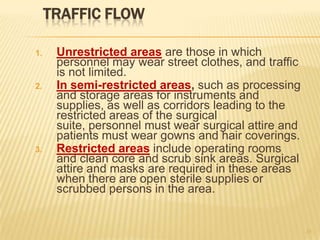
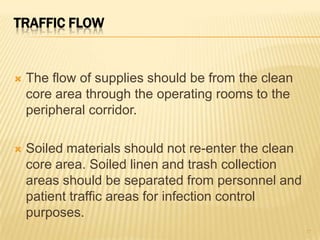
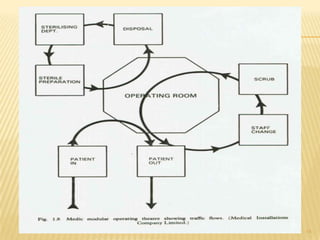
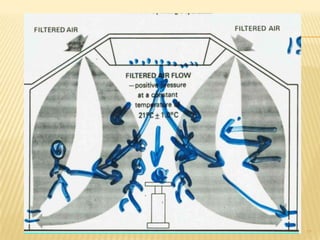
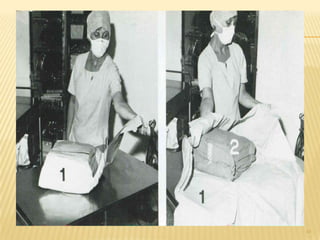
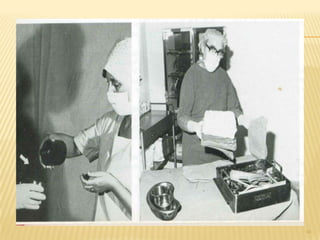
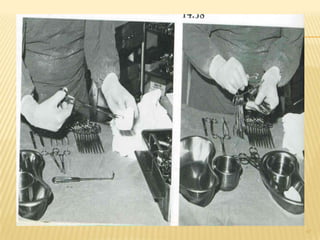
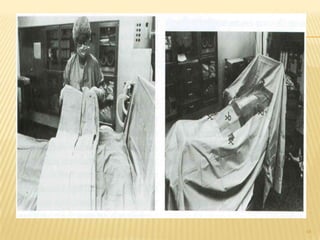
The document discusses operating theater design considerations for infection prevention. It outlines key features of super-specialty and general operating theaters including ventilation systems with minimum air changes per hour, positive pressure differentials, air velocities, temperatures and humidity levels. It also describes traffic flow patterns with clean, semi-restricted and restricted zones and emergency signaling systems.