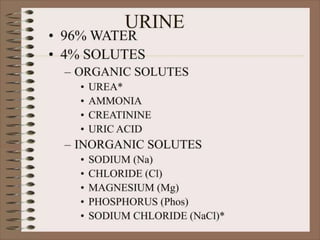
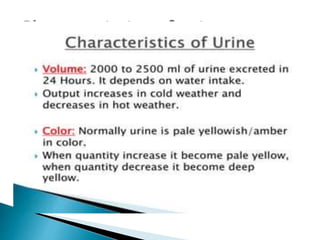
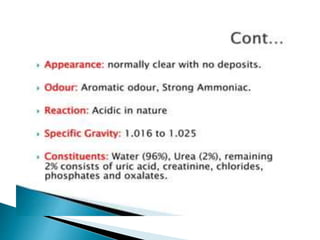
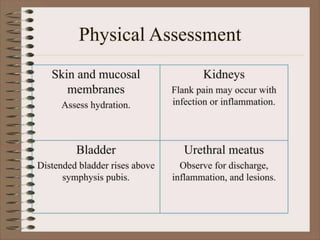
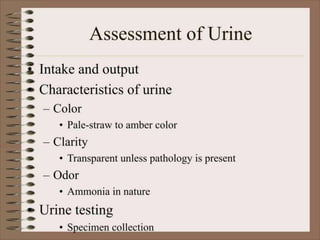
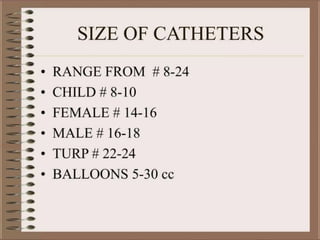
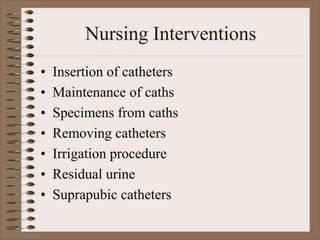
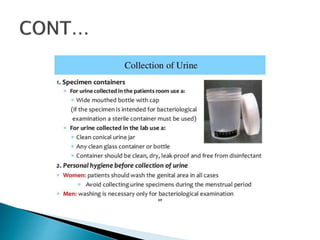
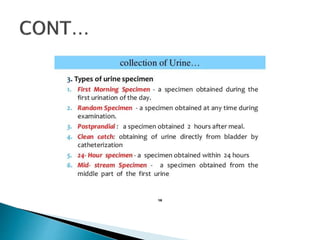
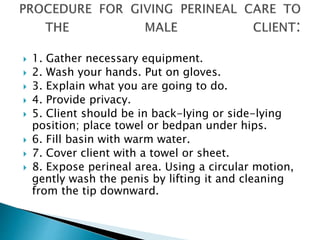
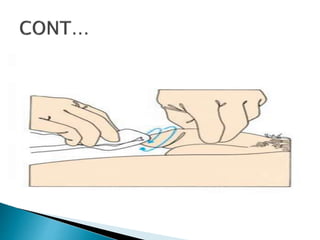
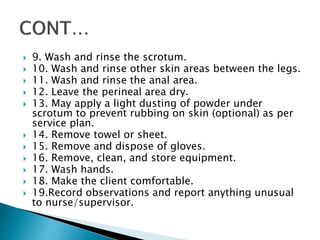
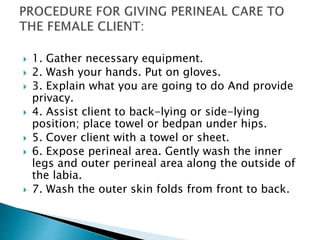
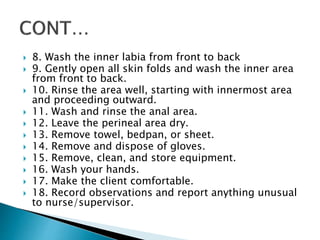
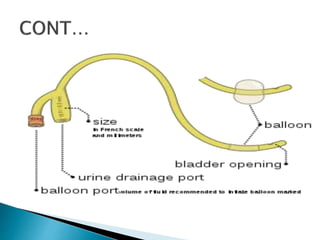
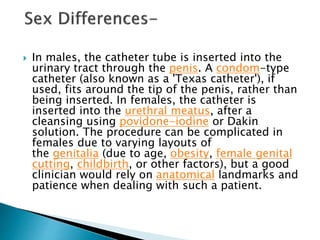
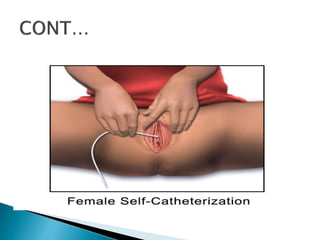
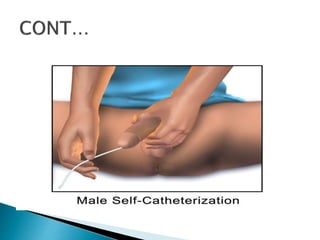
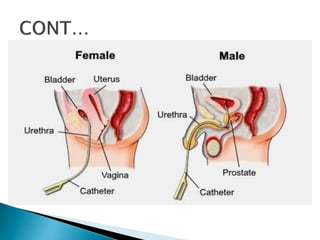
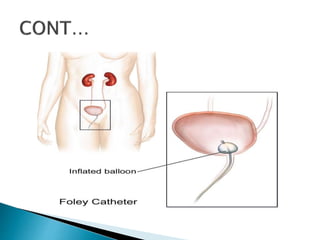
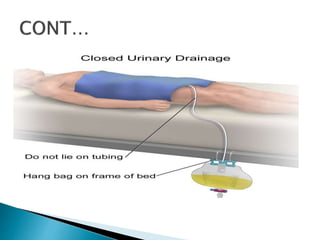
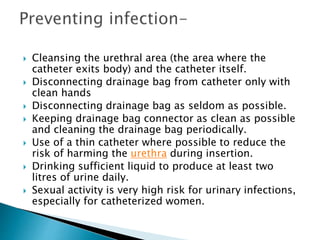
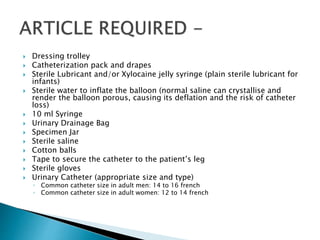
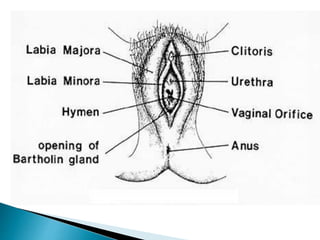
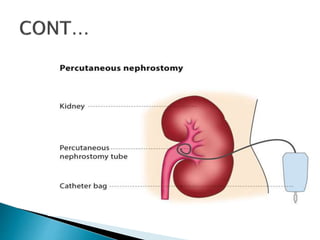
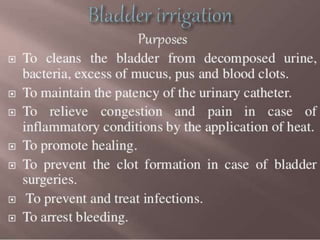
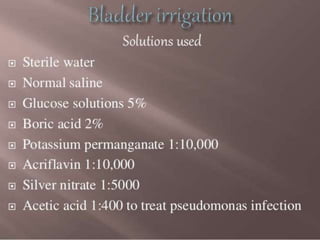
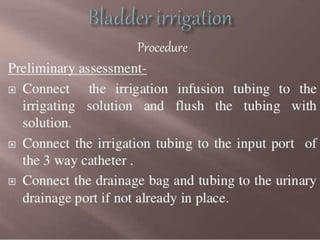
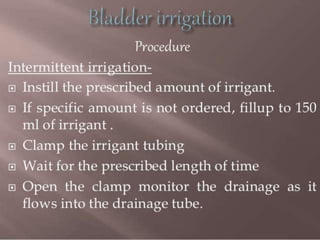
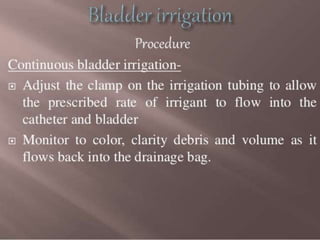
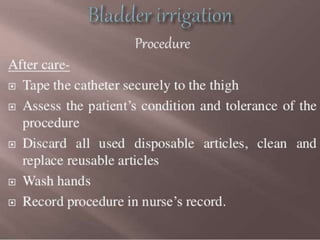
The document discusses various aspects of urinary care, including urine composition, bedpan usage, and perineal care techniques for both male and female patients. It covers the procedures for urinary catheterization, types of catheters, and urinary diversion, emphasizing the importance of hygiene and monitoring for complications. Key steps in the care process and proper positioning of patients during procedures are also outlined.