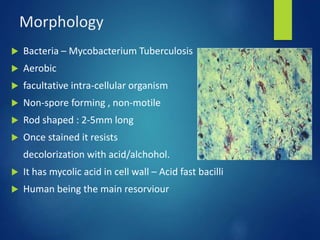
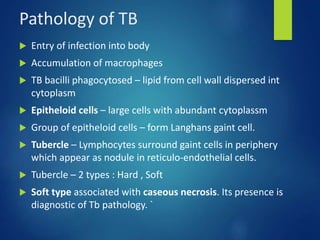
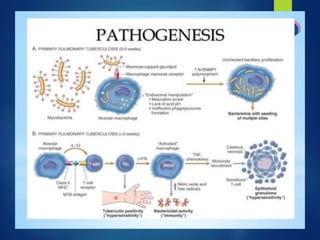
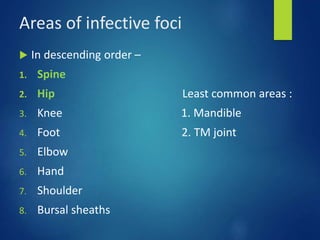
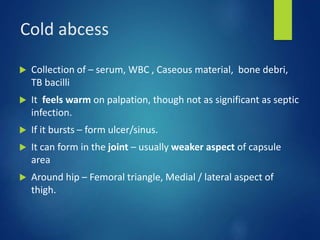
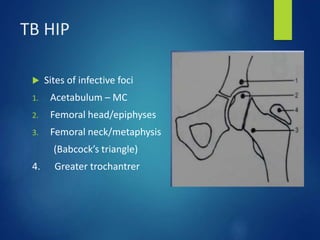
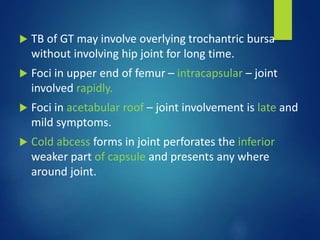
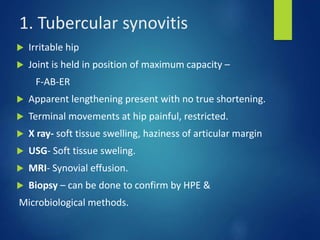
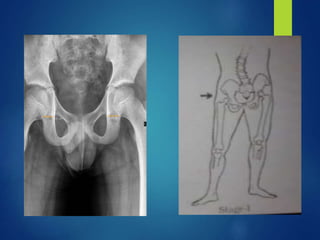
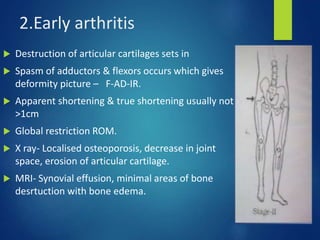
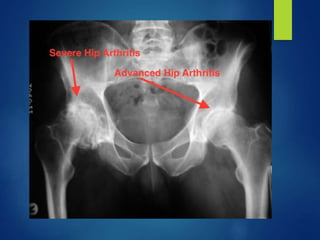
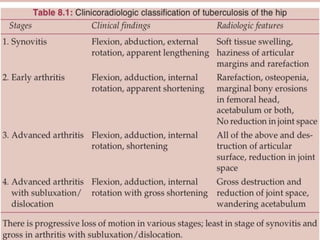
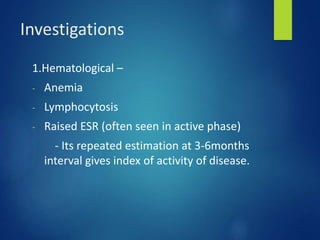
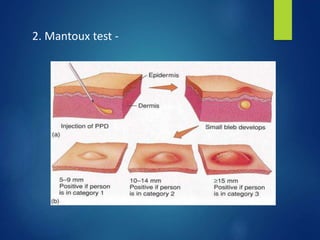
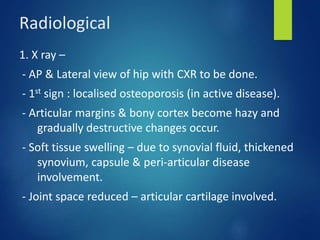
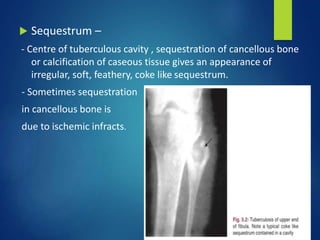
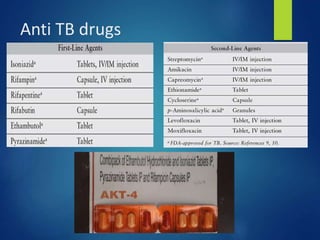
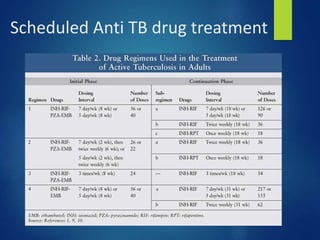
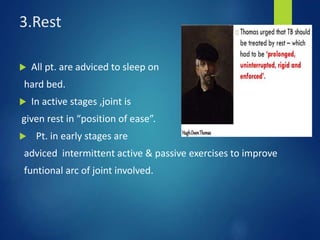
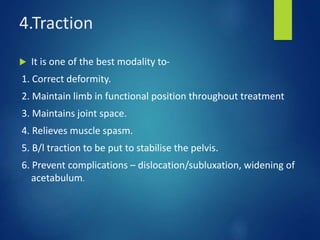
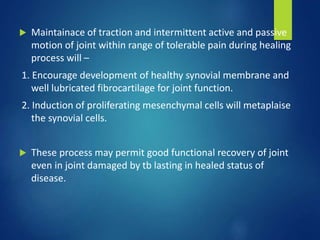
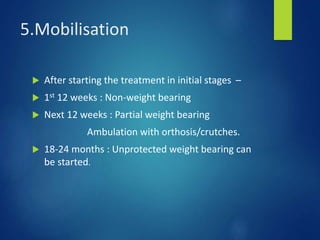
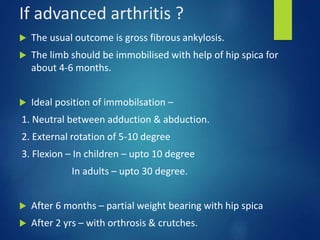
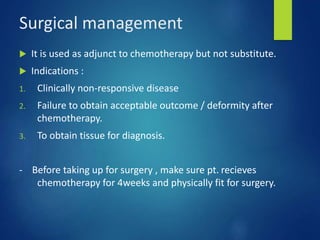
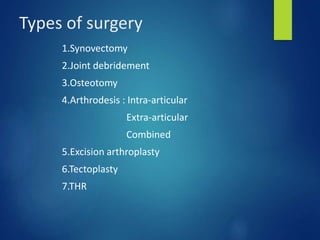
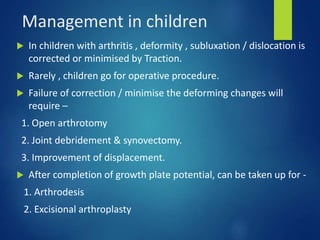
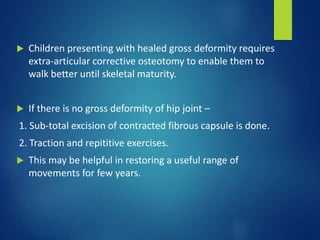
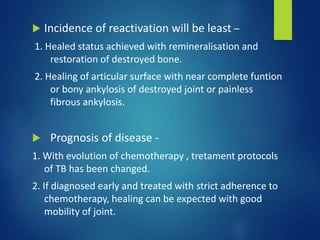
This document discusses tuberculosis of the hip. It begins by describing the morphology of the Mycobacterium tuberculosis bacteria. It then covers the pathology and stages of TB infection, including formation of tubercles and caseous necrosis. Risk groups for TB are listed. Common sites of TB infection are provided, with the hip being one of the most common. Features specific to TB of the hip include pain, limping and deformity. Stages of TB hip are outlined from initial synovitis to terminal arthritis. Diagnostic tests and treatments, including medical management with anti-TB drugs and surgical options, are summarized.