Acid base maintenance.
Biochemistry
Acid base maintenance
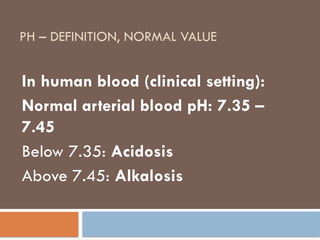
pH – definition, normal value
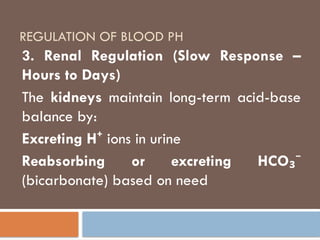
Regulation of blood PH
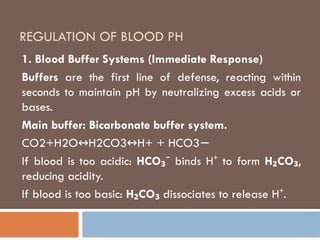
Blood buffer system
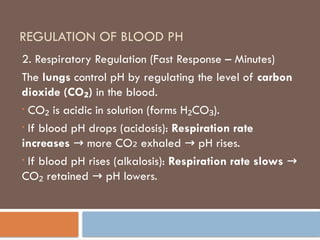
Respiratory regulation
Renal regulation
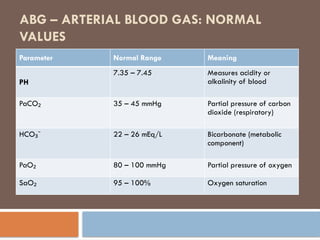
Arterial Blood Gas
ABG Normal Value
Acid base disorder
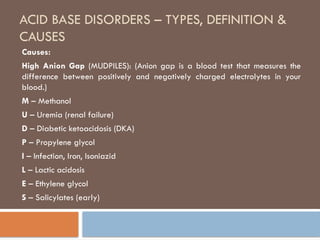
types of acid base
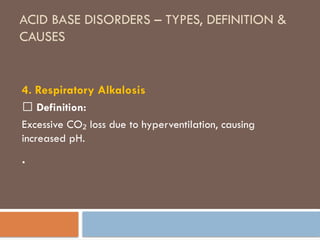
definition of acid base
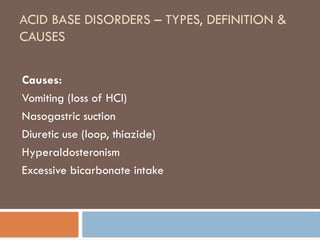
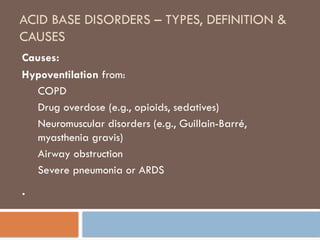
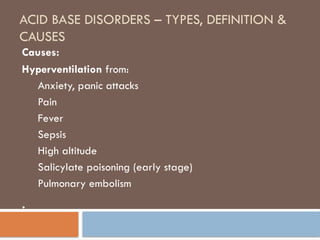
causes of acid base
Metabolic acidosis
Metabolic alkalosis
Respiratory acidosis
Respiratory alkalosis
Hyperventilation
Nursing
Nutrition