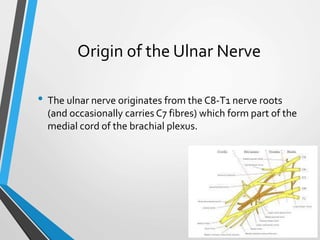
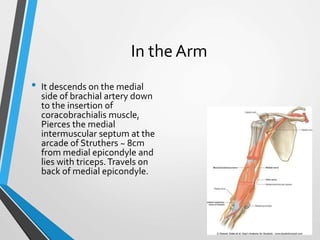
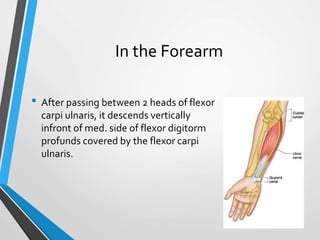
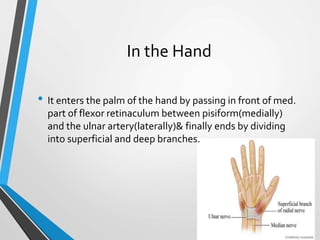
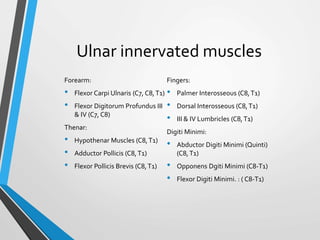
The ulnar nerve, a terminal branch of the brachial plexus, originates from the C8-T1 nerve roots and has a complex pathway through the axilla, arm, and forearm, entering the hand to innervate various muscles. Injuries to the ulnar nerve can lead to significant motor and sensory impairments, including characteristic 'claw hand' deformities and loss of sensation in the medial aspect of the hand. Common entrapment syndromes include cubital tunnel syndrome and Guyon's canal syndrome, which can occur due to anatomical abnormalities or trauma.