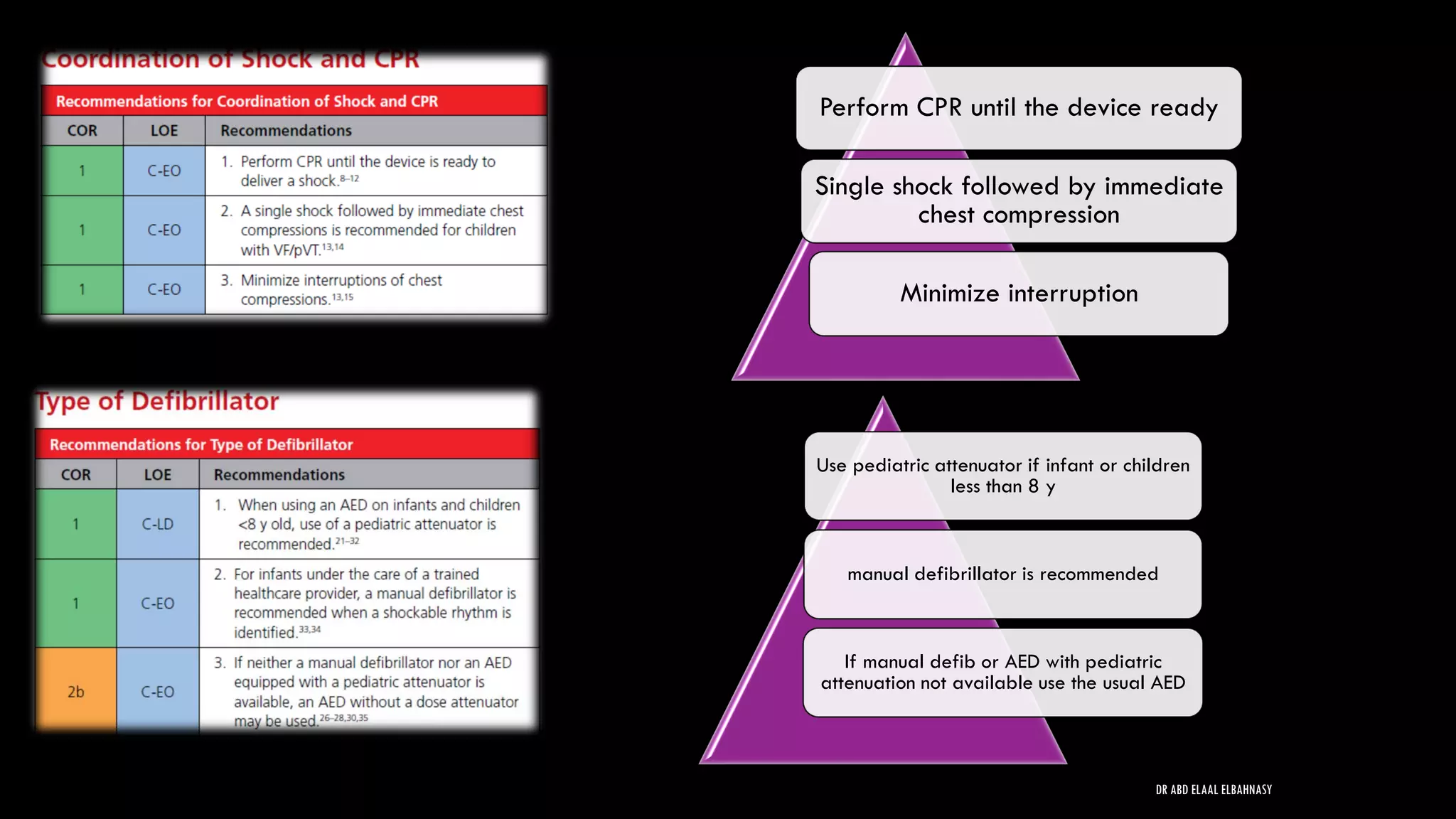
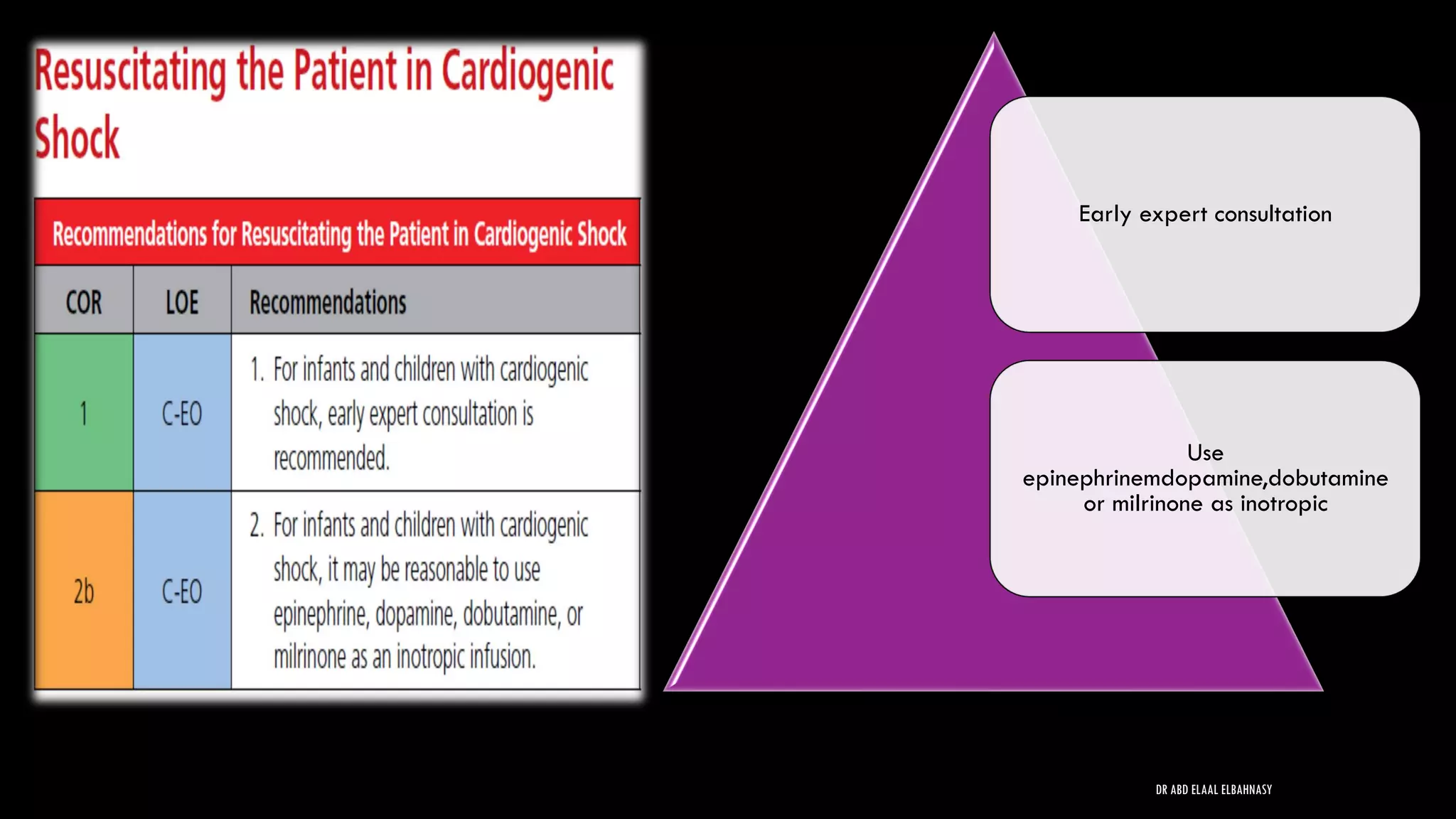
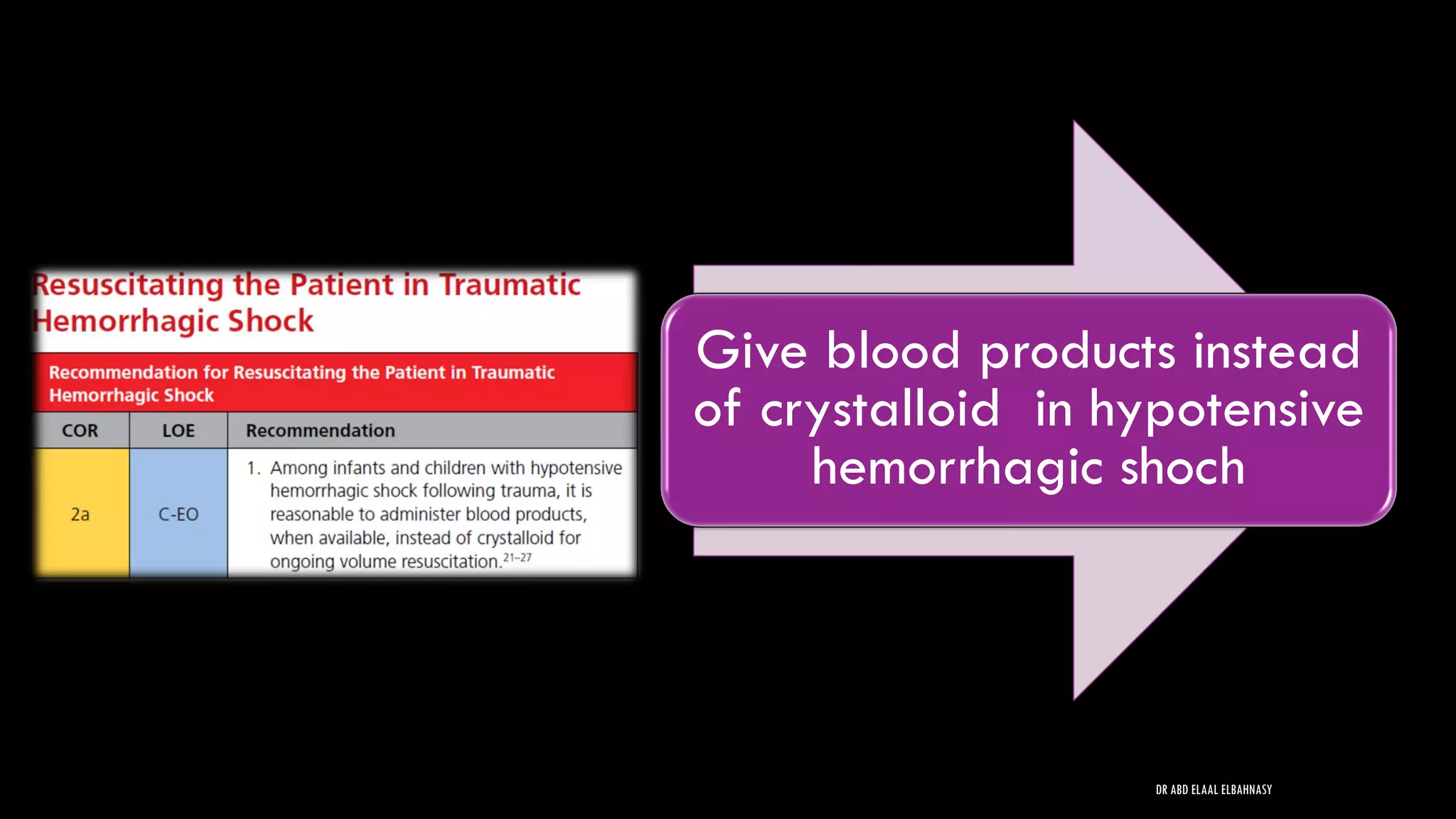
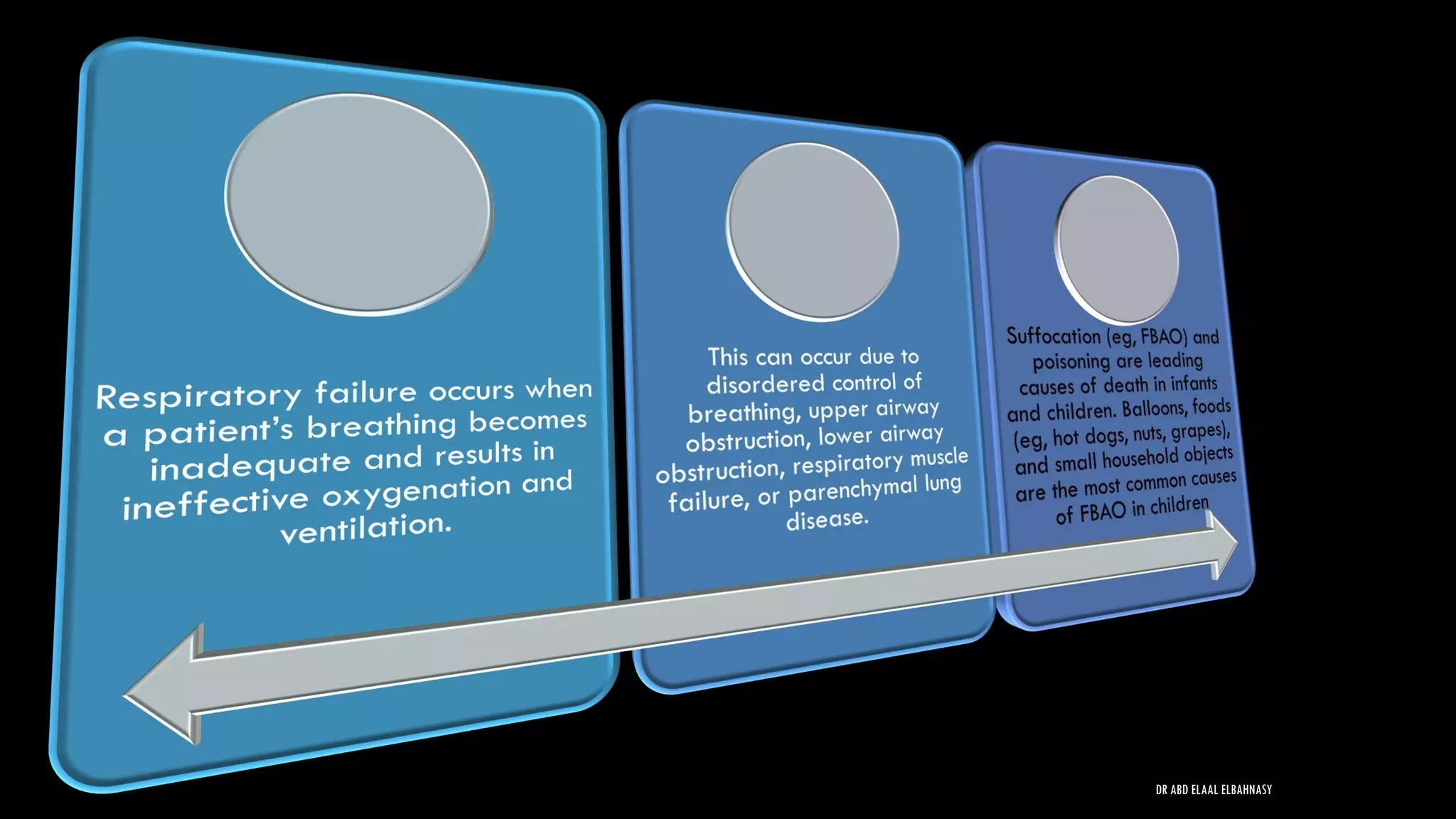
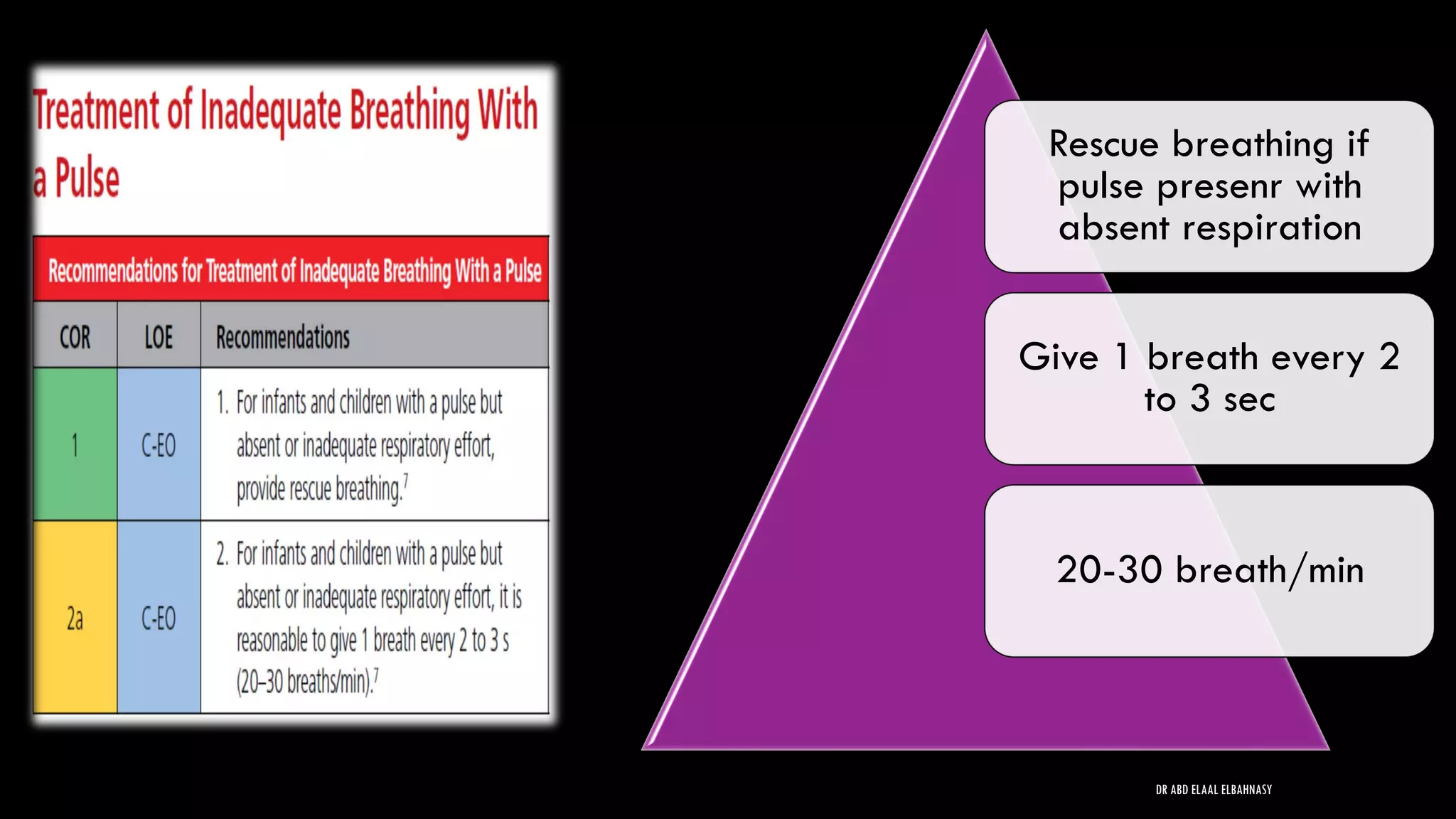
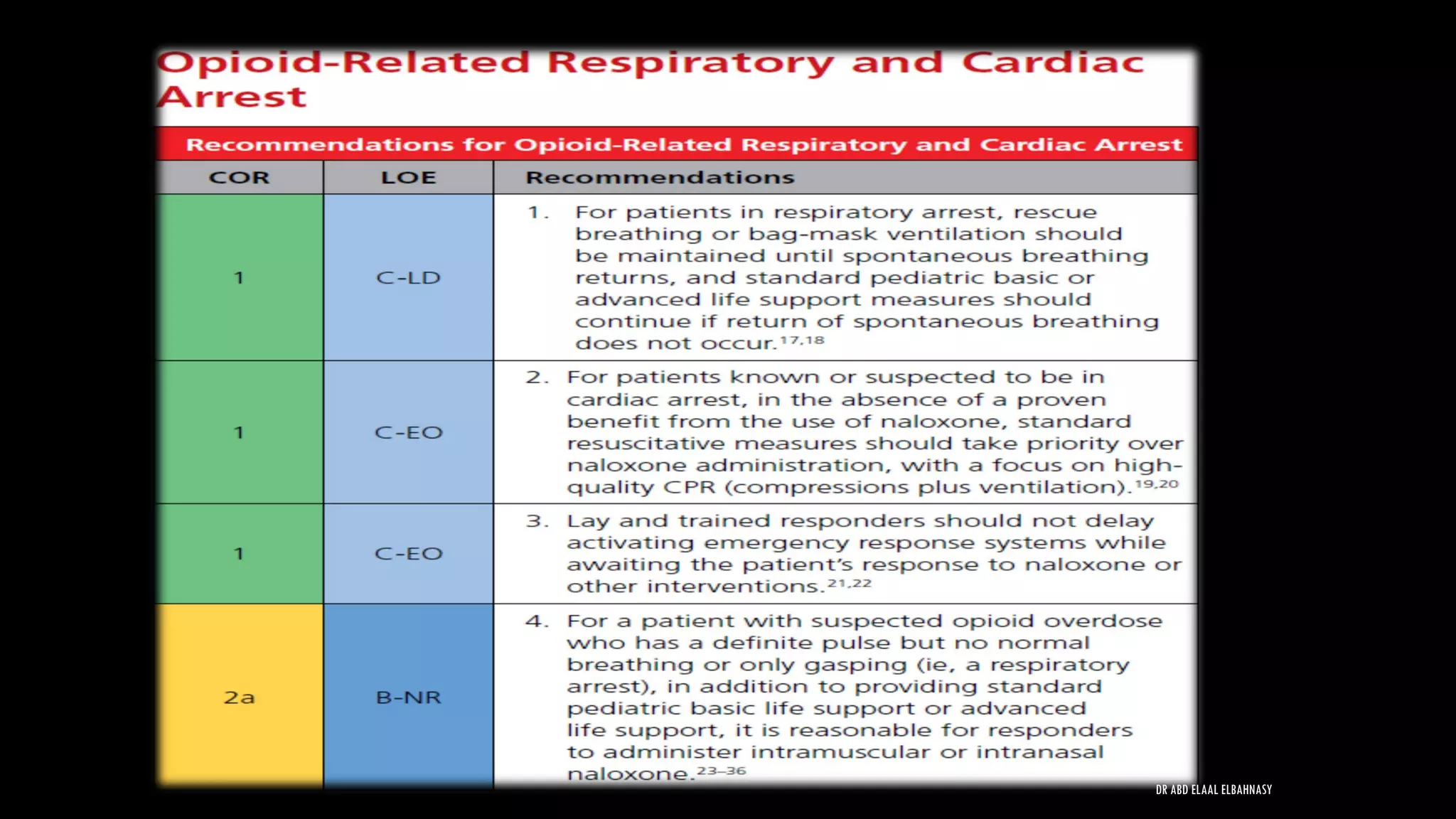
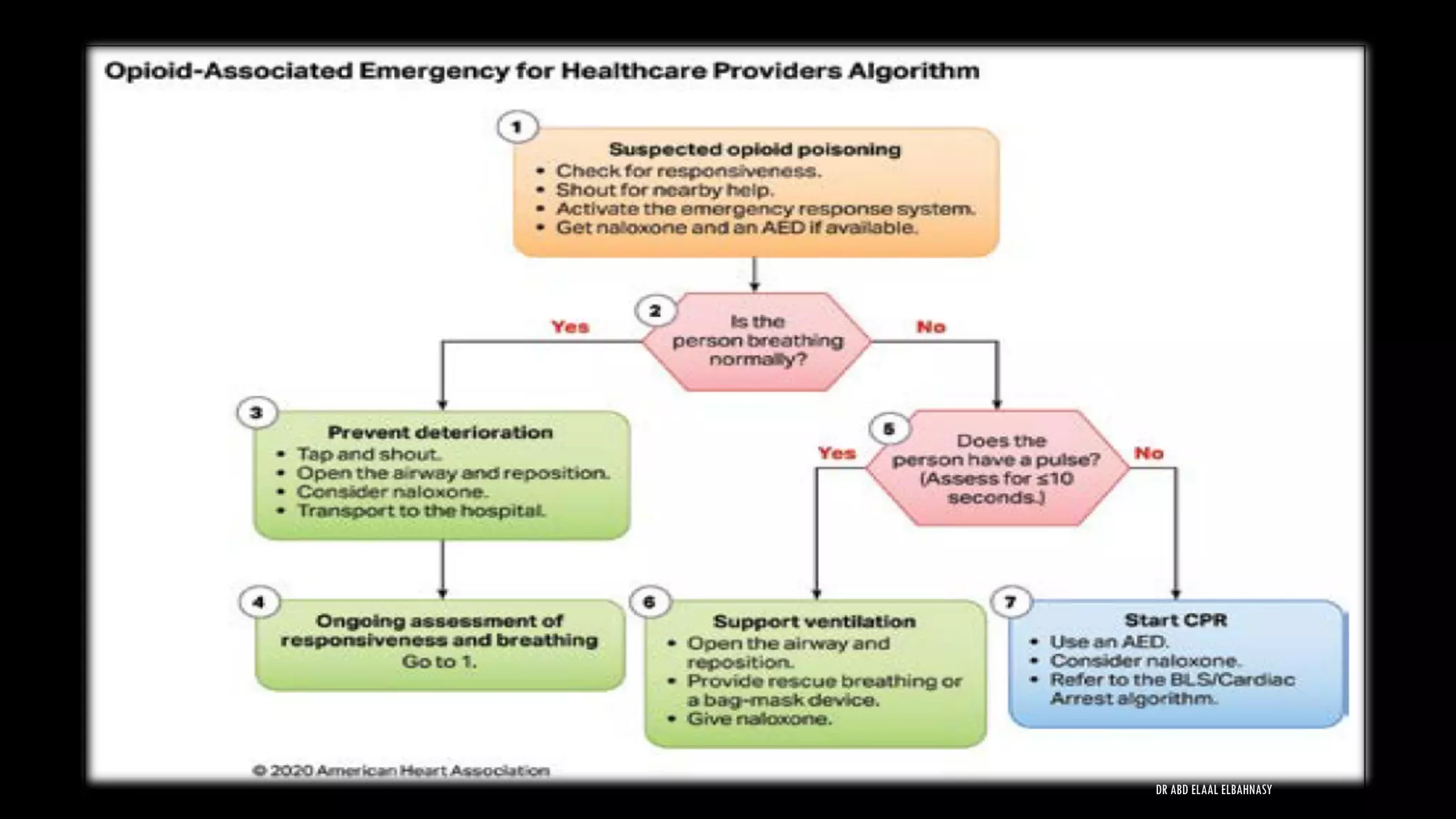
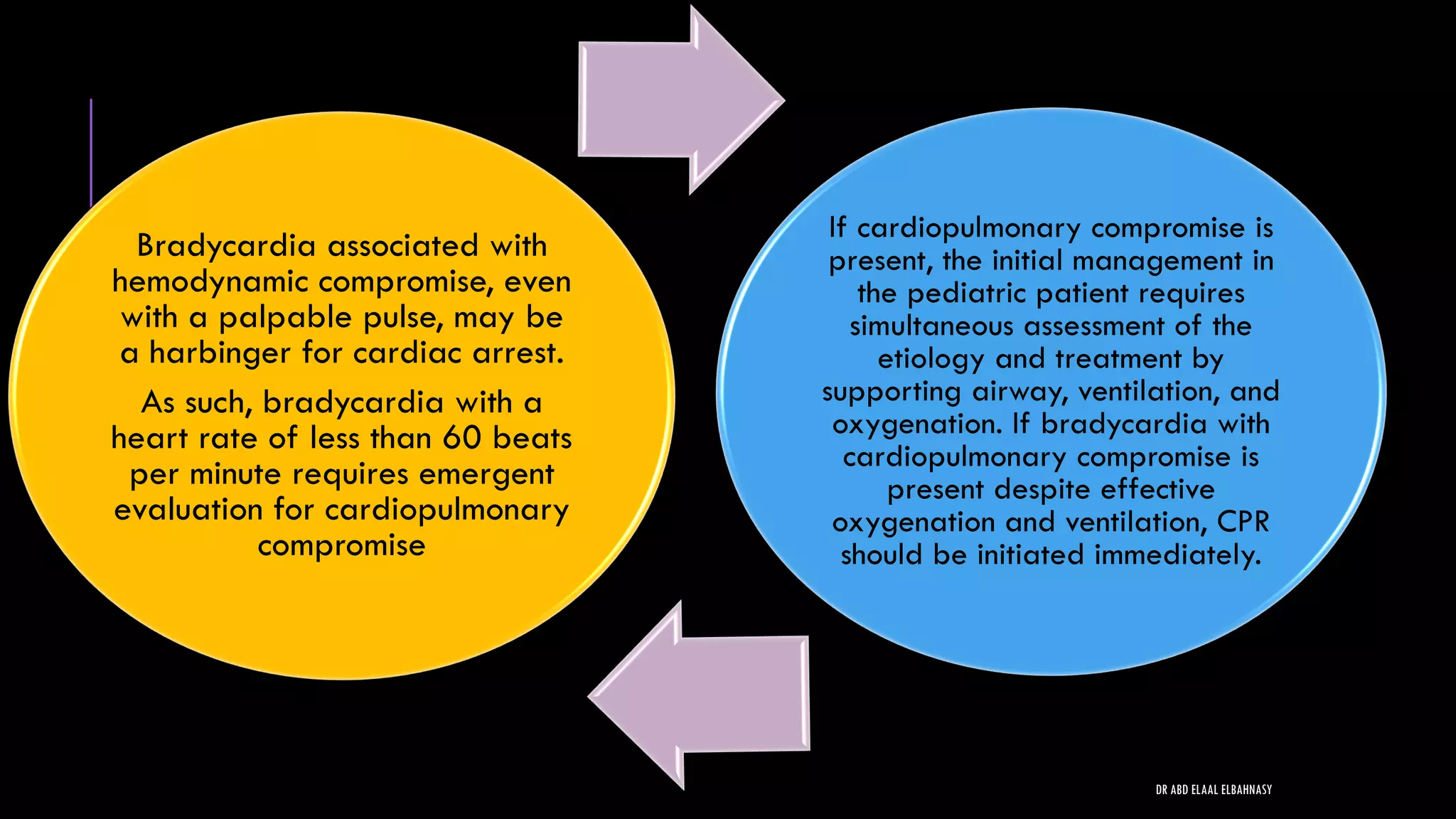
1) Cardiac arrest in children is usually caused by respiratory failure or shock rather than primary cardiac issues.
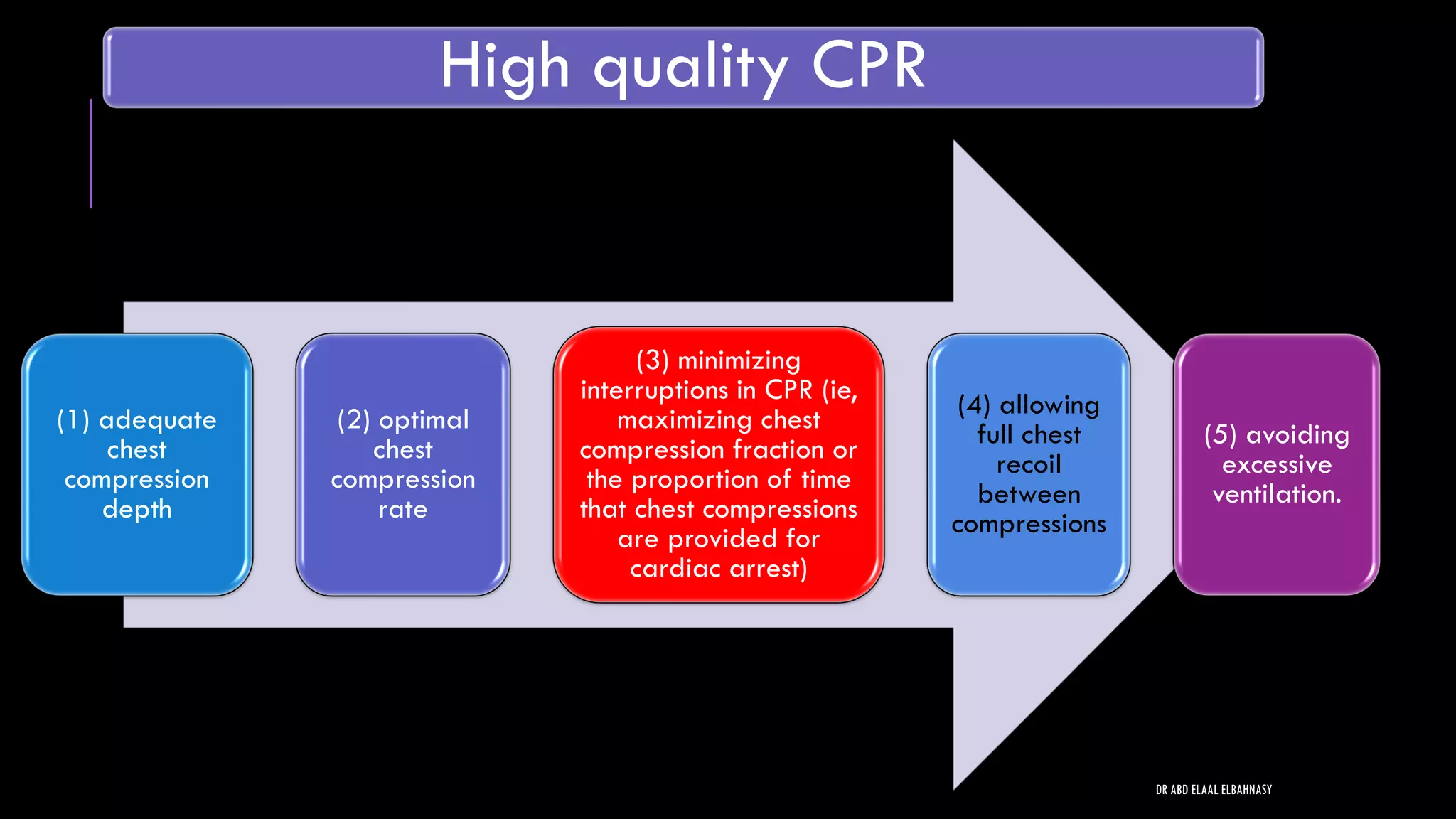
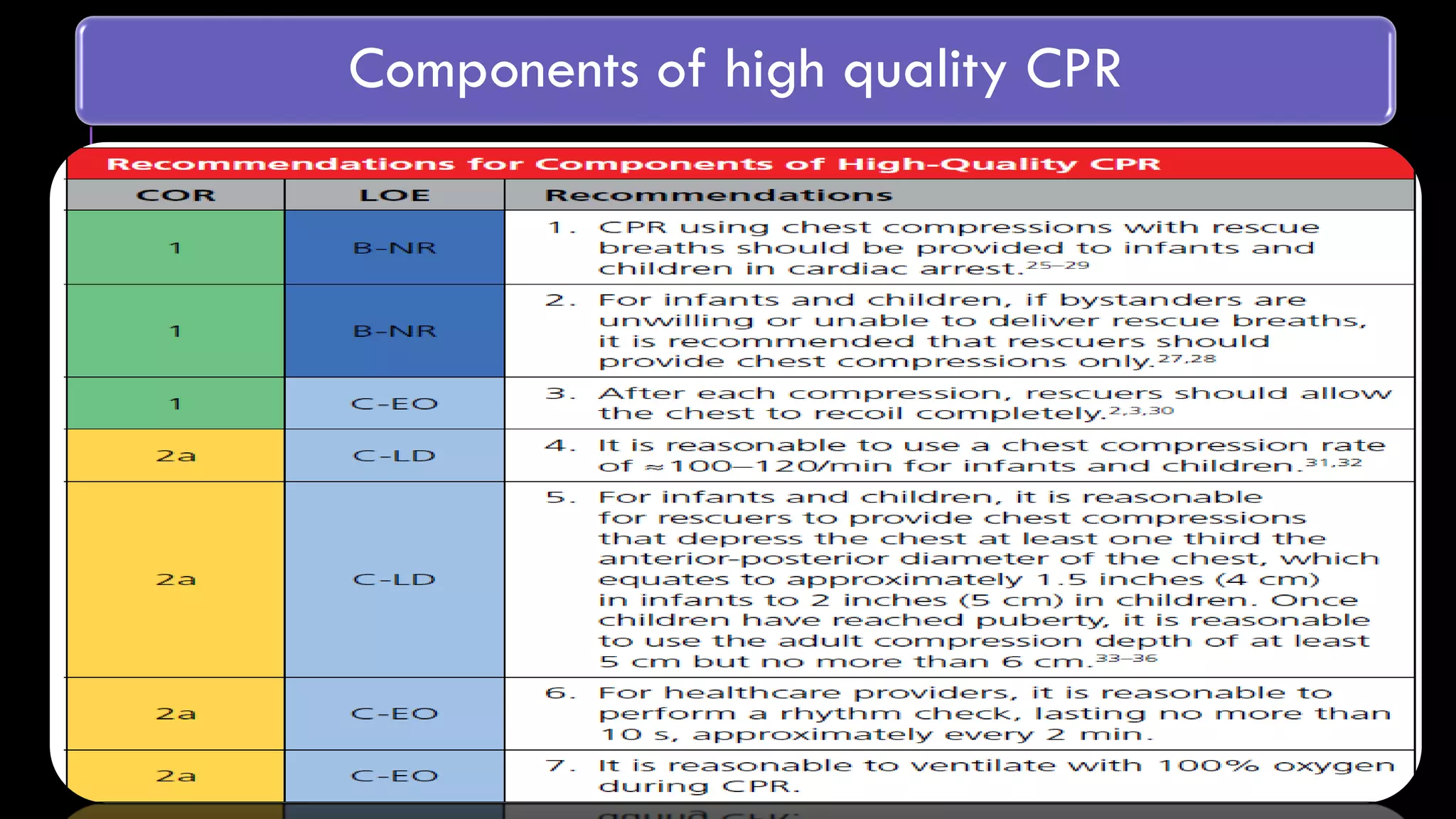
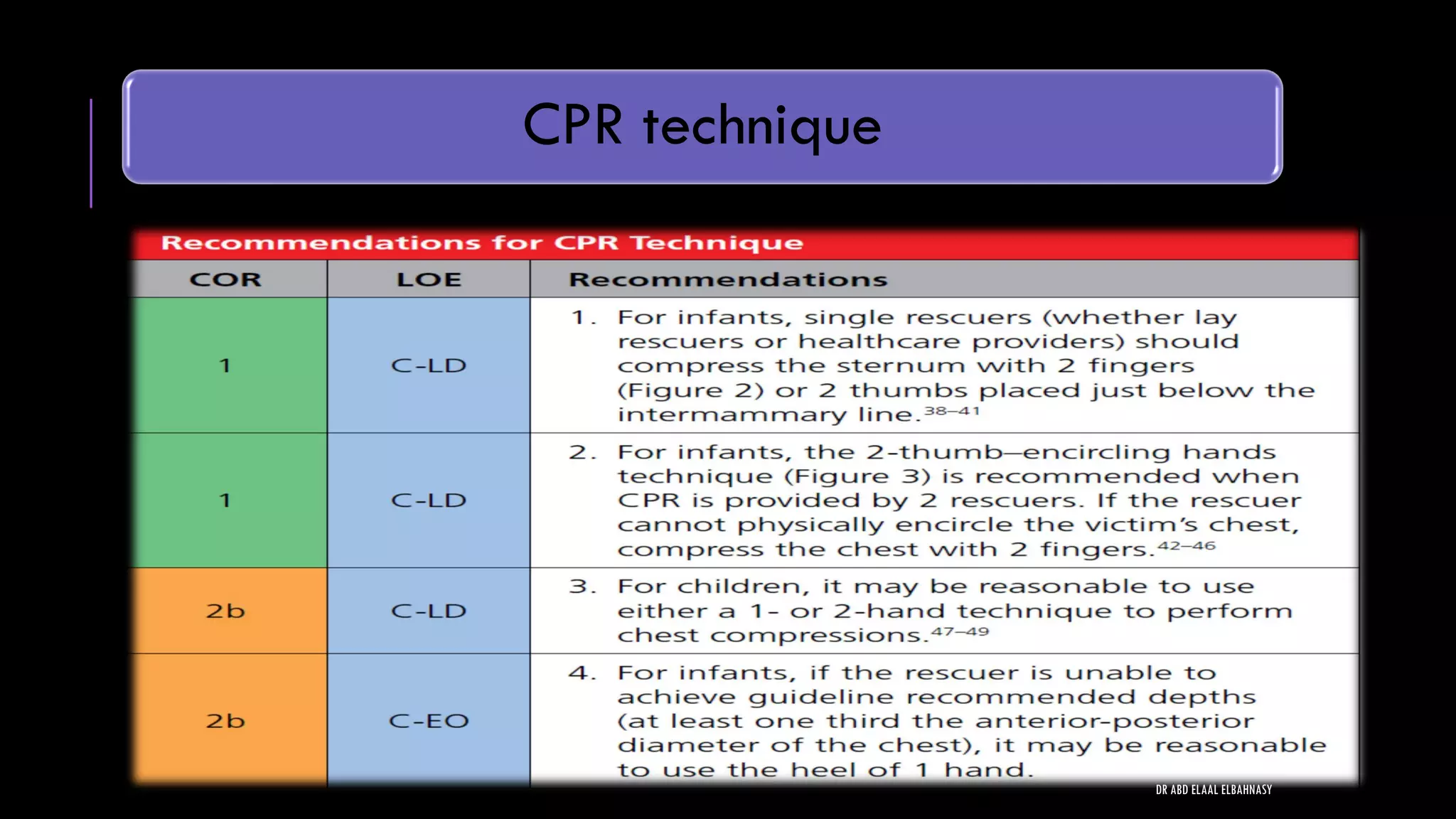
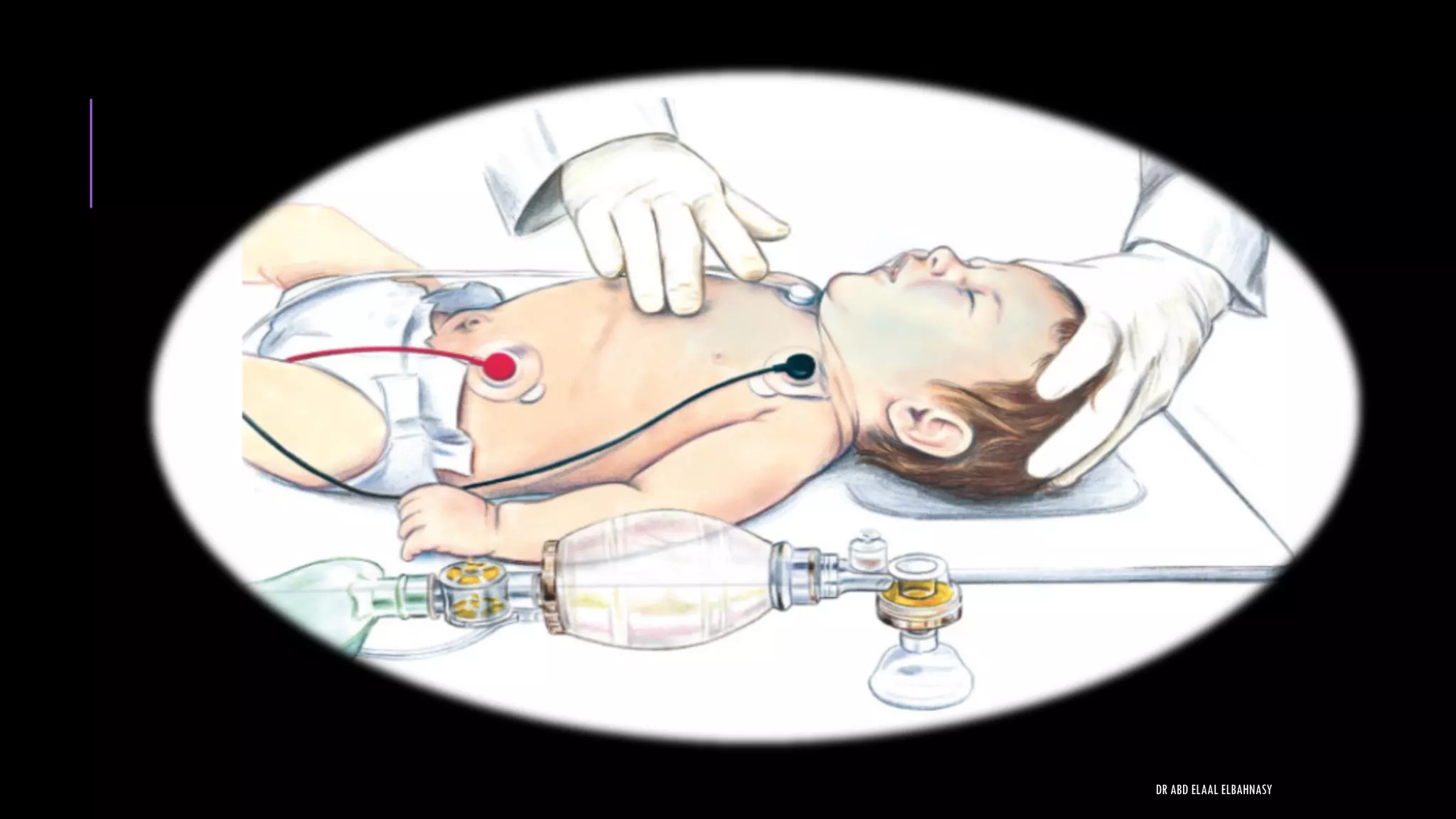
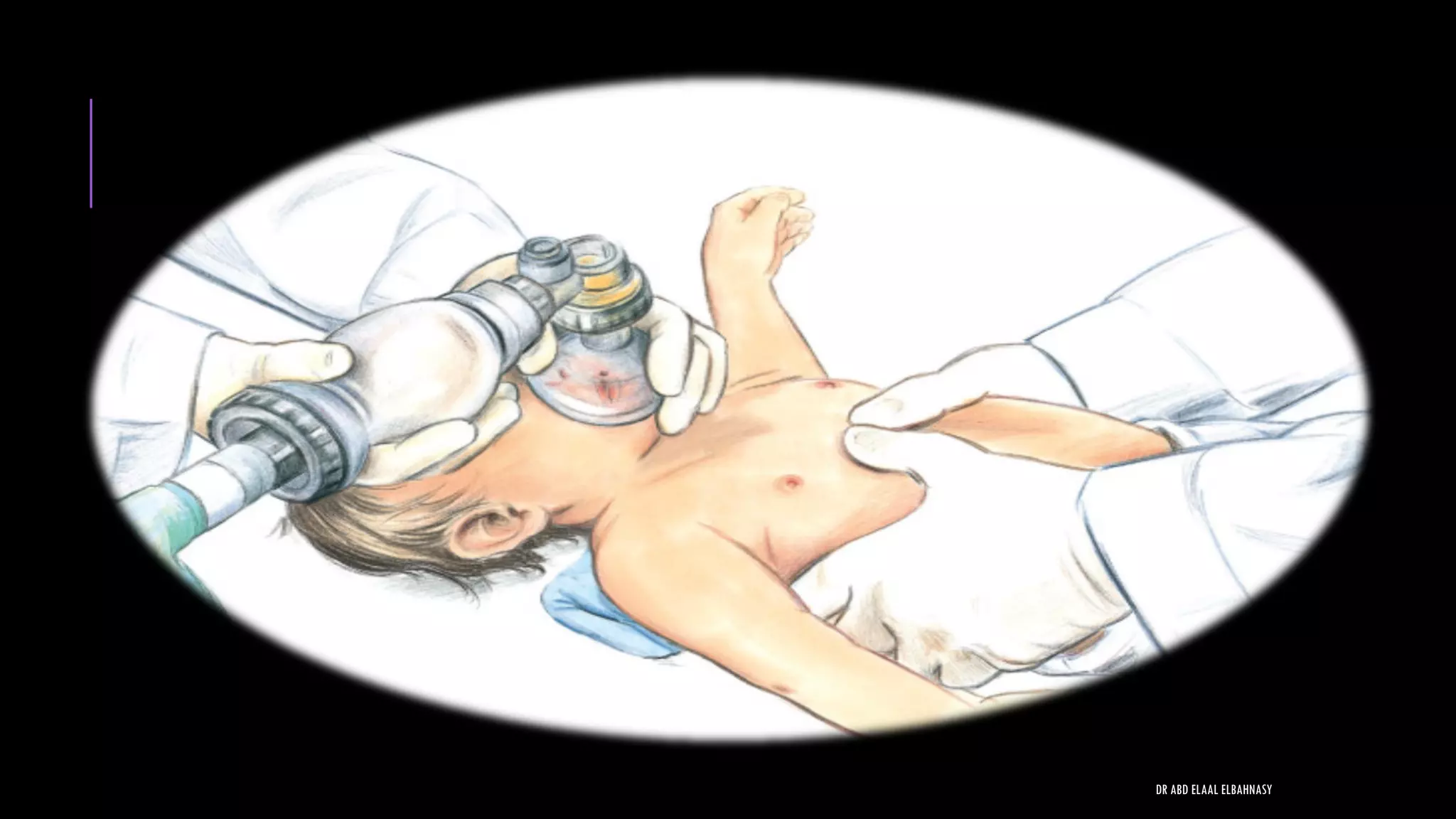
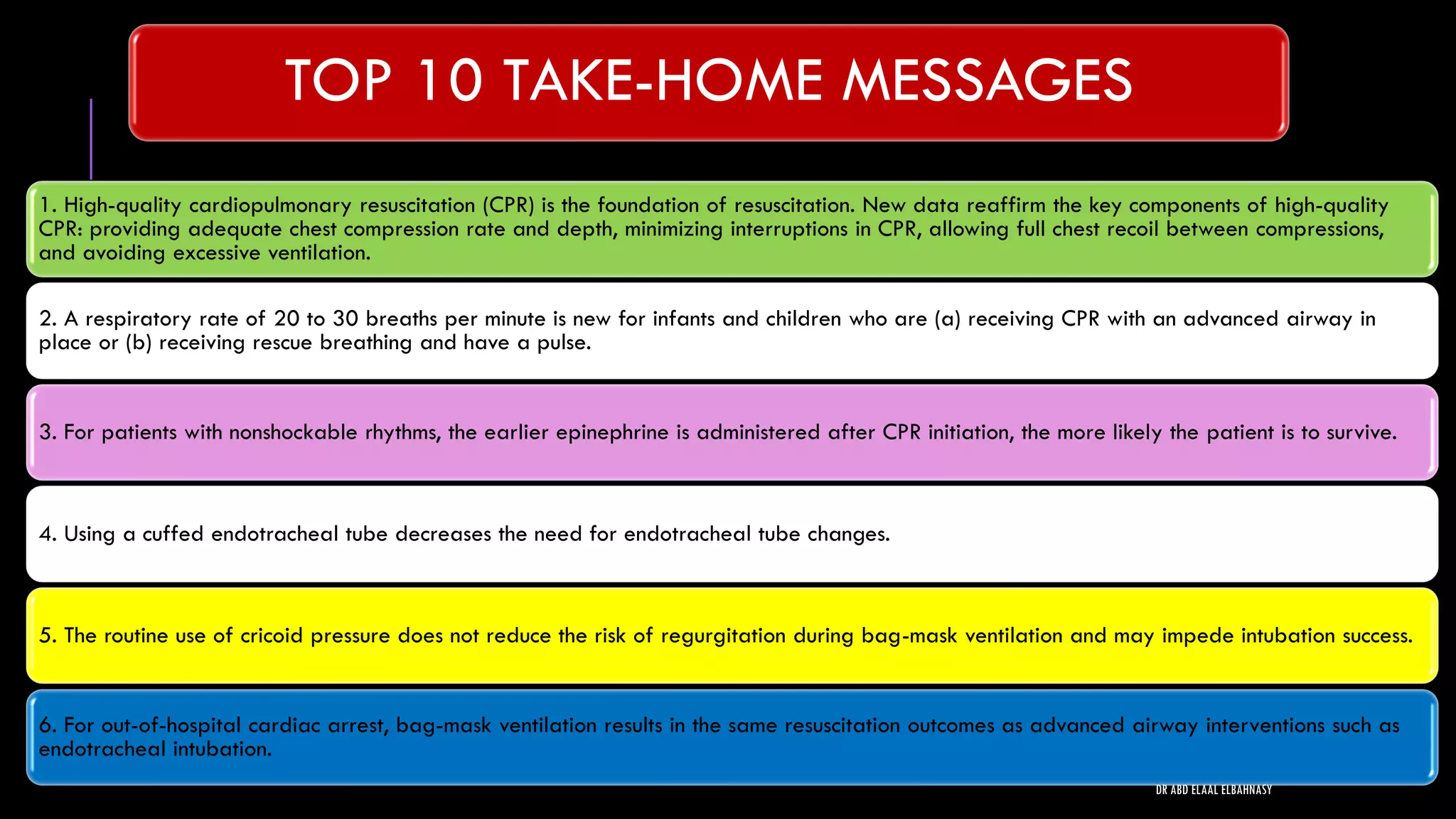
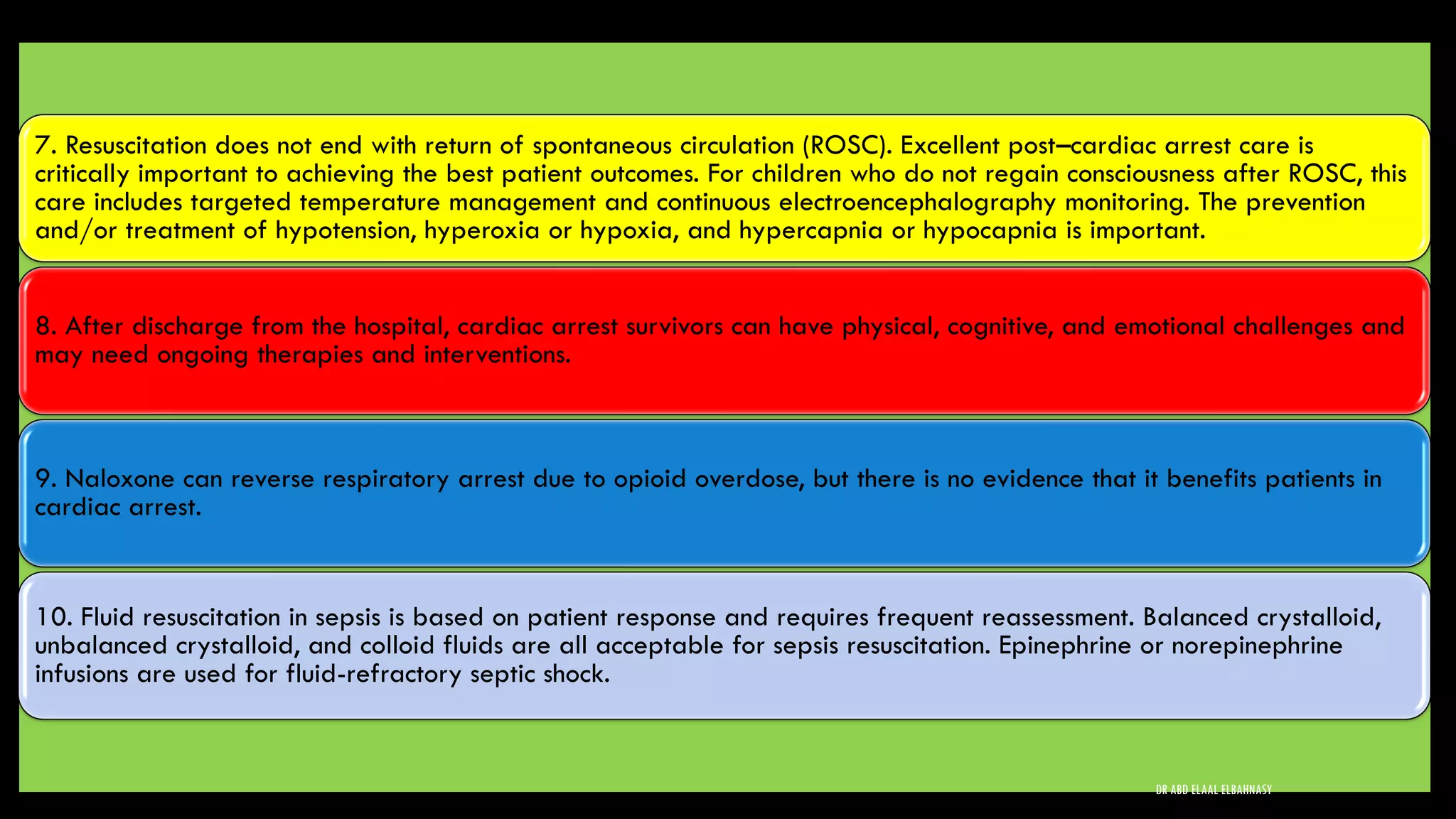
2) High quality CPR is essential and includes adequate chest compressions, optimal rate, minimizing interruptions, full chest recoil, and avoiding excessive ventilation.
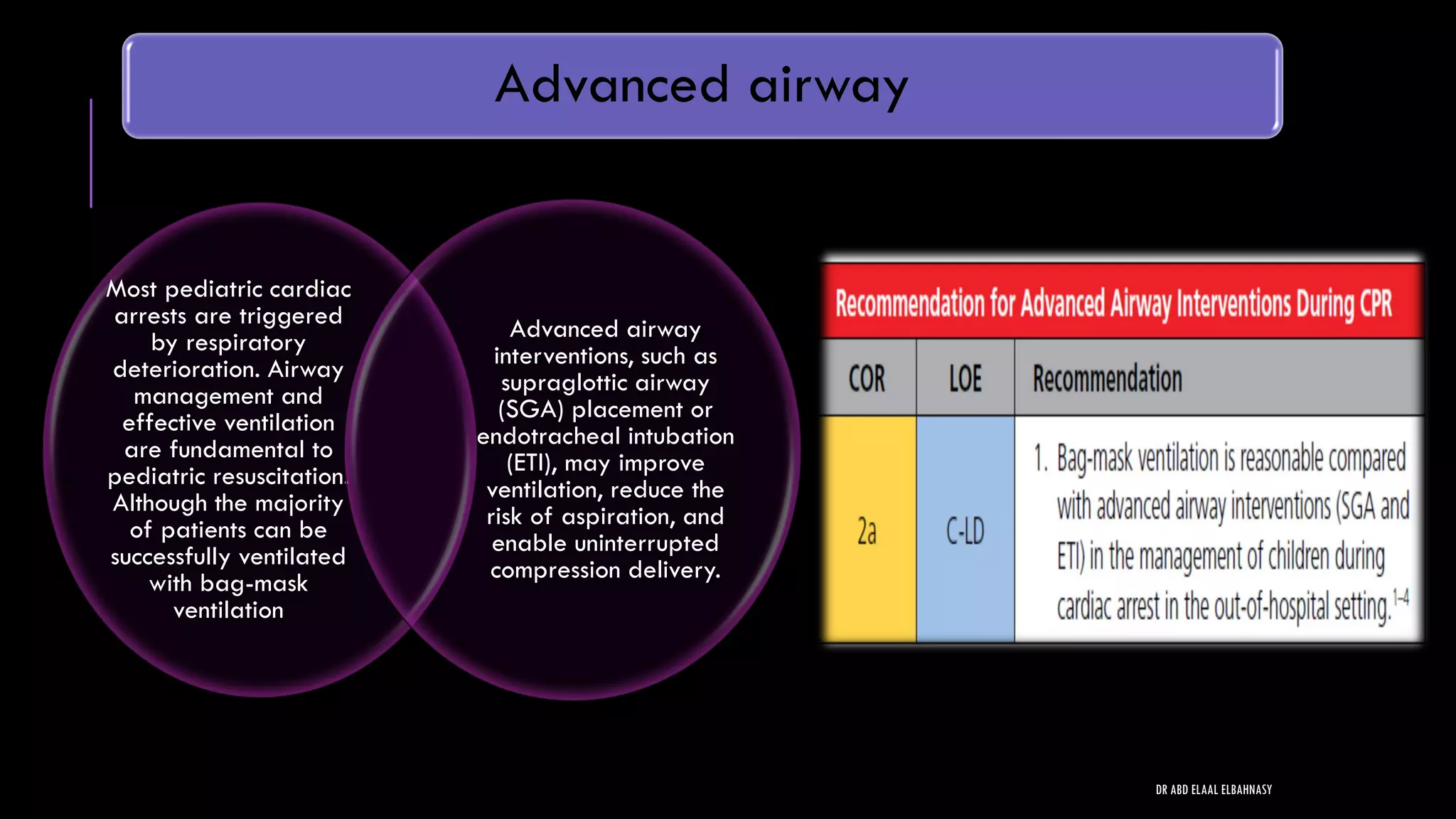
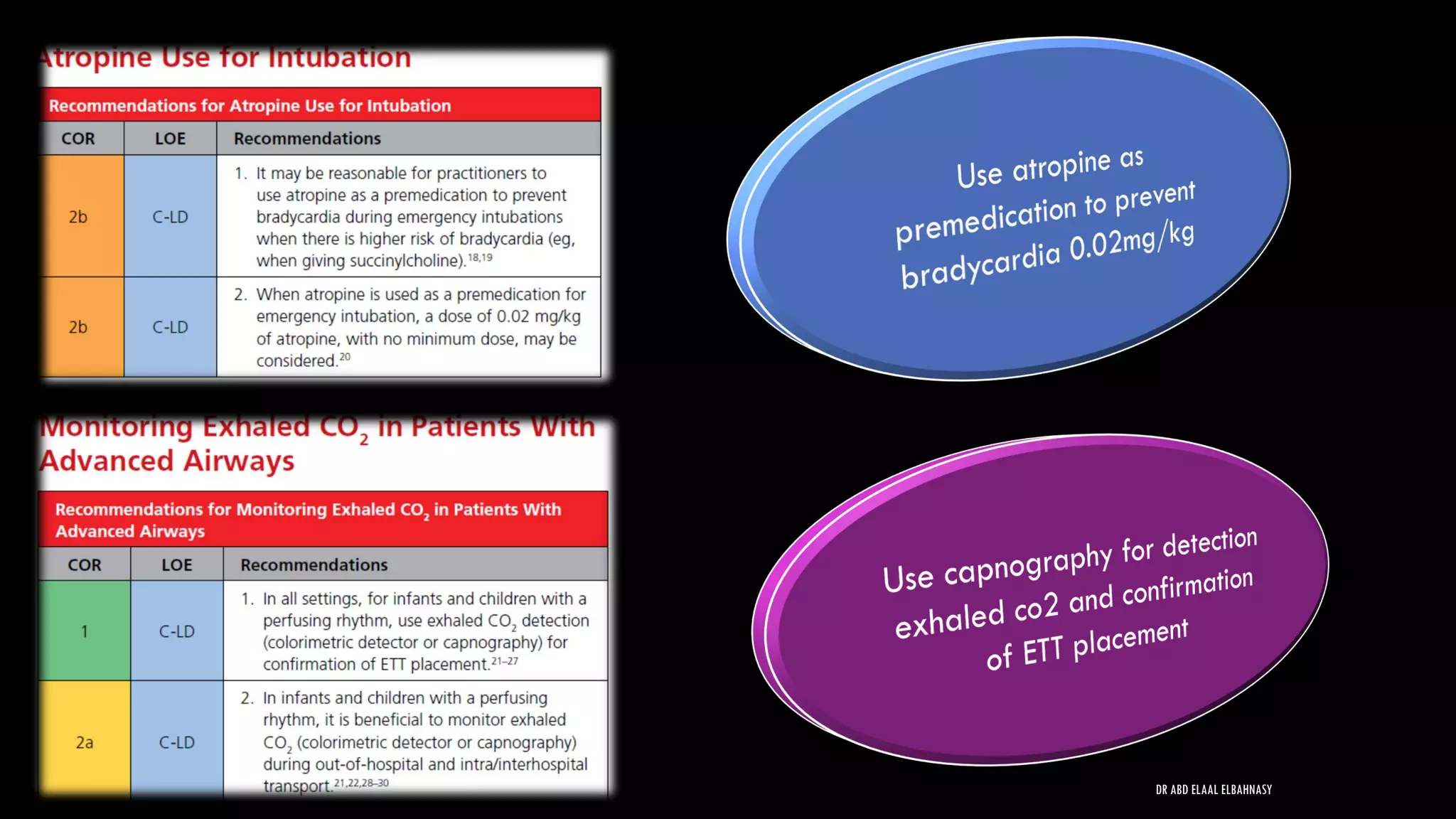
3) Advanced airway interventions like endotracheal intubation can improve ventilation and reduce risks, but are not always necessary for resuscitation. Bag-mask ventilation is often sufficient.