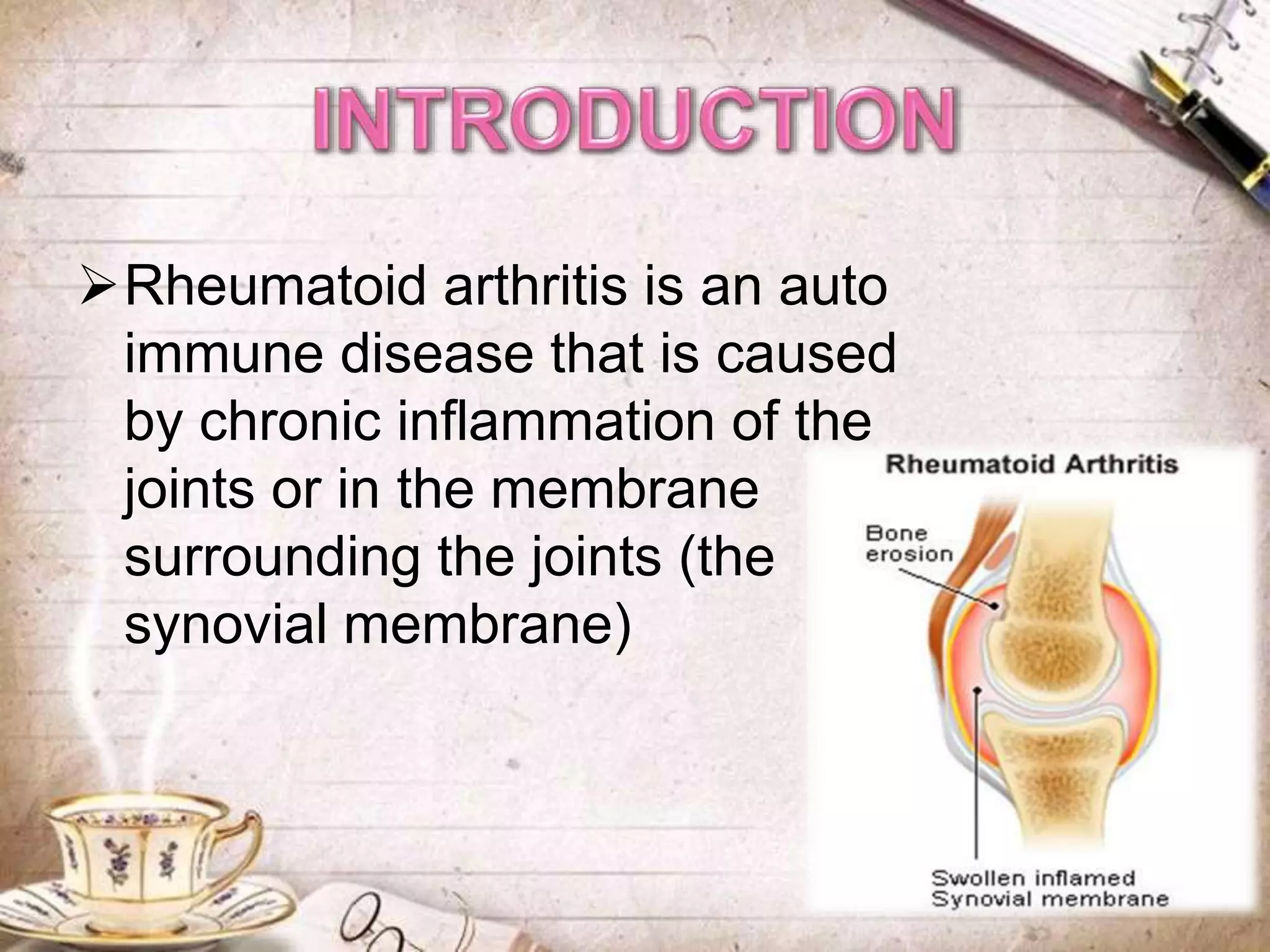
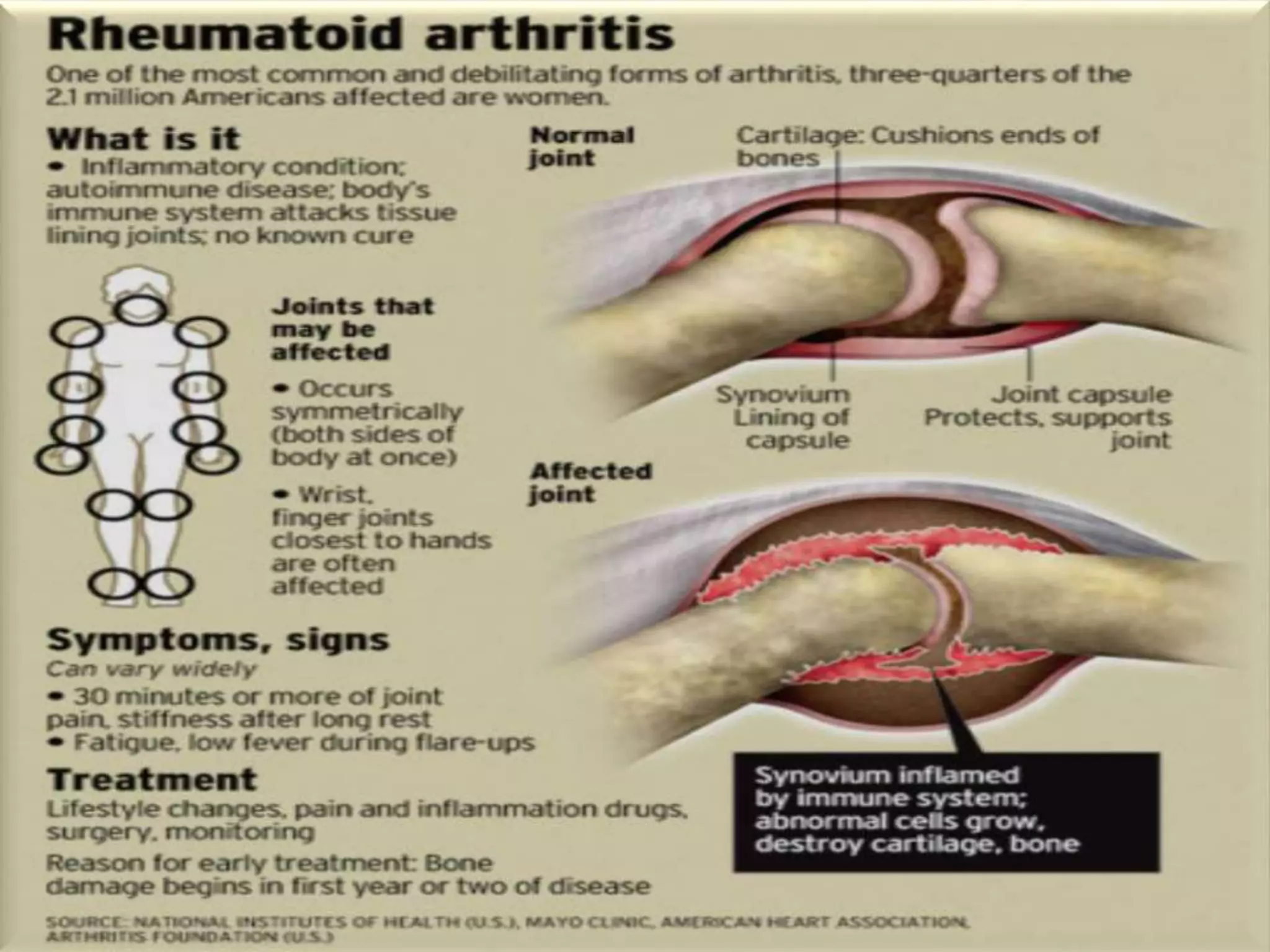
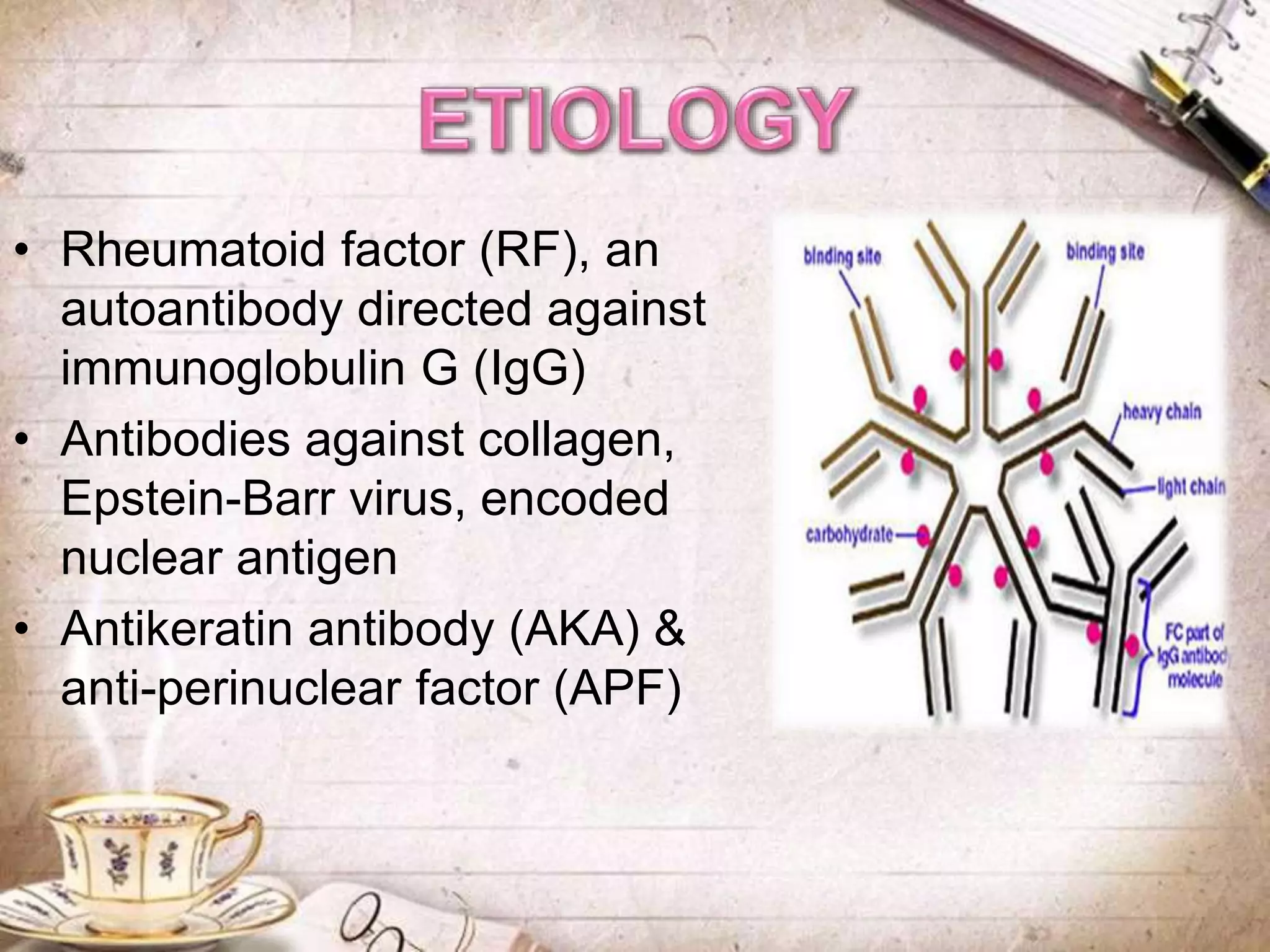
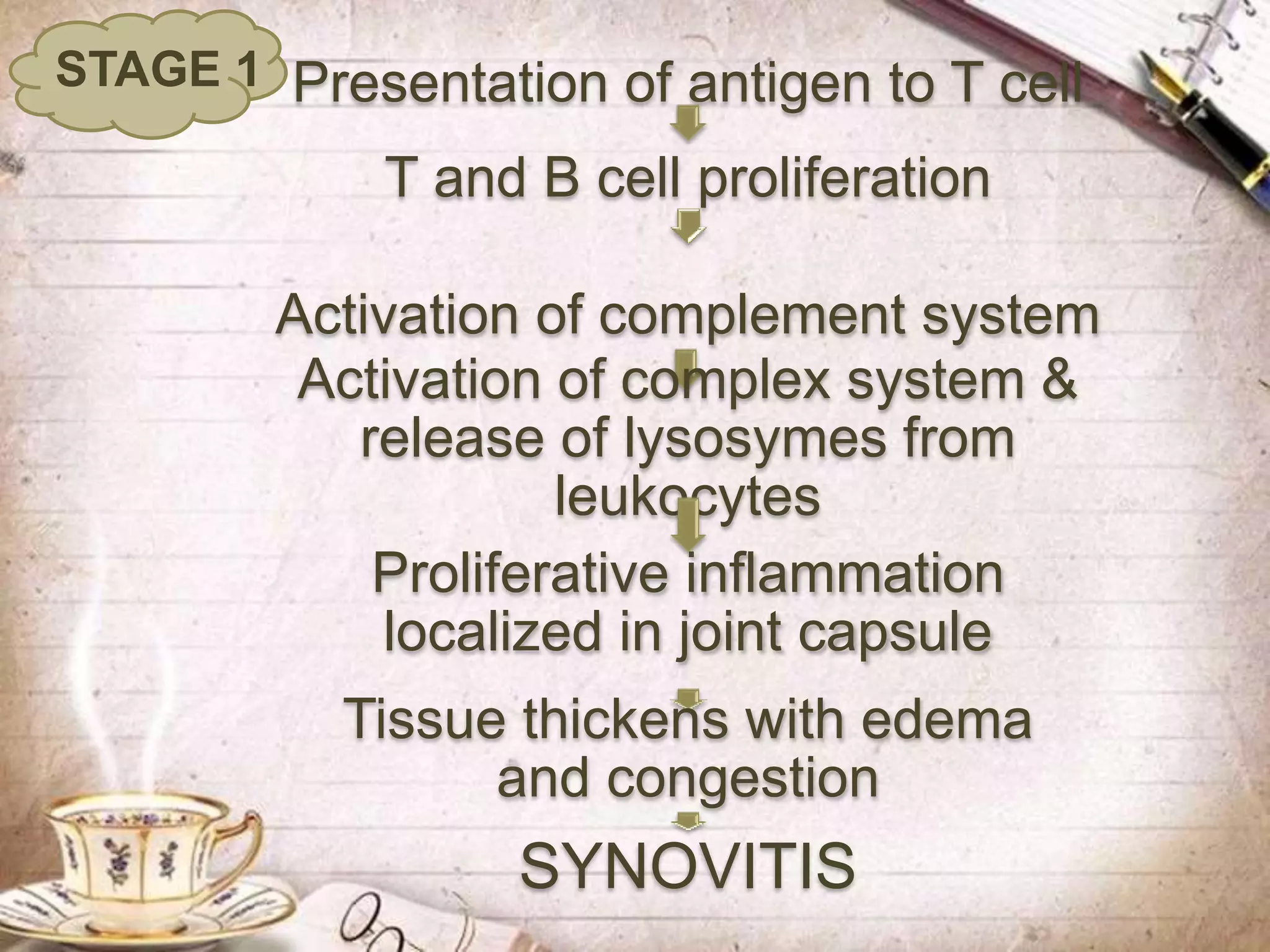
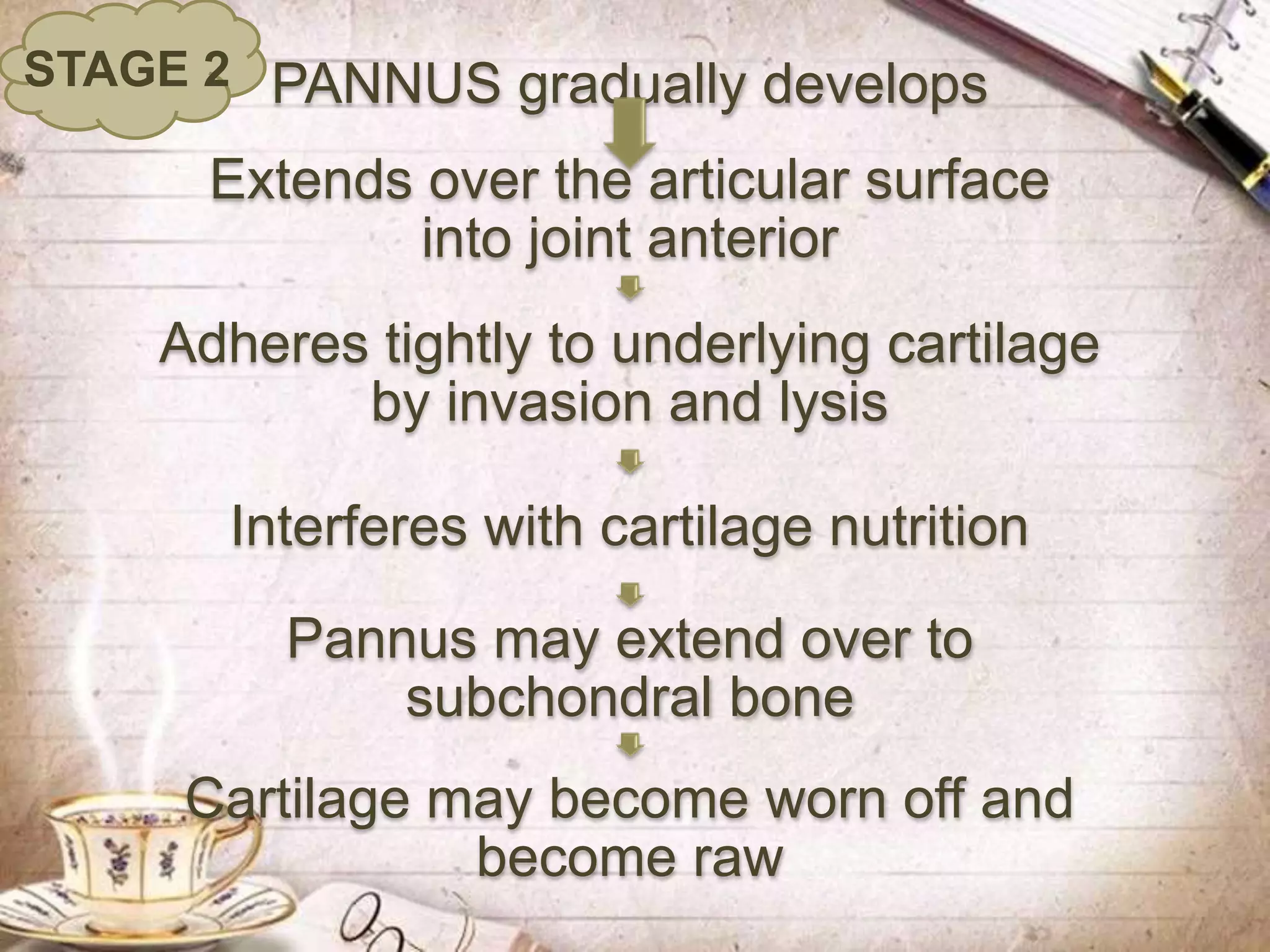
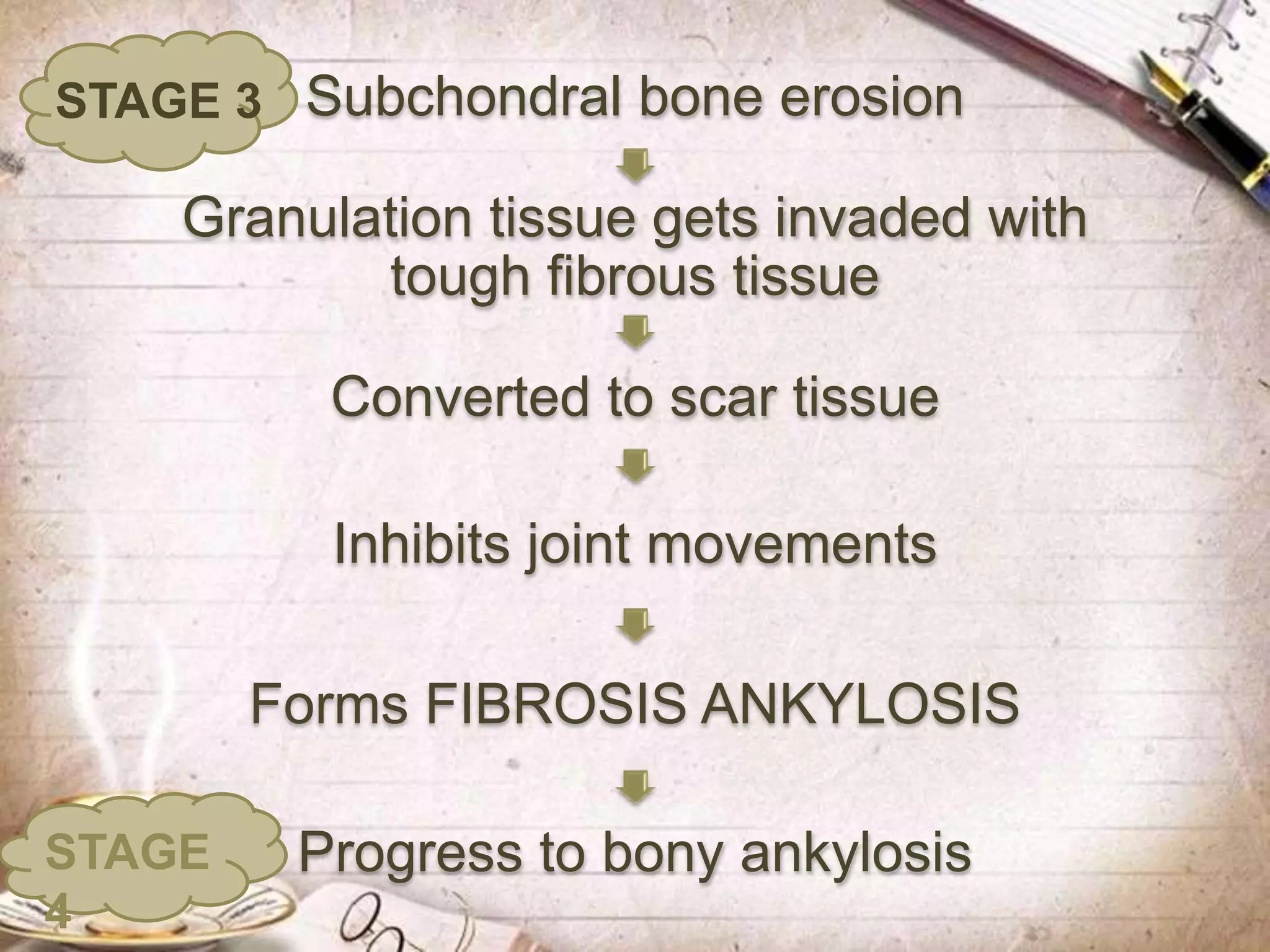
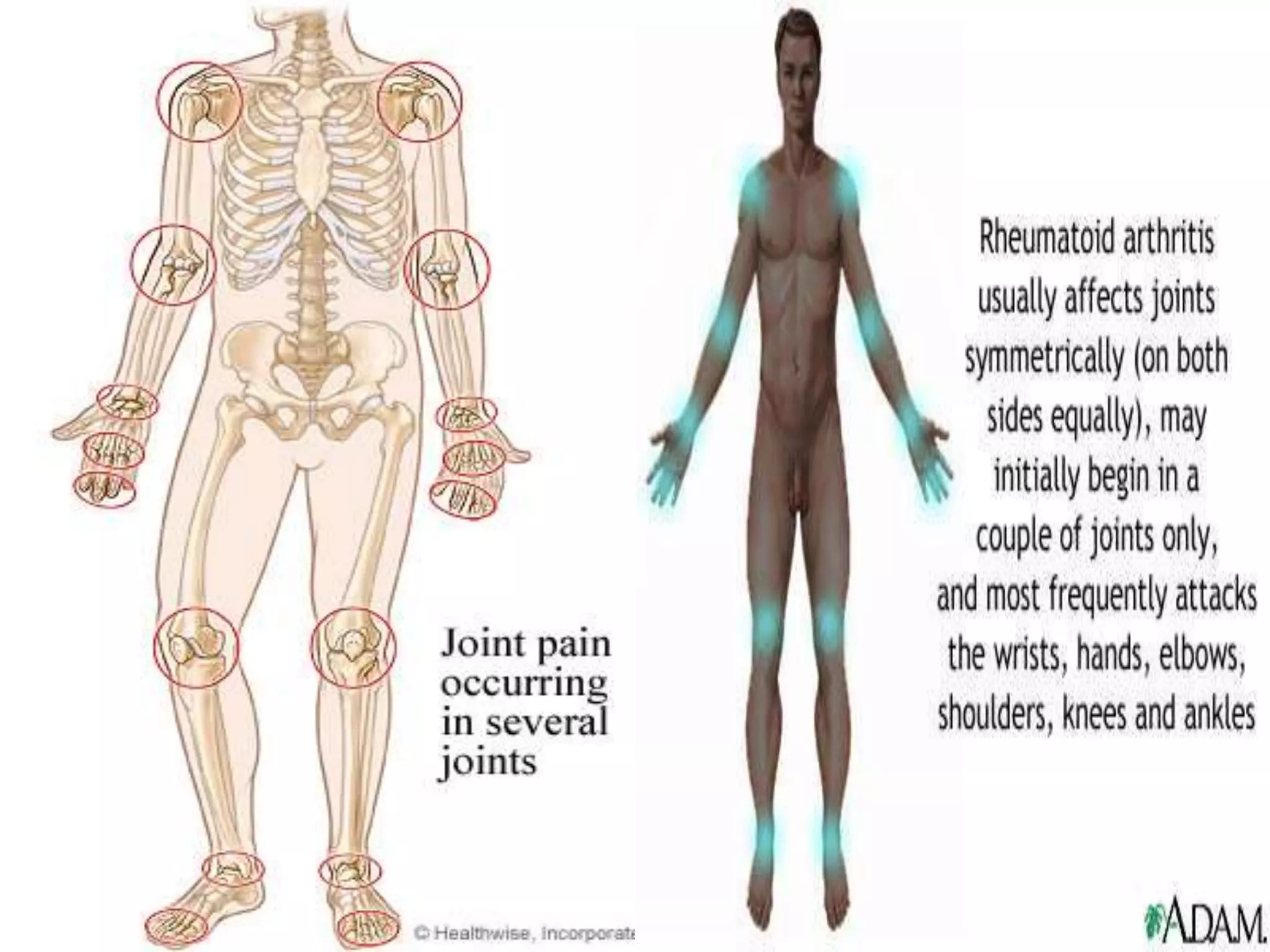
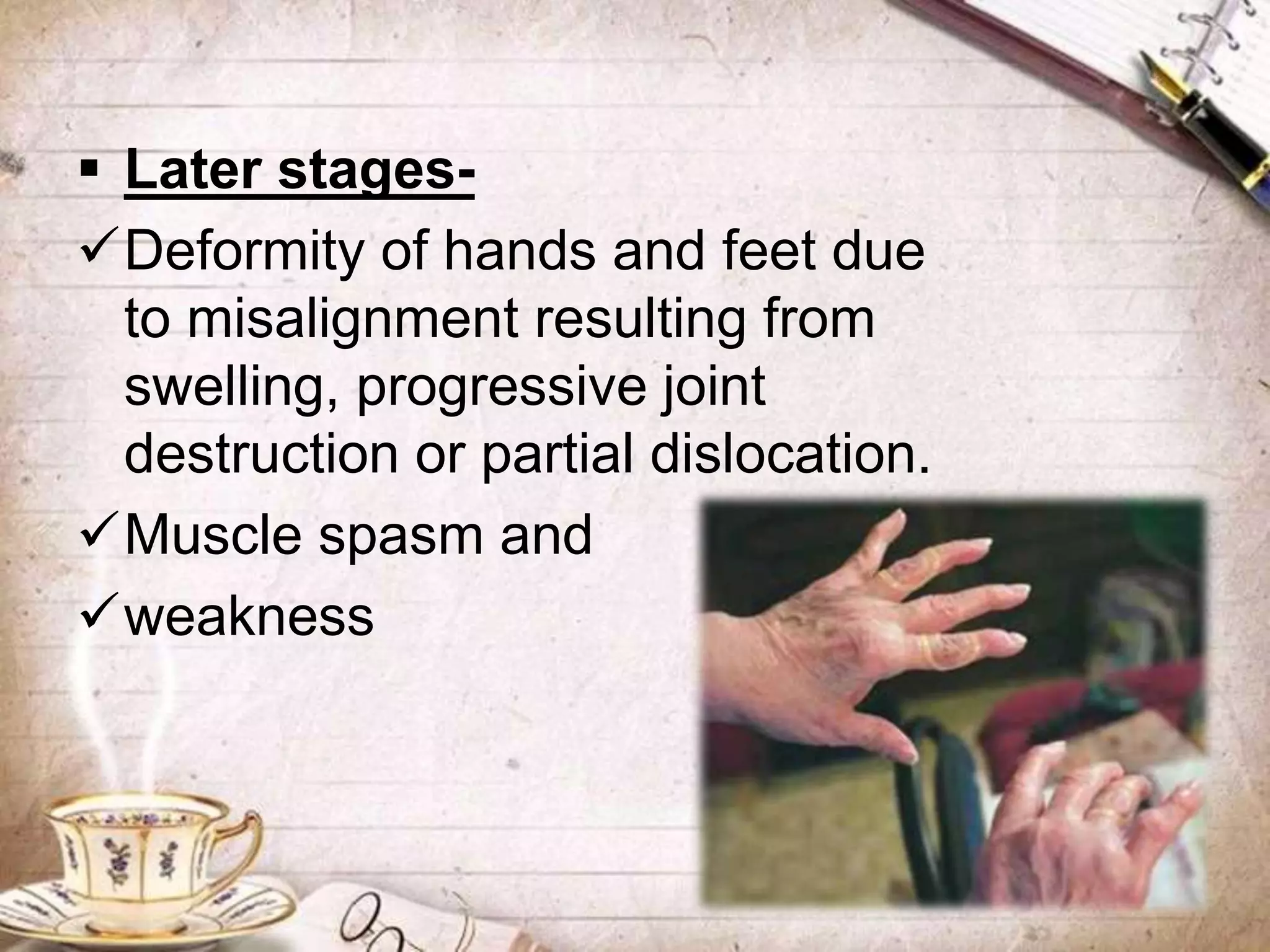
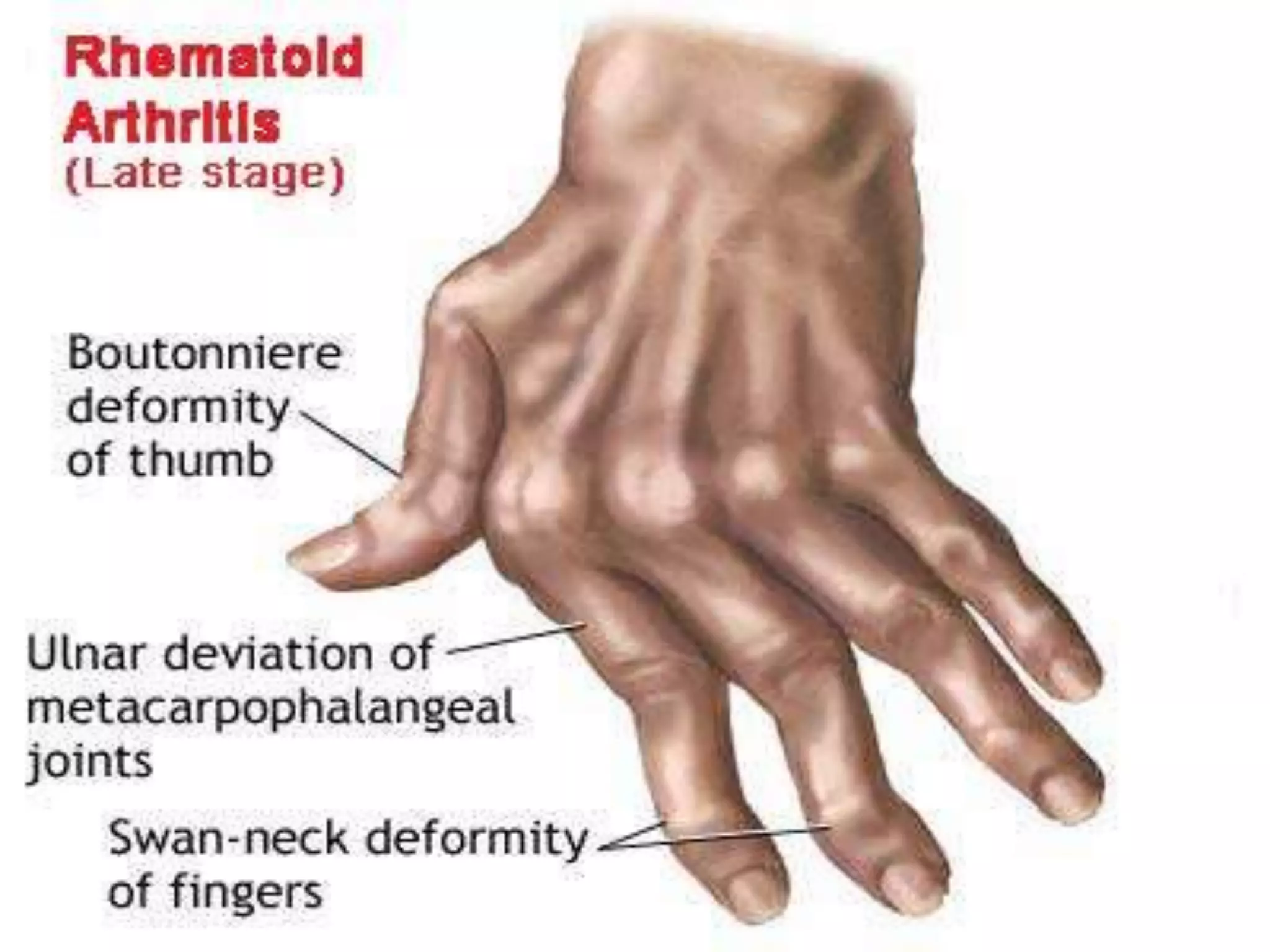
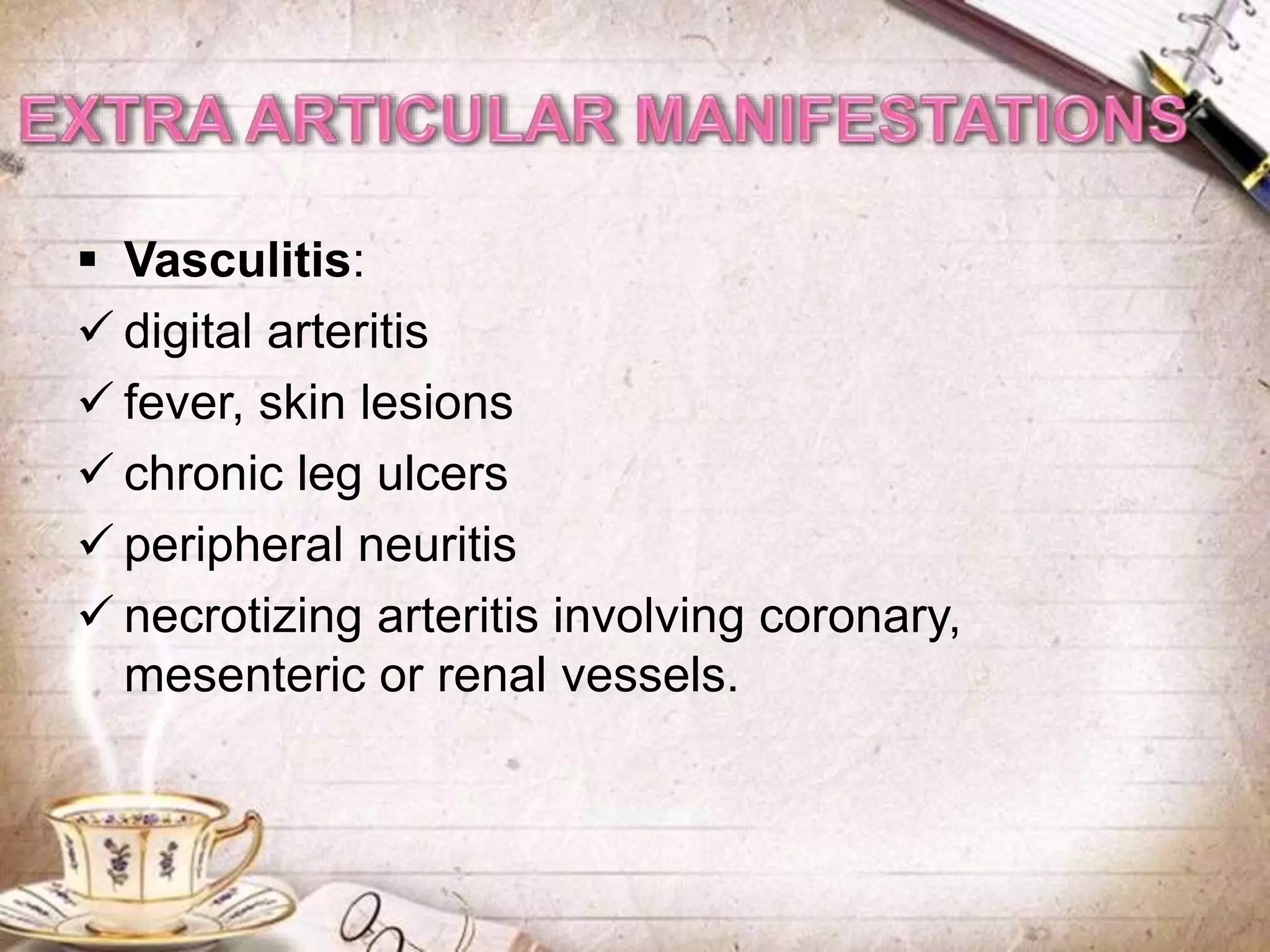
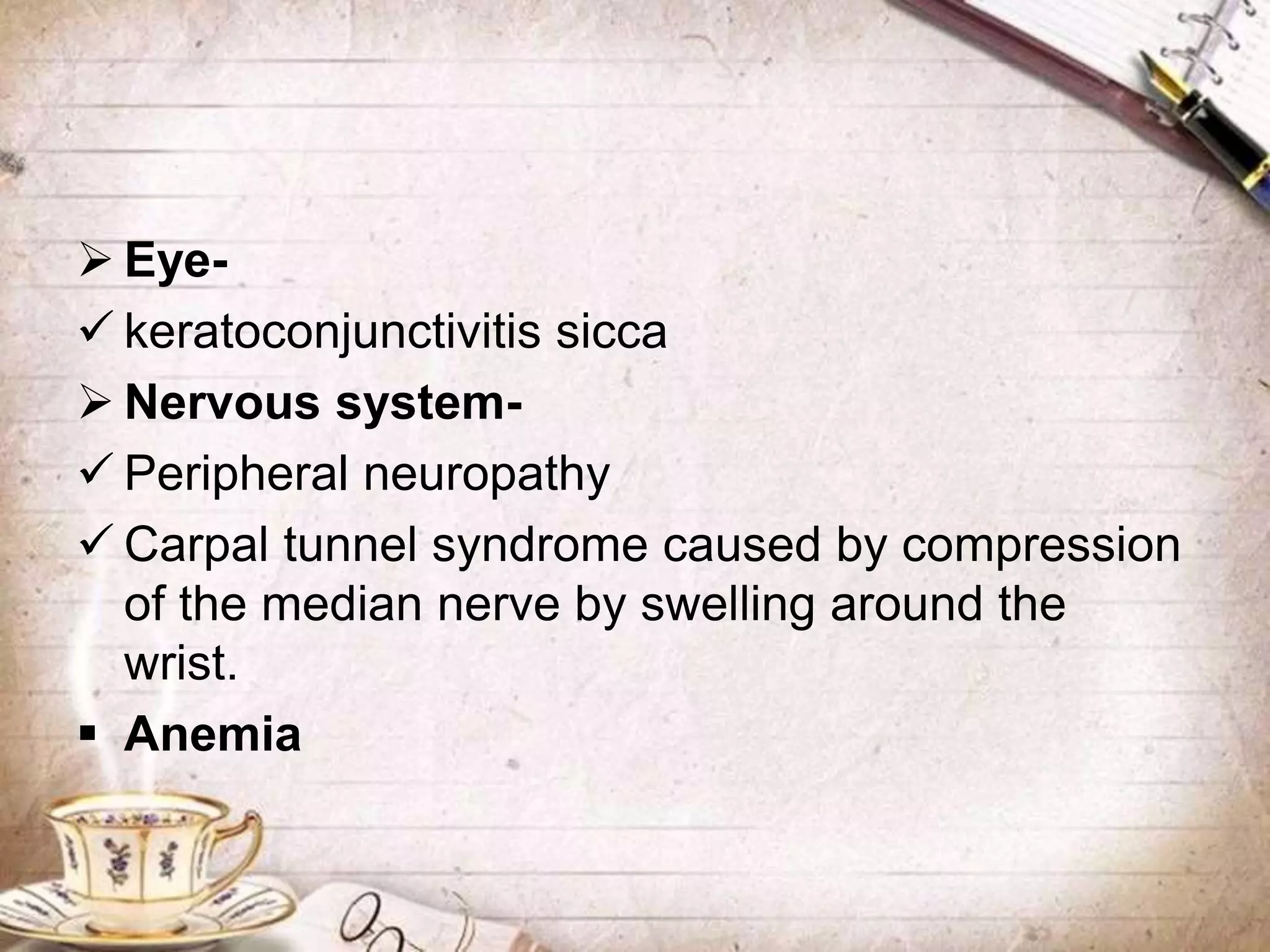
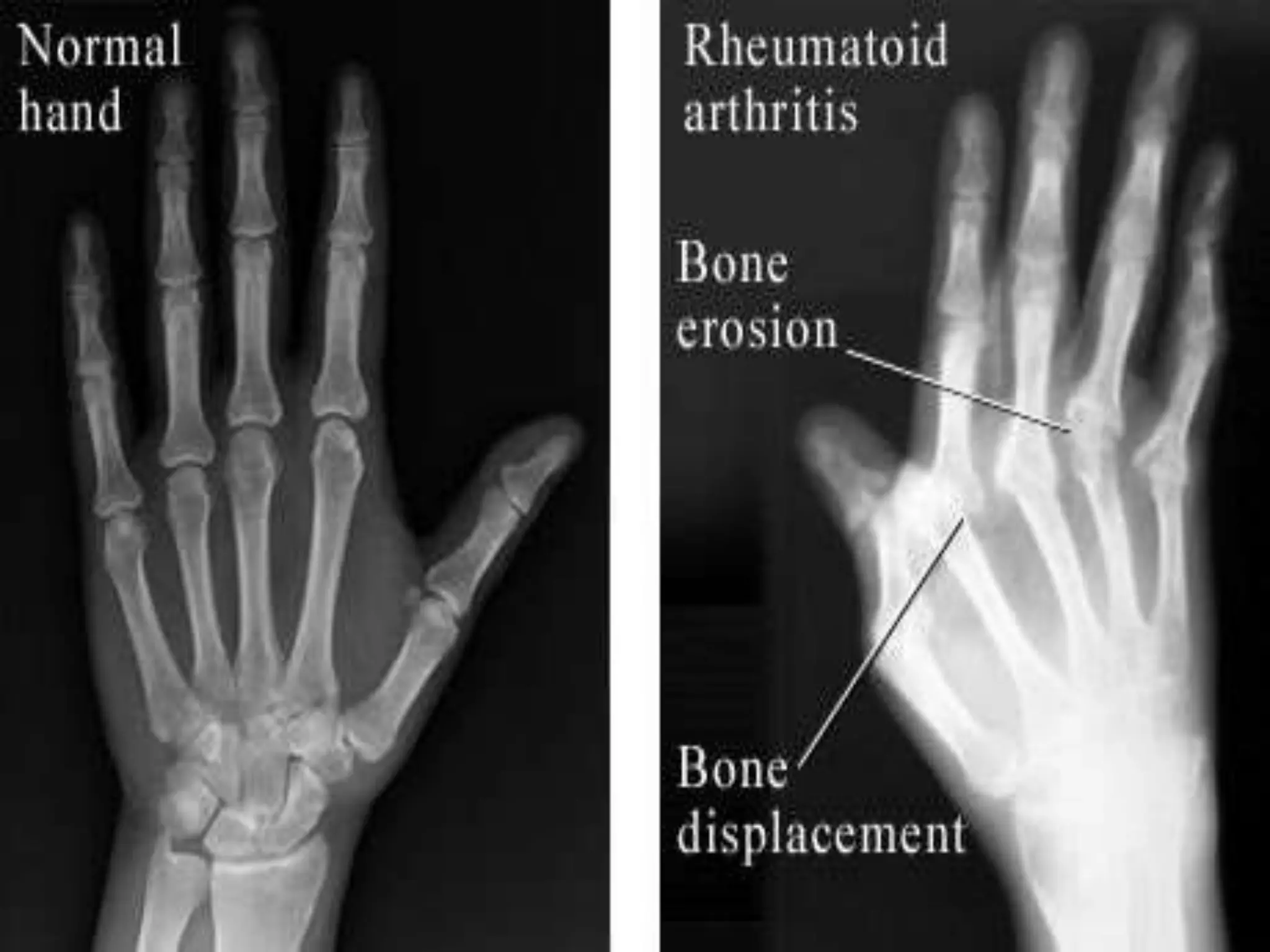
Rheumatoid arthritis (RA) is a chronic autoimmune disorder characterized by symmetrical inflammation of joints, affecting approximately 1% of the population, primarily women aged 20-40. The disease progresses through four stages and can lead to joint destruction and extra-articular manifestations such as anemia and lung fibrosis. Management includes medical treatments to control inflammation and surgical interventions to restore joint function.