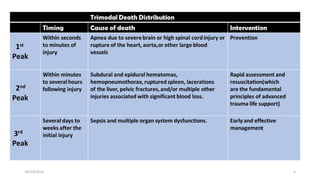
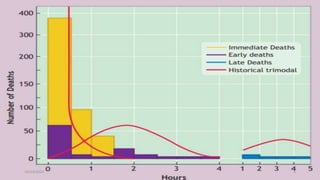
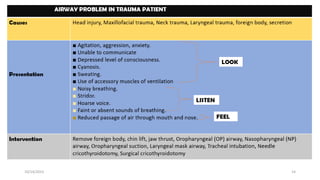
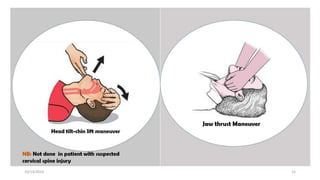
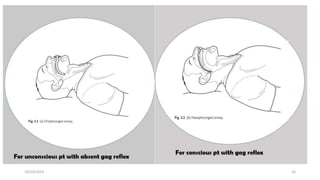
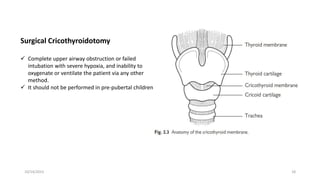
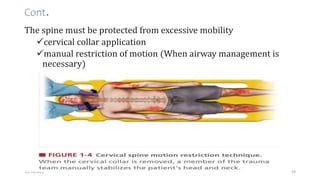
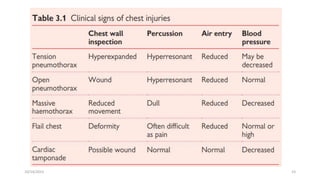
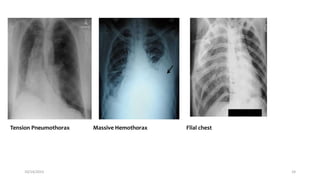
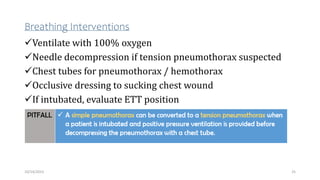
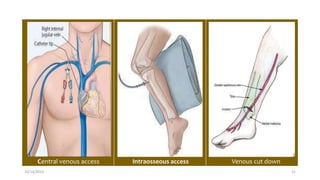
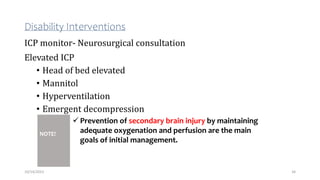
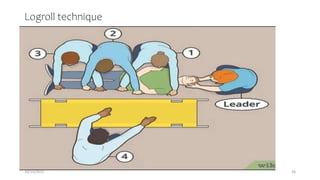
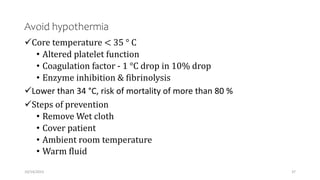
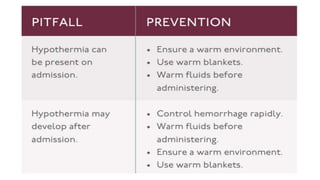
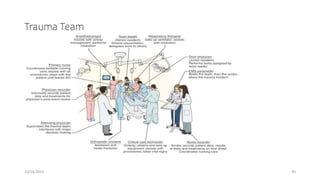
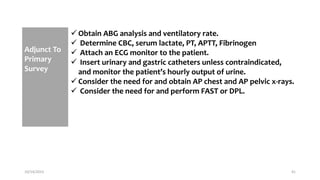
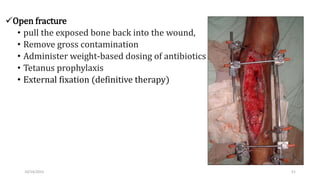
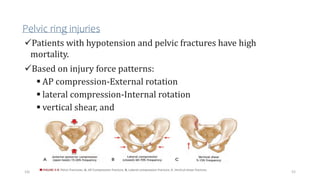
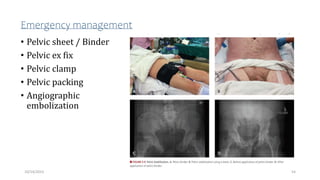
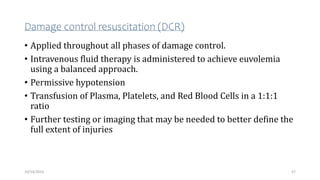
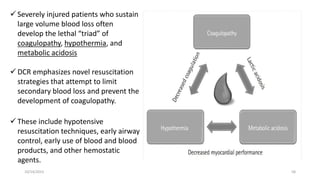
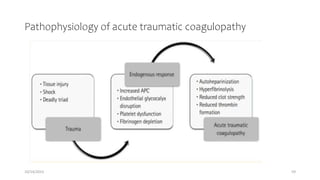
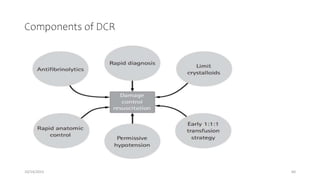
The document outlines the Advanced Trauma Life Support (ATLS) guidelines, emphasizing a structured approach to the initial assessment and management of trauma patients using the ABCDE methodology. It highlights the critical statistics on trauma-related deaths, discusses musculoskeletal injuries, pelvic trauma, and the importance of damage control resuscitation and surgery. Key interventions for airway management, breathing, circulation, and disability are detailed, alongside a focus on emergency protocols and resuscitation techniques.