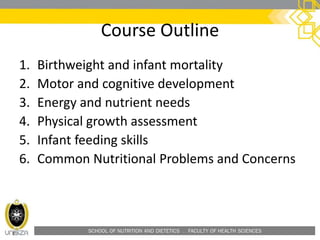
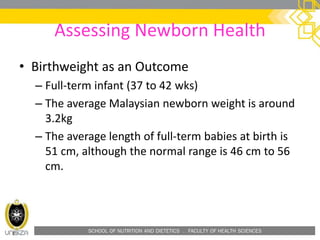
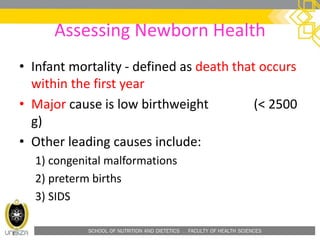
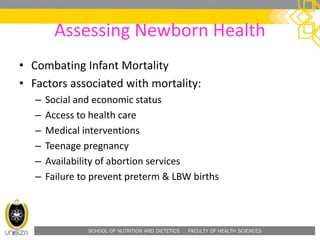
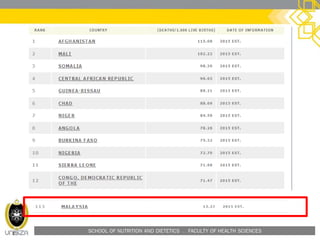
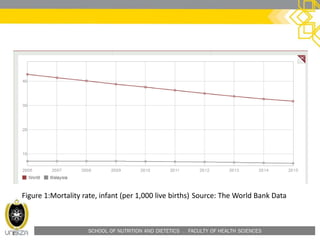
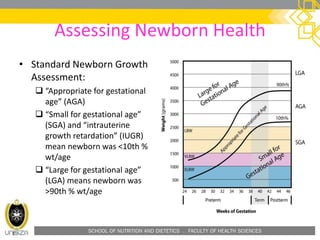
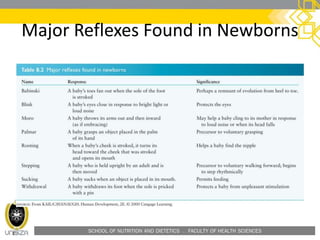
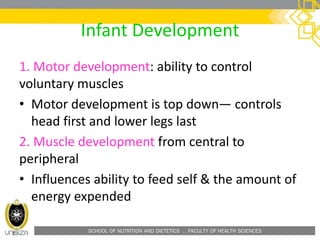
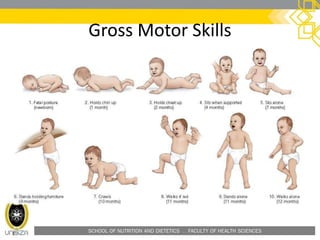
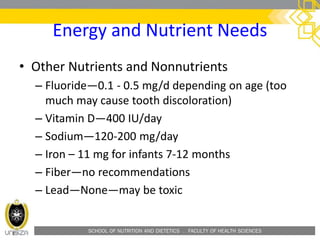
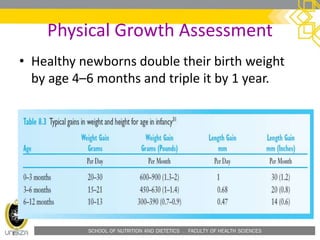
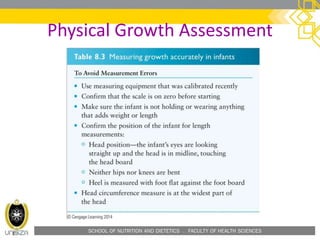
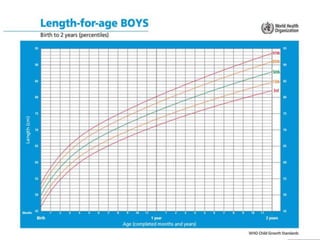
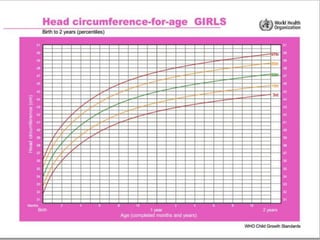
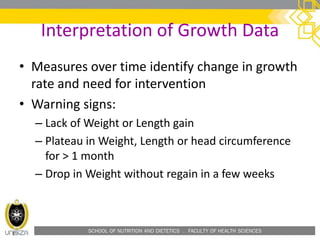
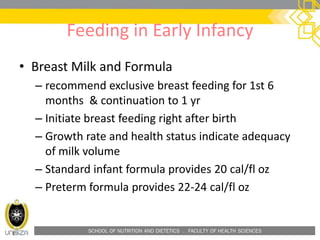
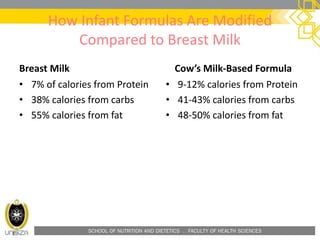
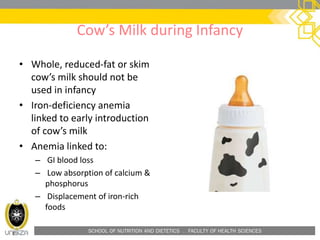
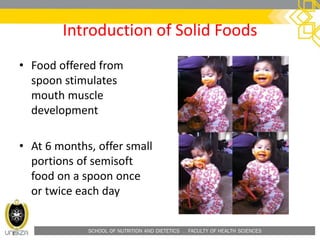
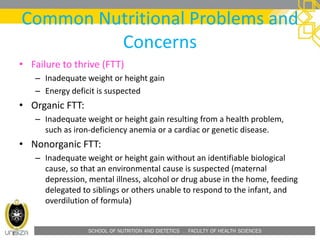
This document outlines a lecture on infant nutrition. It discusses assessing newborn health, including birthweight and factors related to infant mortality. It covers infant development, including motor, cognitive, and digestive system development. It also addresses energy and nutrient needs of infants, including calories, protein, fat and other nutrients. The document discusses physical growth assessment of infants and common feeding practices in early infancy, including breastfeeding and formula. It concludes by covering the development of infant feeding skills.