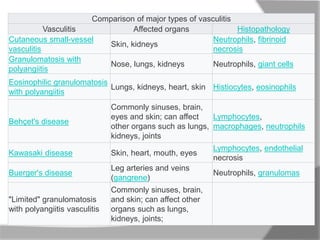
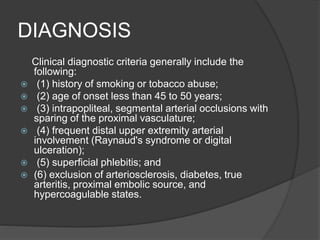
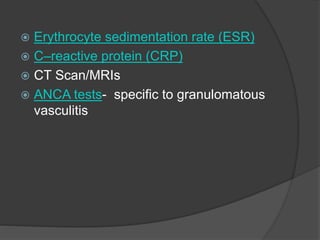
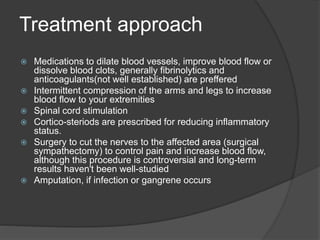
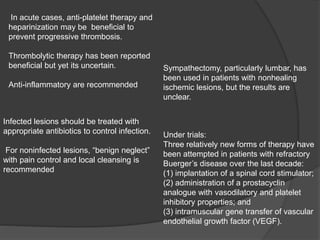
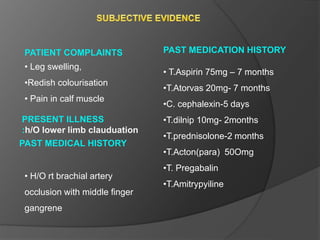
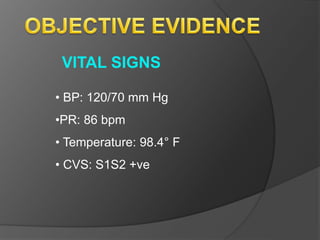
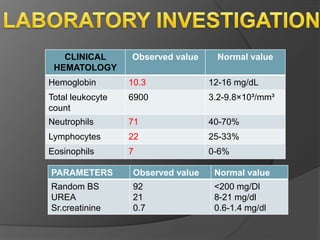
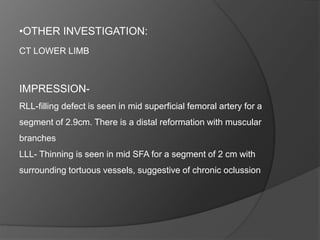
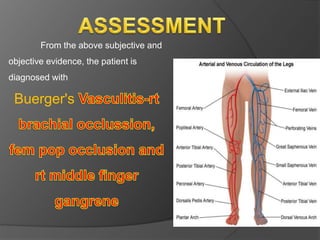
Vasculitis encompasses a range of diseases marked by inflammation of blood vessels, resulting in damage that varies by type and affected organs. Buerger's disease, a notable form, is triggered mainly by tobacco use and leads to painful thrombosis in the limbs, often requiring surgical intervention or amputation. Diagnosis includes clinical history and imaging, while treatment focuses on improving blood flow, managing symptoms, and preventing complications.