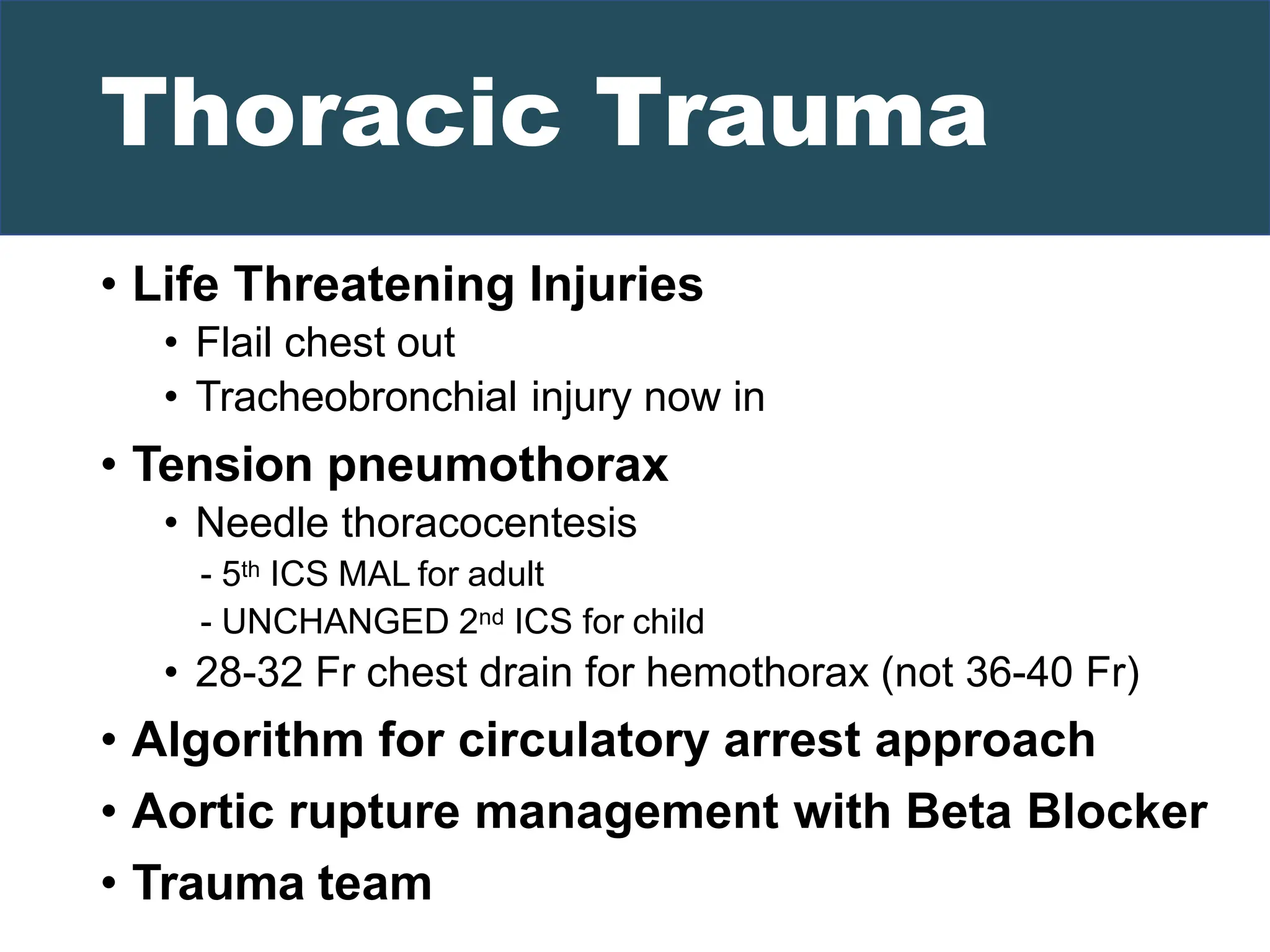
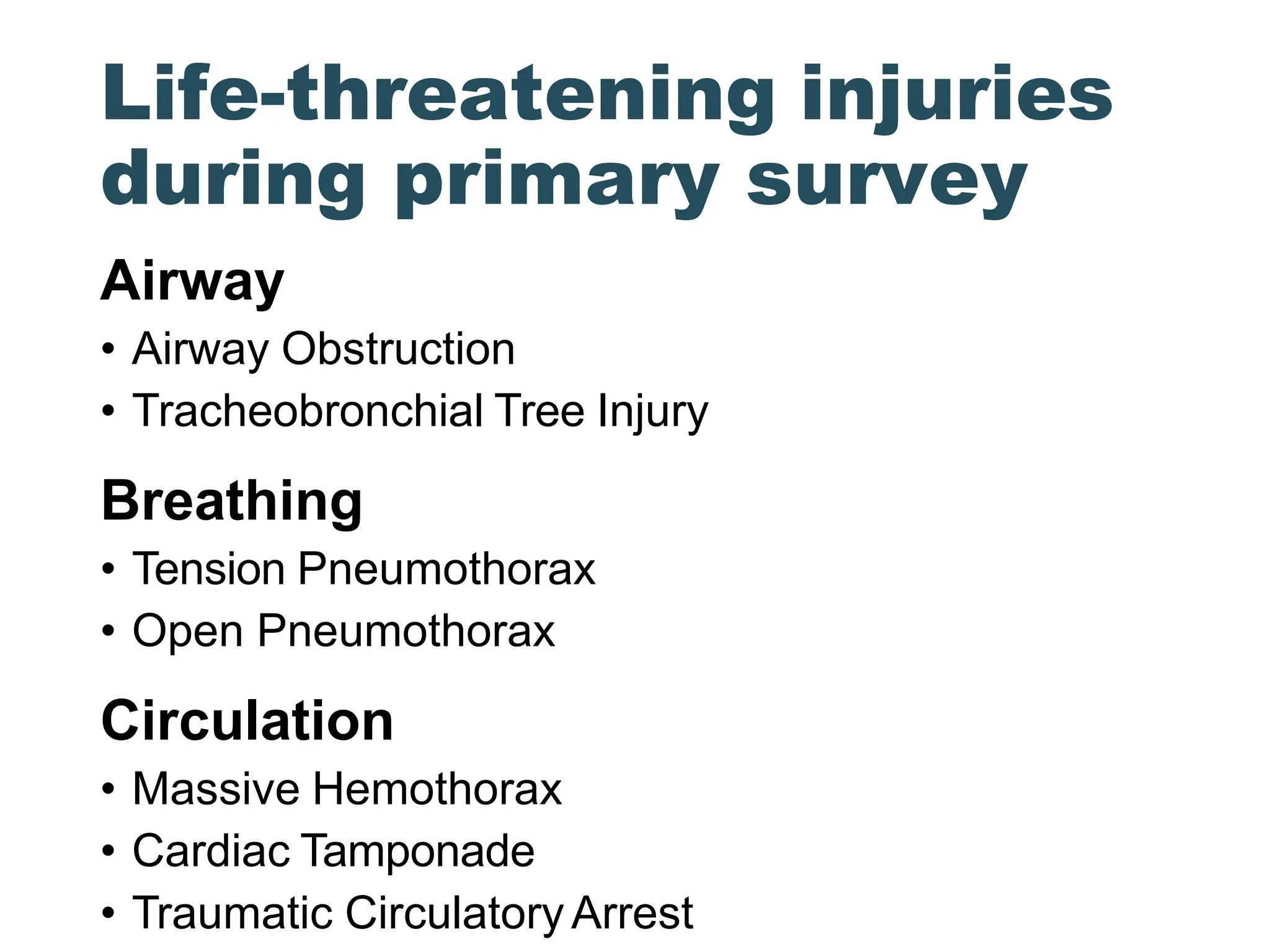
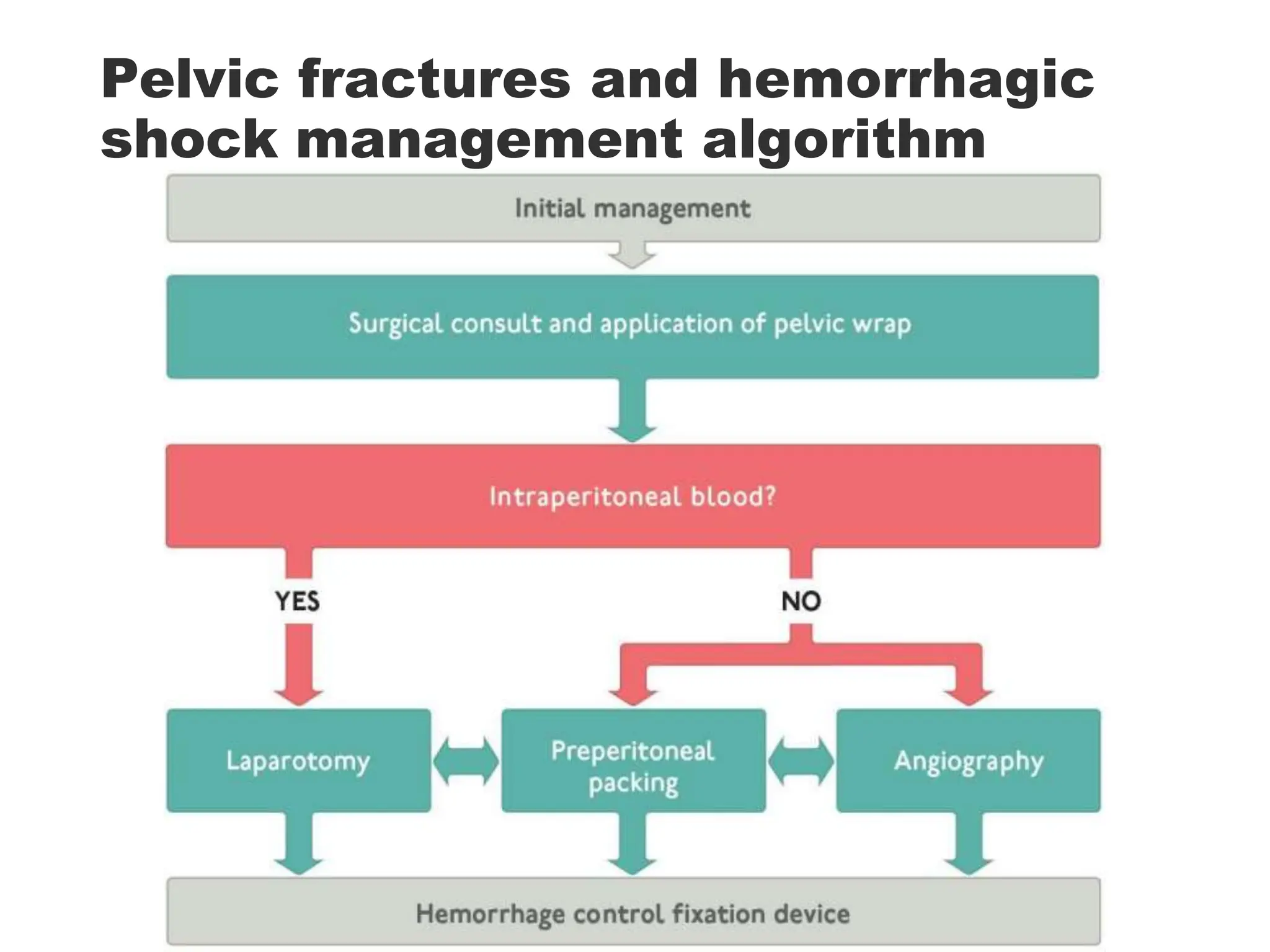
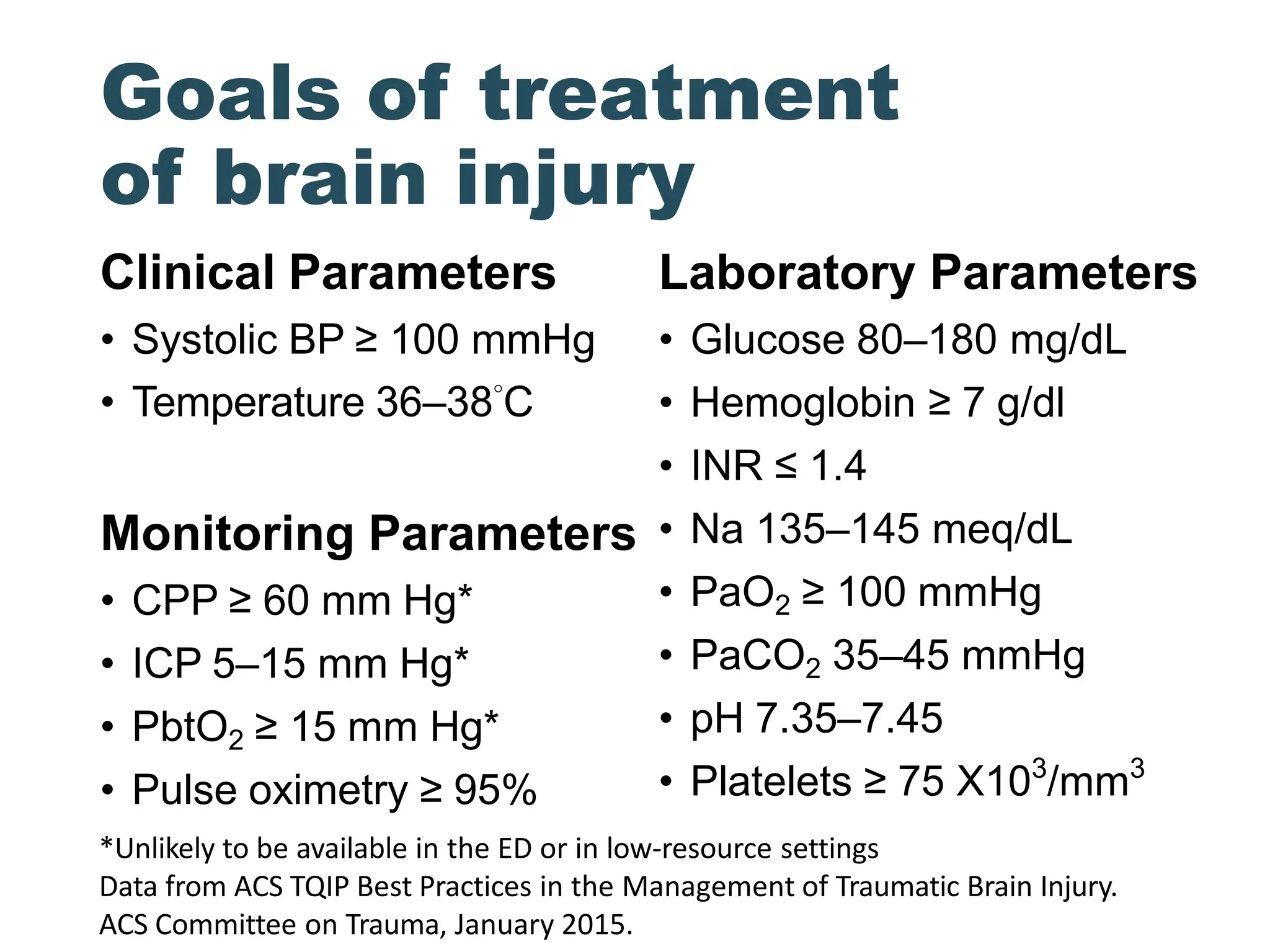
The document summarizes several key updates to the 10th edition of the ATLS guidelines. Some notable changes include restricting initial fluid resuscitation to 1 L, emphasizing drug-assisted intubation over rapid sequence intubation, recommending early use of blood products and tranexamic acid for shock management, and introducing algorithms for traumatic cardiac arrest and pelvic fracture hemorrhage. The guidelines also provide new recommendations for several areas like needle thoracocentesis location, head trauma anticoagulation reversal, and avoiding unnecessary CT scans during transfer to definitive care.