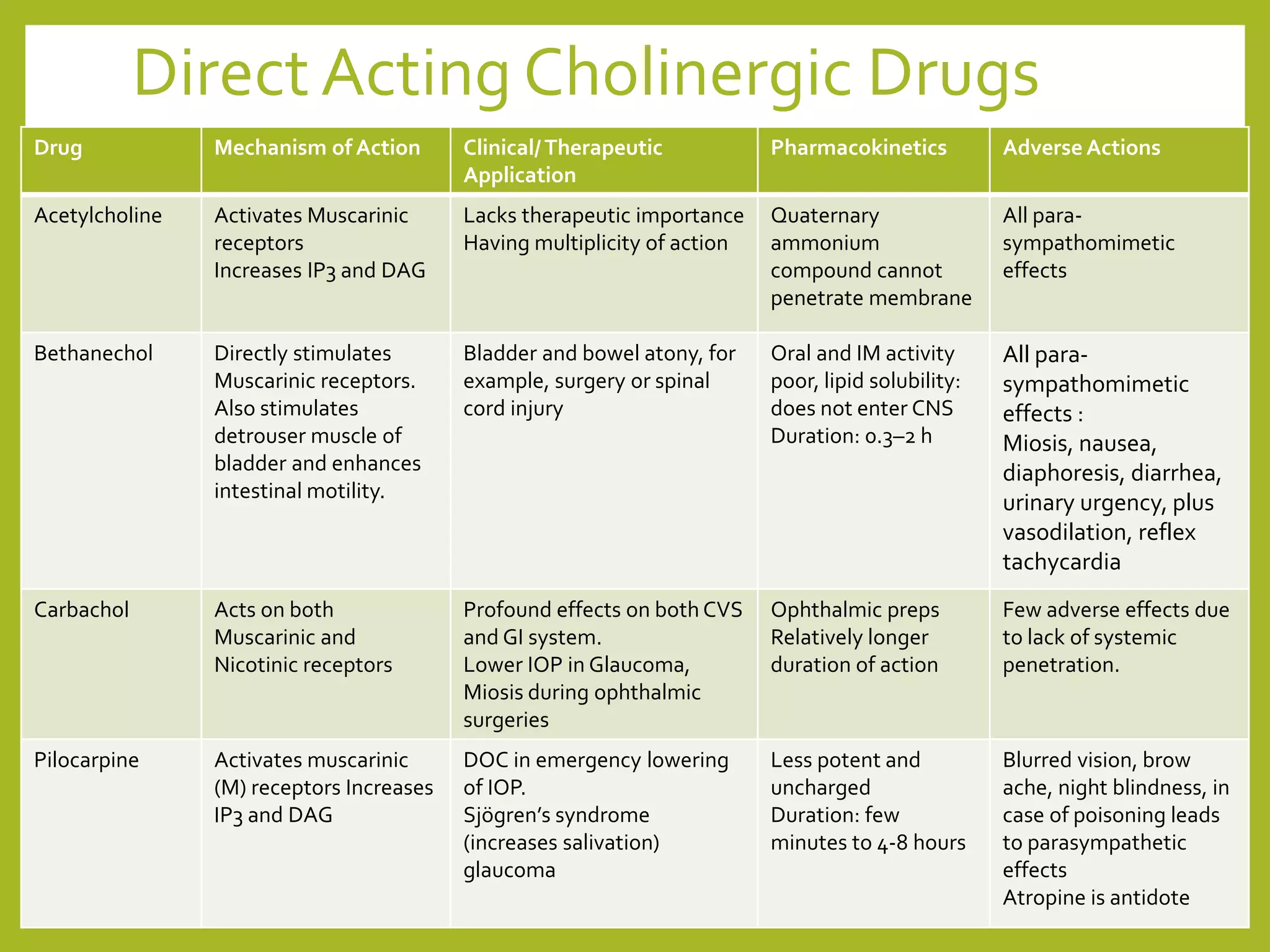
This presentation covers cholinergic drugs, dividing them into cholinergic agonists and antagonists, detailing their mechanisms, therapeutic uses, and adverse effects. It discusses various classifications, including direct-acting and indirect-acting agonists, and highlights the synthesis and action of acetylcholine. The document also touches on the toxicology of anticholinesterase agents and outlines the applications of both cholinergic and anticholinergic drugs in clinical settings.