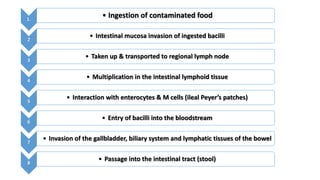
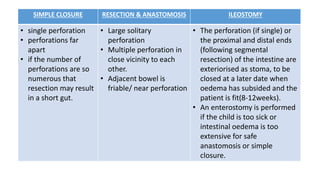
Typhoid ileal perforation is a frequent and severe surgical complication of typhoid fever, primarily affecting children in developing countries. Diagnosis is mostly clinical, and the main treatment is surgery, which includes options like perforation closure or segmental resection. Early diagnosis and effective management are crucial to minimize complications and mortality.