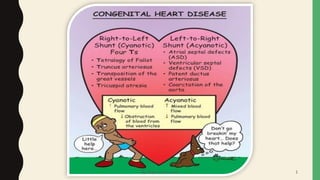
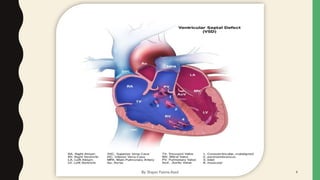
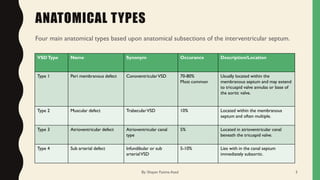
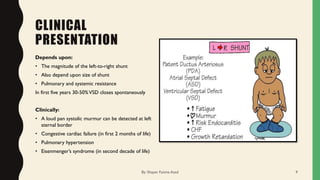
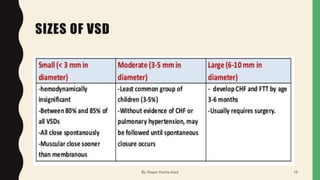
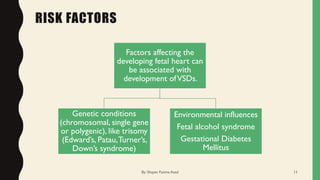
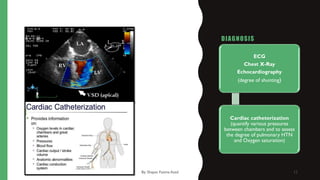
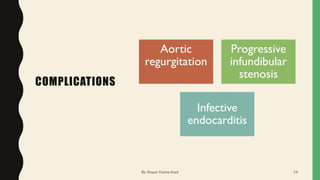
Ventricular septal defect (VSD) is a defect in the wall separating the left and right ventricles of the heart. There are four main types of VSD based on location. A VSD allows blood to flow from the left ventricle to the right ventricle, overloading the right ventricle and lungs. Symptoms depend on the size of the shunt but can include heart failure, pulmonary hypertension, and abnormal heart sounds. VSDs are typically diagnosed via echocardiogram and may close on their own, though large defects often require surgical closure to prevent complications later in life. With treatment, long-term prognosis is excellent.