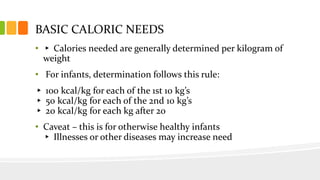
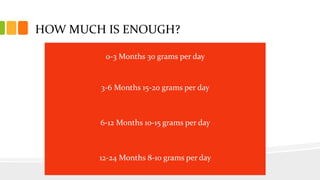
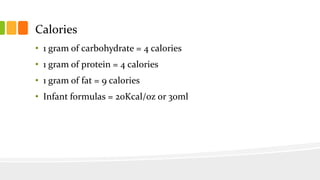
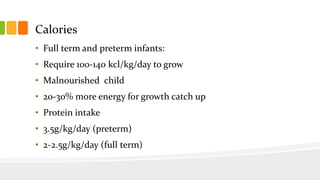
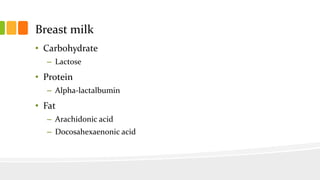
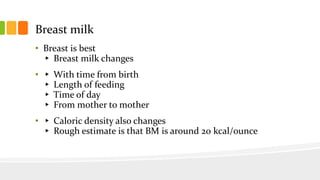
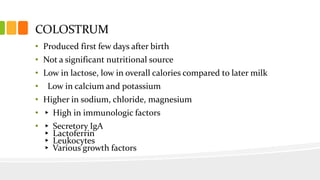
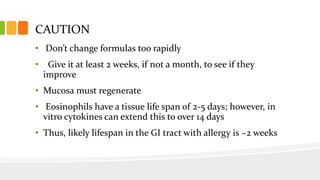
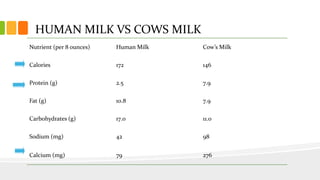
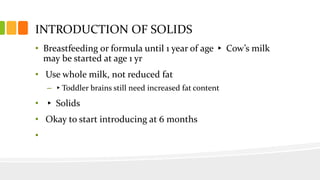
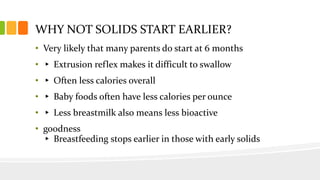
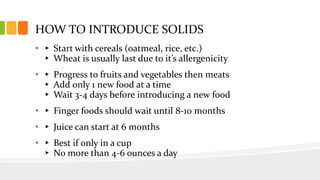
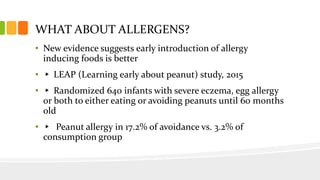
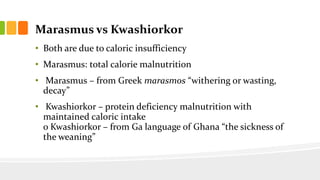
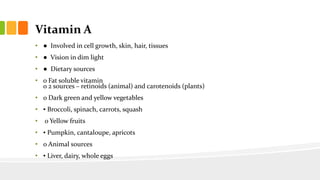
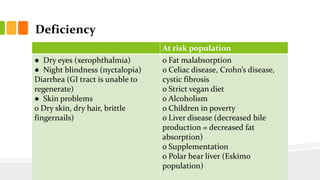
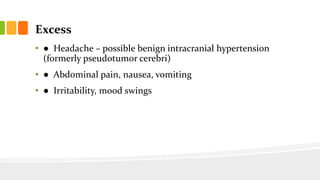
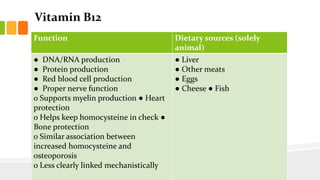
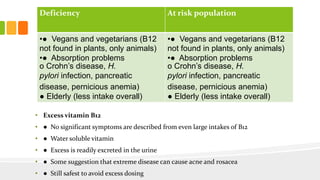
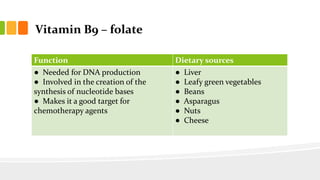
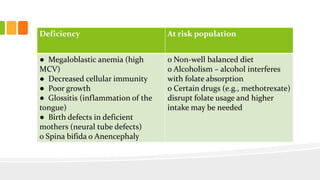
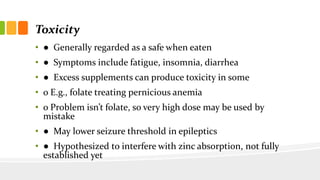
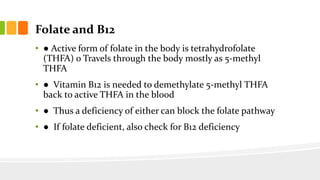
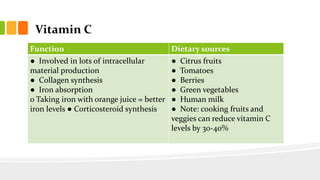
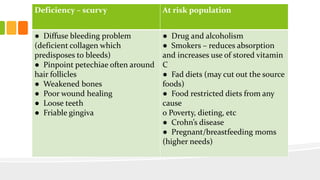
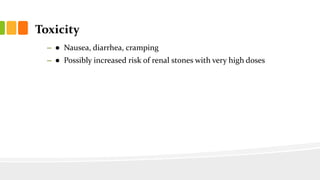
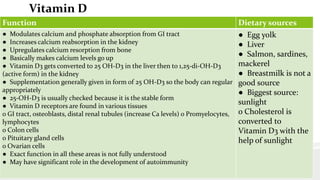
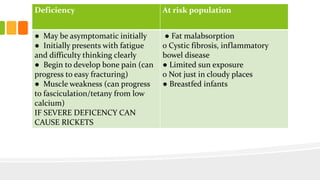
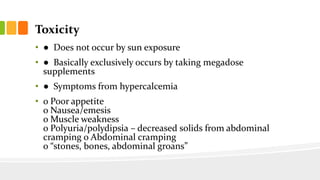
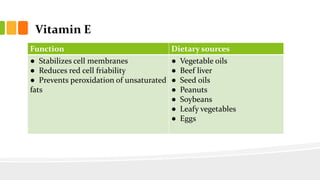
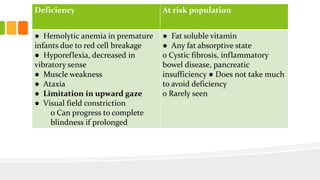
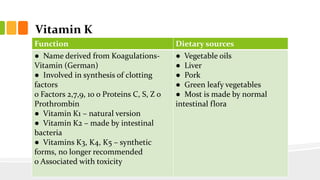
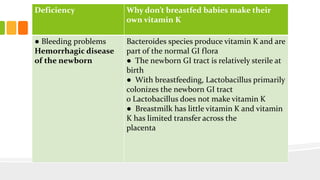
This document discusses nutrition for infants and children. It covers basic caloric needs determined by weight, the introduction of solids beginning around 6 months, and vitamins and minerals important for growth and development. Breastmilk is outlined as the best source of nutrition for infants, providing antibodies, fats and proper nutrients for development. The risks and symptoms of deficiencies for various vitamins like A, B12, folate, C, and D are also summarized.