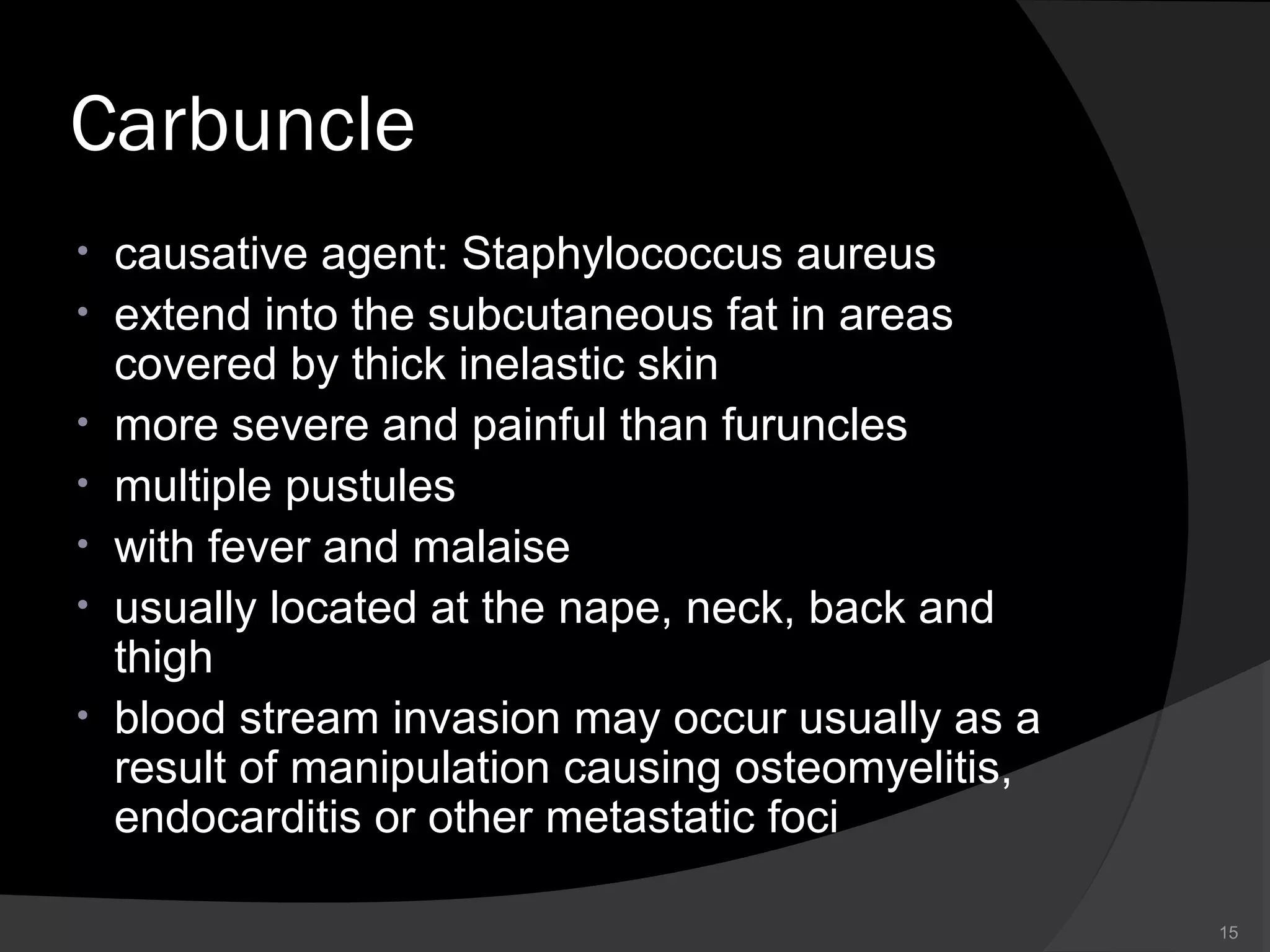
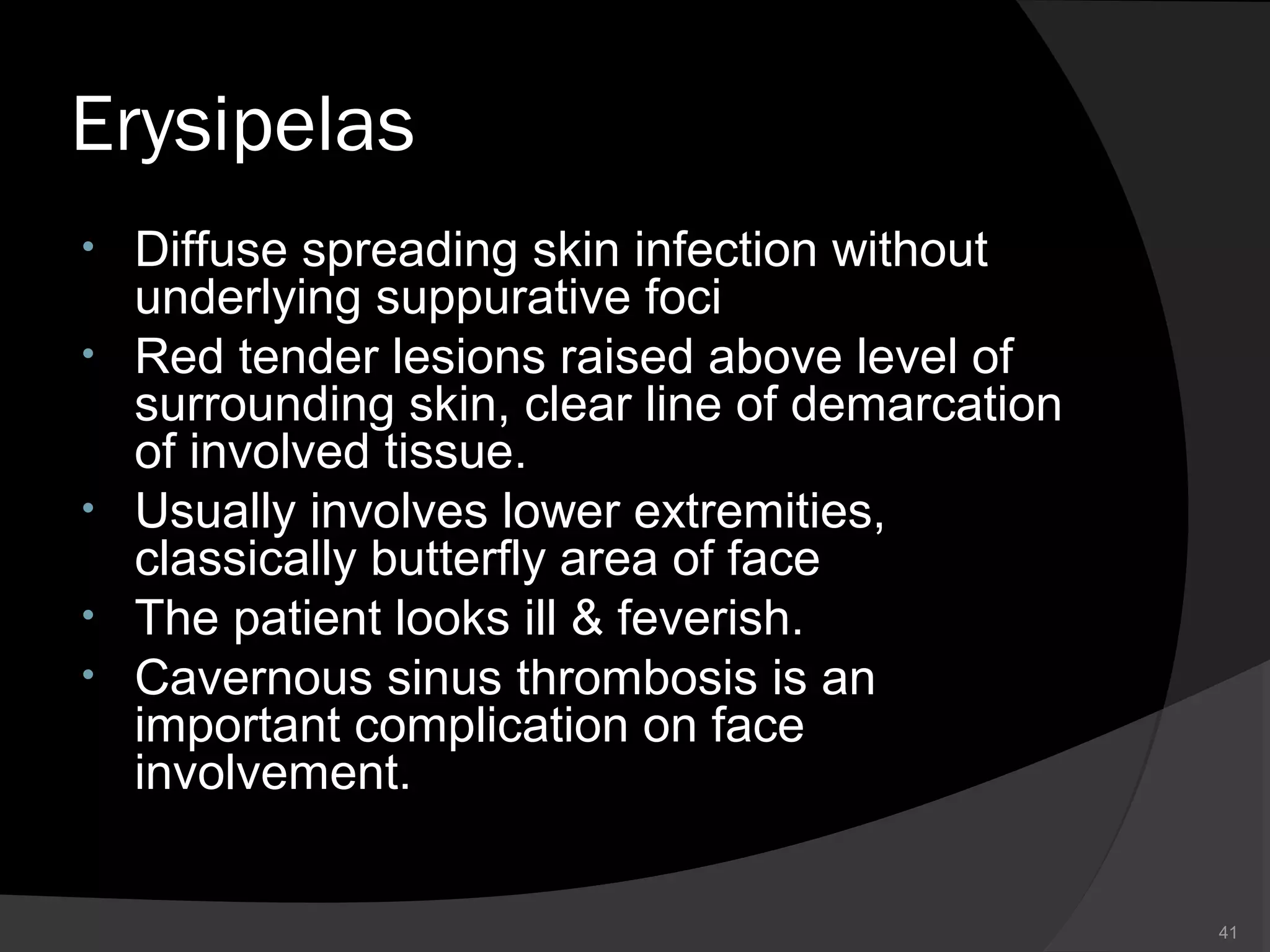
The document provides an overview of bacterial skin infections, detailing various common types such as folliculitis, boils, carbuncles, and impetigo, and their causative agents, primarily Staphylococcus and Streptococcus species. It describes symptoms, risk factors, and treatment options for each condition, emphasizing the importance of hygiene and antibiotic therapy. Additionally, it covers severe conditions like necrotizing fasciitis and scarlet fever, including their diagnosis, management, and epidemiology.