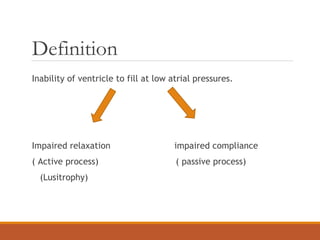
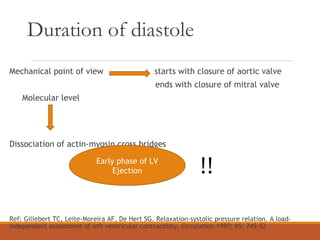
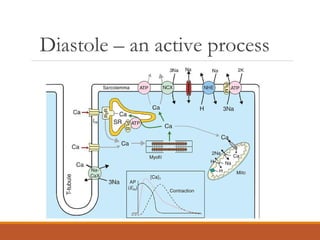
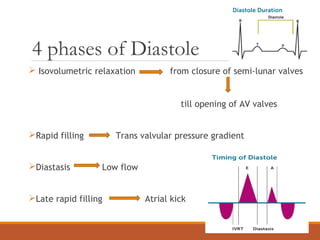
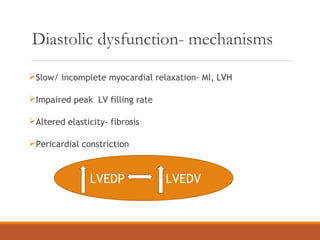
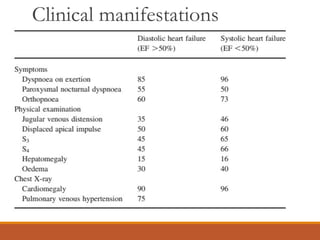
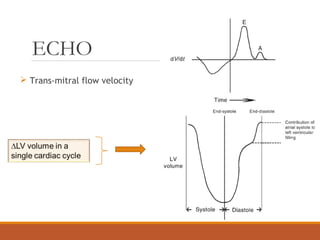
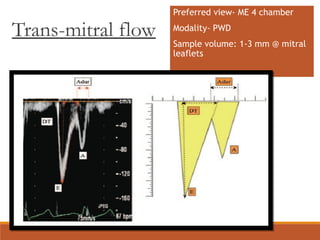
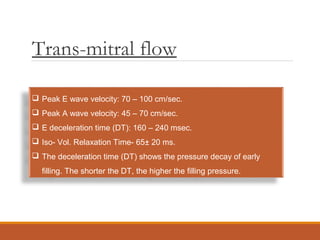
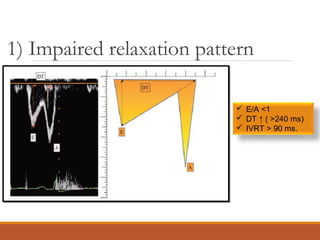
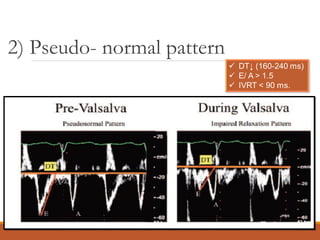
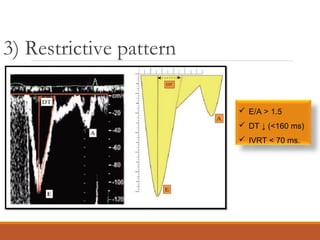
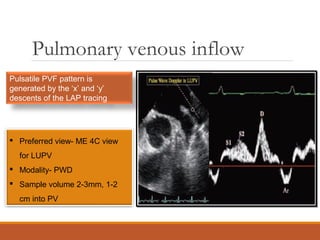
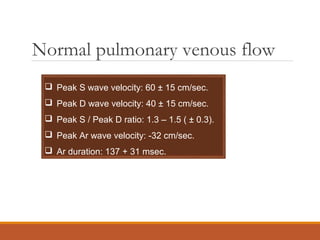
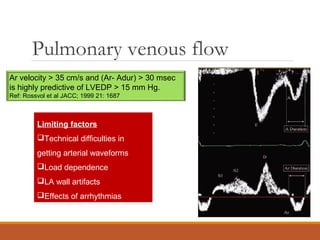
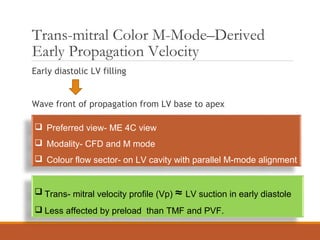
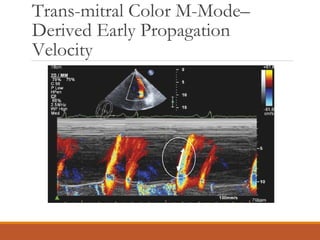
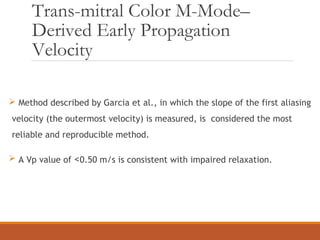
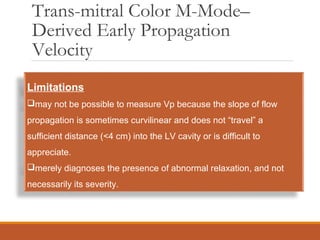
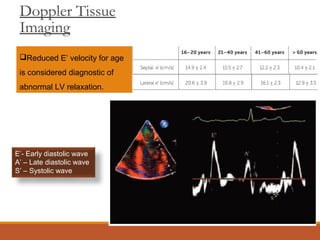
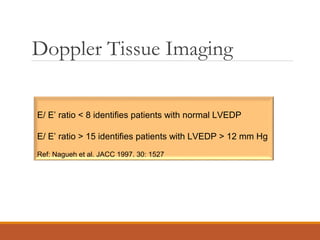
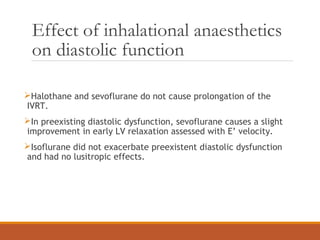
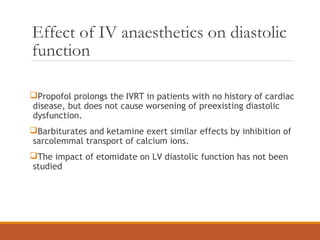
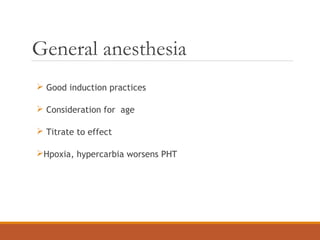
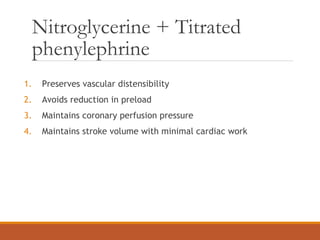
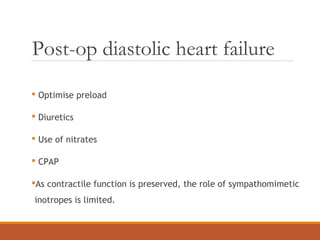
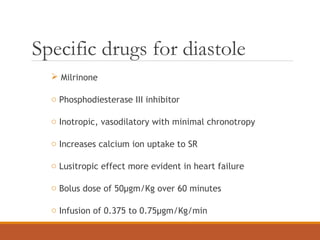
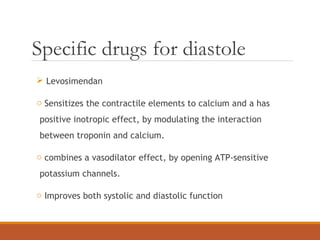
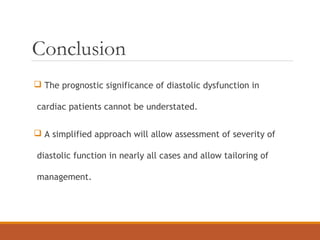
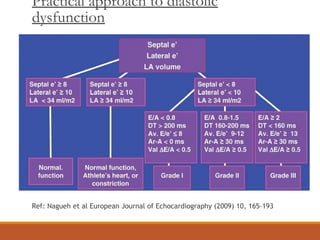
This document discusses diastolic dysfunction, its diagnosis using echocardiography, and anesthetic considerations. It defines diastolic dysfunction as the inability of the ventricle to fill at low atrial pressures. The key aspects of diastolic function evaluation by echocardiography include trans-mitral flow patterns, pulmonary venous flow, tissue Doppler imaging, and mitral annular velocities. Anesthetic goals are to maintain preload and afterload while avoiding drugs that may worsen diastolic function. Specific drugs like milrinone and levosimendan can have beneficial effects on diastolic function in patients with heart failure. Careful preoperative evaluation and postoperative monitoring are important for patients with diast