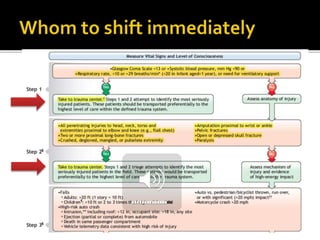
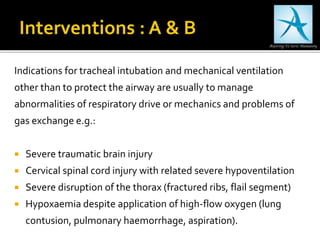
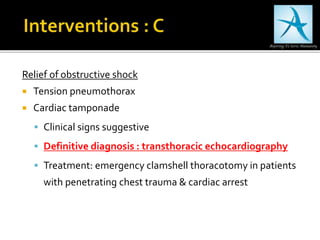
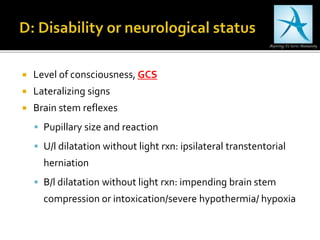
The document provides guidelines on the assessment and management of trauma patients in the pre-hospital setting. It emphasizes maintenance of airway, breathing, and circulation as top priorities, with rapid transport to a trauma center. Diagnostic techniques like focused assessment with sonography for trauma (FAST) exam and indications for intubation are outlined. Triage systems like revised trauma score (RTS) and injury severity score (ISS) are also summarized for evaluating patients and comparing outcomes.