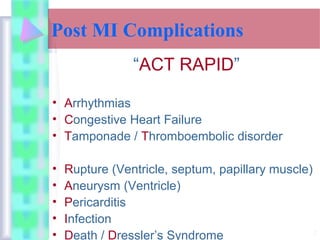
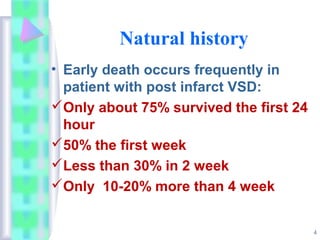
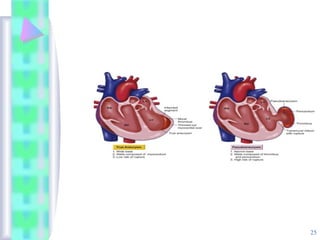
This document discusses surgical treatment of complications from acute myocardial infarction (MI). It describes various complications that can occur post-MI including ventricular septal rupture, papillary muscle rupture, and ventricular free wall rupture which can lead to pseudoaneurysm formation. For each complication, the document outlines signs and symptoms, diagnostic techniques, surgical repair procedures, indications for operation, and factors impacting survival. Early surgical intervention is recommended for complications before additional organ damage or failure occurs.