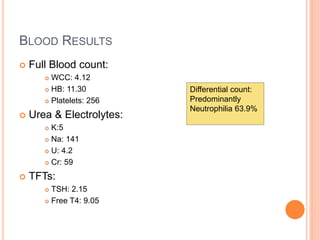
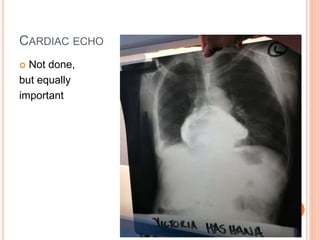
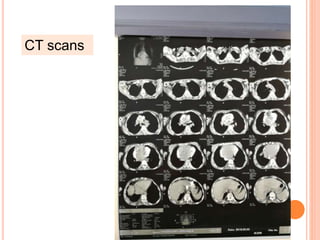
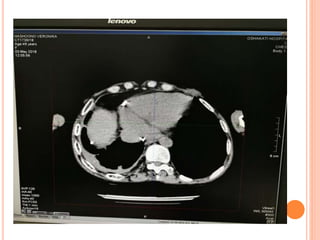
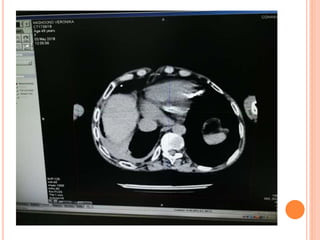
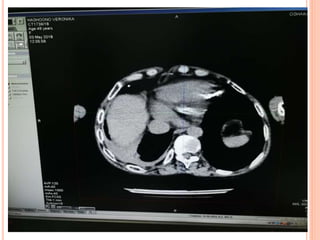
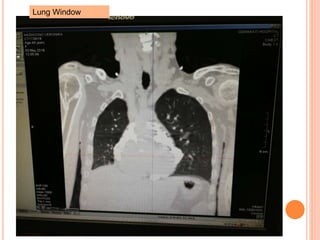
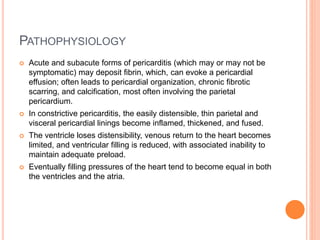
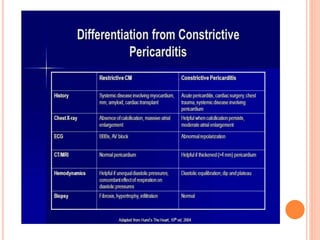
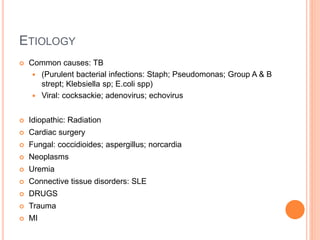
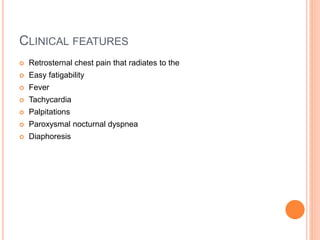
This case involves a 58-year-old female presenting with bilateral foot swelling for 8 weeks, central chest pain for 4 weeks, and heart palpitations for 4 weeks. Her history and examination are consistent with constrictive pericarditis. Key findings include elevated JVP, muffled heart sounds, and signs of chronic liver disease. Constrictive pericarditis occurs when chronic inflammation leads to a thickened, fibrotic pericardium that restricts cardiac filling. Common causes are tuberculosis, other infections, radiation, and idiopathic. Definitive treatment is pericardiectomy, while medical management may be considered for less severe cases.