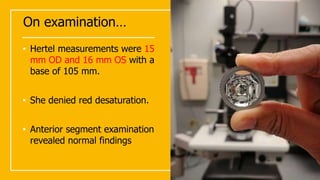
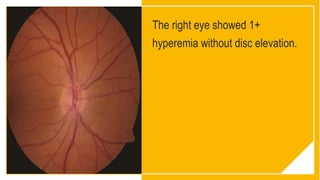
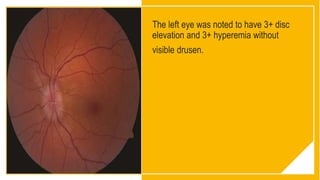
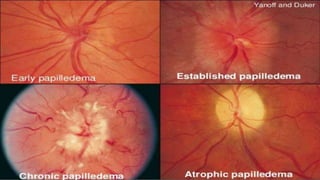
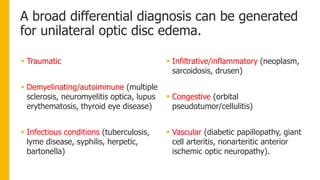
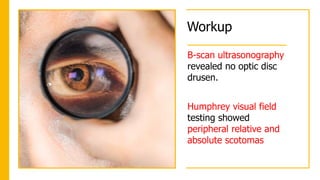
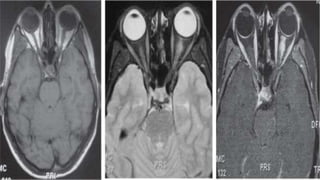
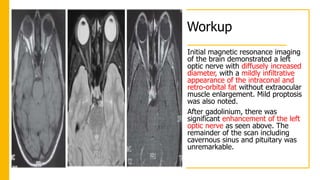
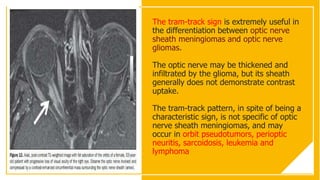
A 44-year-old woman presented for a LASIK consultation but was found to have unilateral optic disc edema in her left eye. Further workup with MRI revealed enhancement of the left optic nerve consistent with an optic nerve sheath meningioma. These types of tumors typically involve the orbital portion of the optic nerve and enhance with contrast in a characteristic "tram track" pattern on imaging. As the patient's examination and vision were stable, she was recommended for observation with serial exams and imaging to monitor for signs of progression.