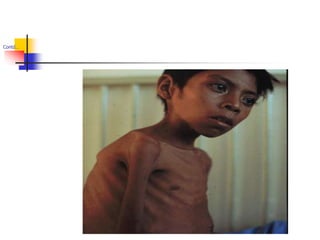
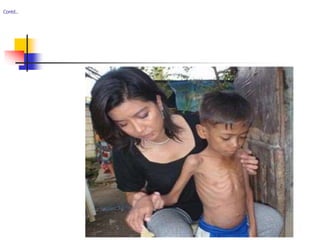
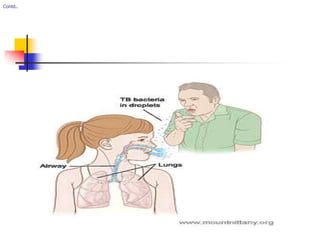
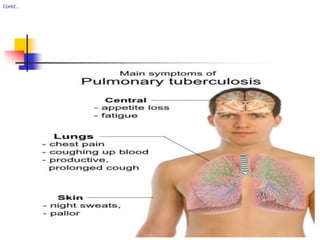
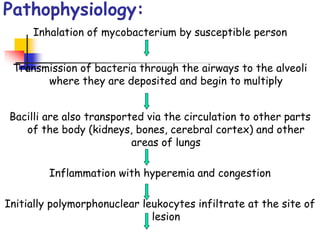
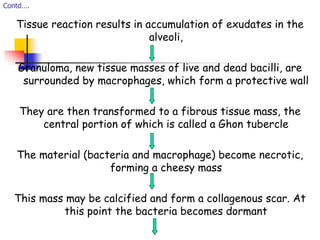
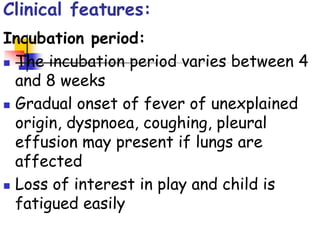
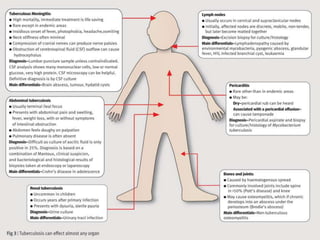
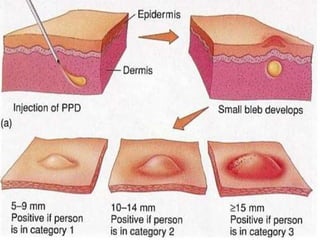
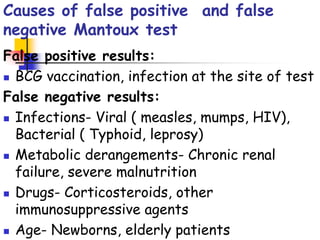
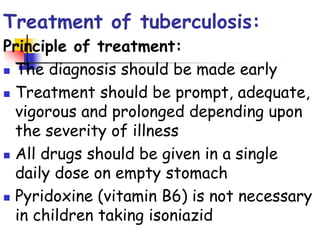
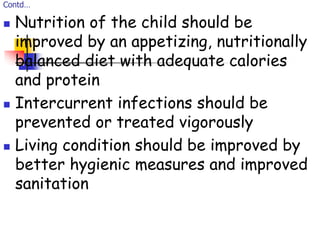
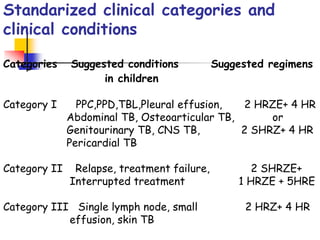
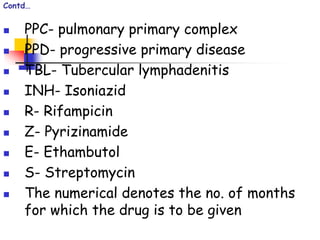
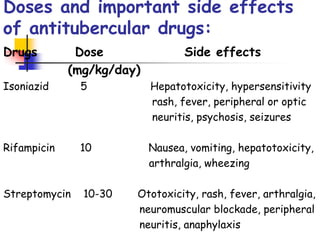
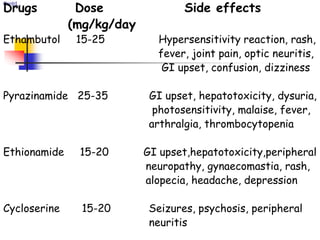
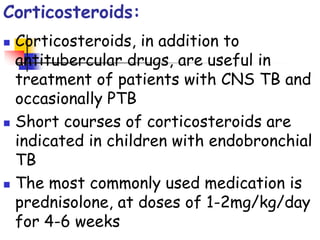
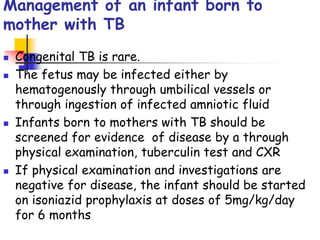
Tuberculosis is a chronic infectious disease caused by Mycobacterium tuberculosis that primarily affects the lungs. It spreads through inhaling droplets from infected individuals and can affect other organs. Young, malnourished, and immunocompromised children are most at risk. Diagnosis involves clinical features, tuberculin skin testing, chest x-rays, and microscopic examination of samples. Treatment consists of a multi-drug regimen over several months. Close contacts of active TB cases, such as young children, should receive preventive treatment to avoid infection.