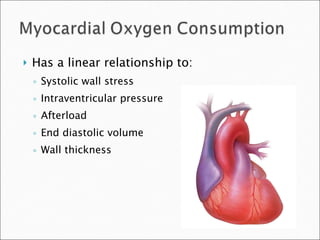
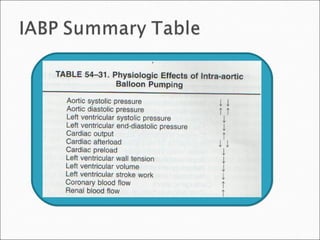
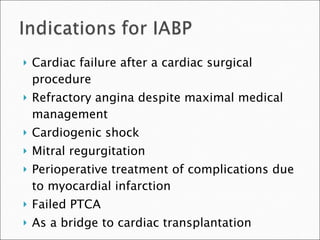
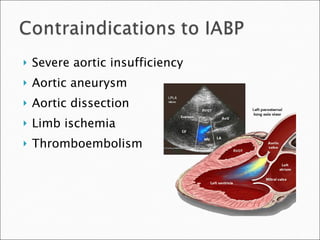
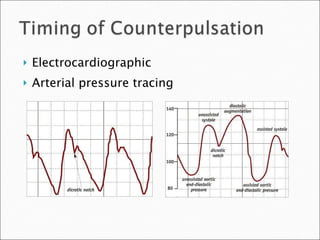
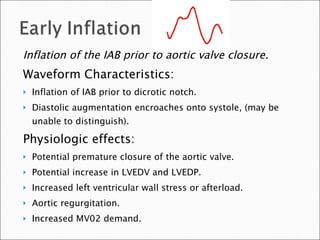
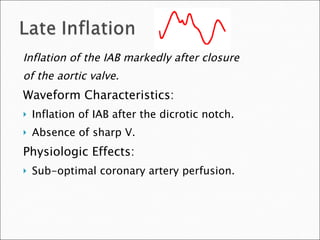
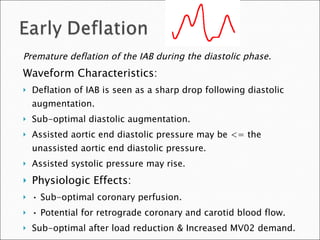
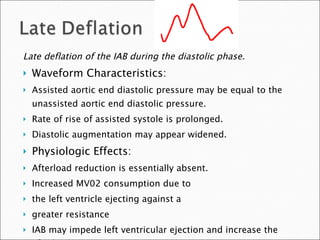
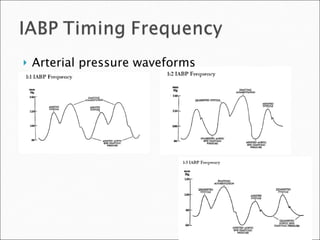
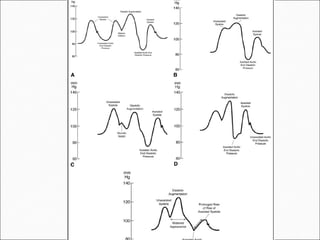
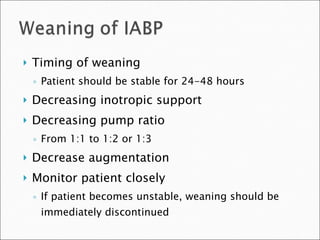
The document discusses the use of an intra-aortic balloon pump (IABP), including appropriate timing of inflation in the cardiac cycle, risks of premature or late deflation, and guidelines for weaning a patient from the device. It notes that the IABP has applications in cardiac failure, refractory angina, cardiogenic shock, and as a bridge to transplantation. Risks include limb ischemia, thrombosis, emboli, bleeding, and aortic complications. Weaning should occur over 24-48 hours with decreasing inotropic support and pump ratios monitored closely.