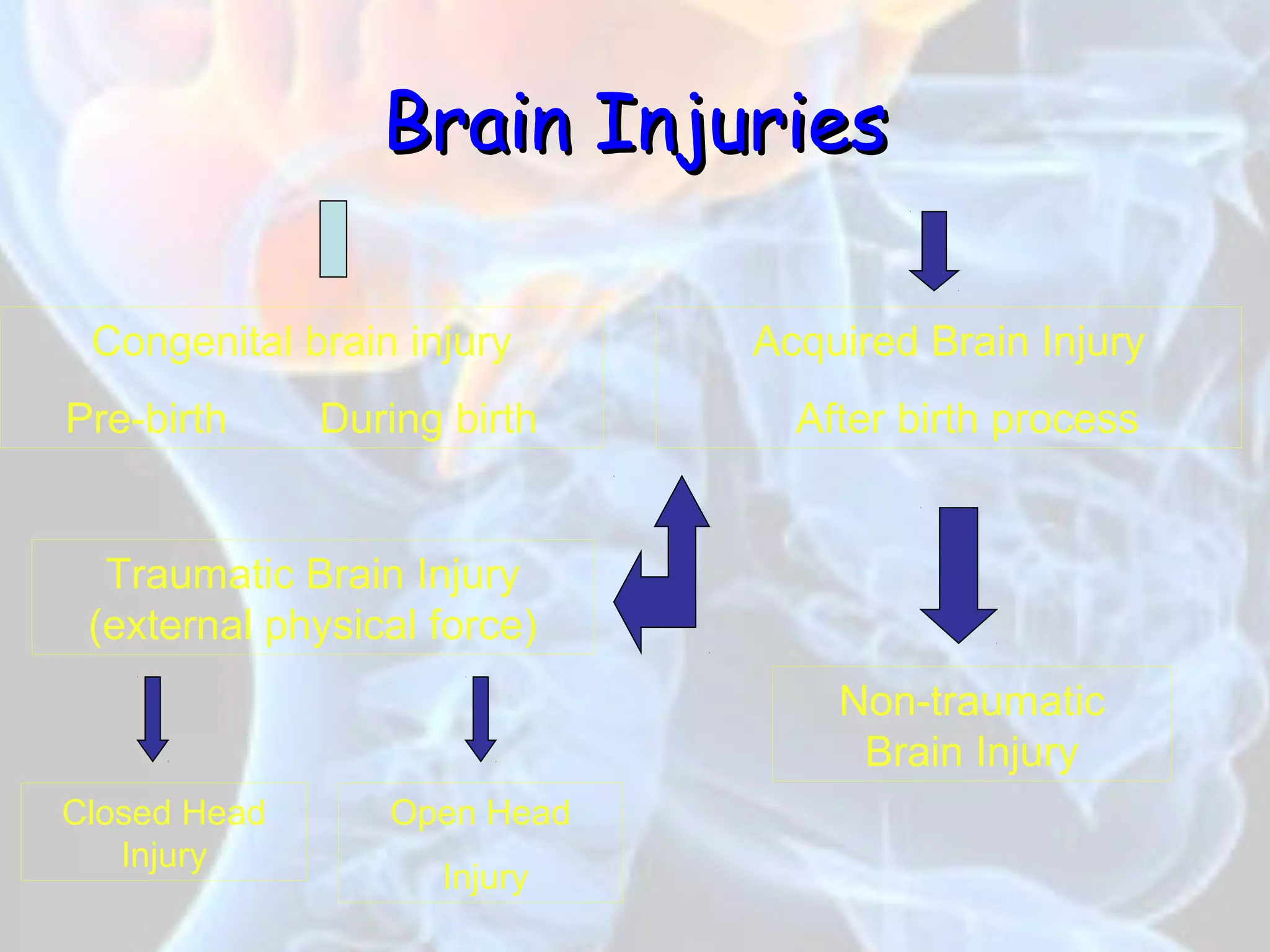
This document summarizes traumatic brain injury (TBI), including its causes, types, symptoms, treatment and outcomes. It discusses the epidemiology of TBI, noting it is a leading cause of death and disability worldwide. It describes the two main types of TBI - open and closed head injuries. It also summarizes the potential psychiatric issues after TBI like depression, mania, psychosis, OCD, PTSD and personality changes. Finally, it discusses factors that can influence outcomes, noting that 30-35% of severe brain injury cases result in death.