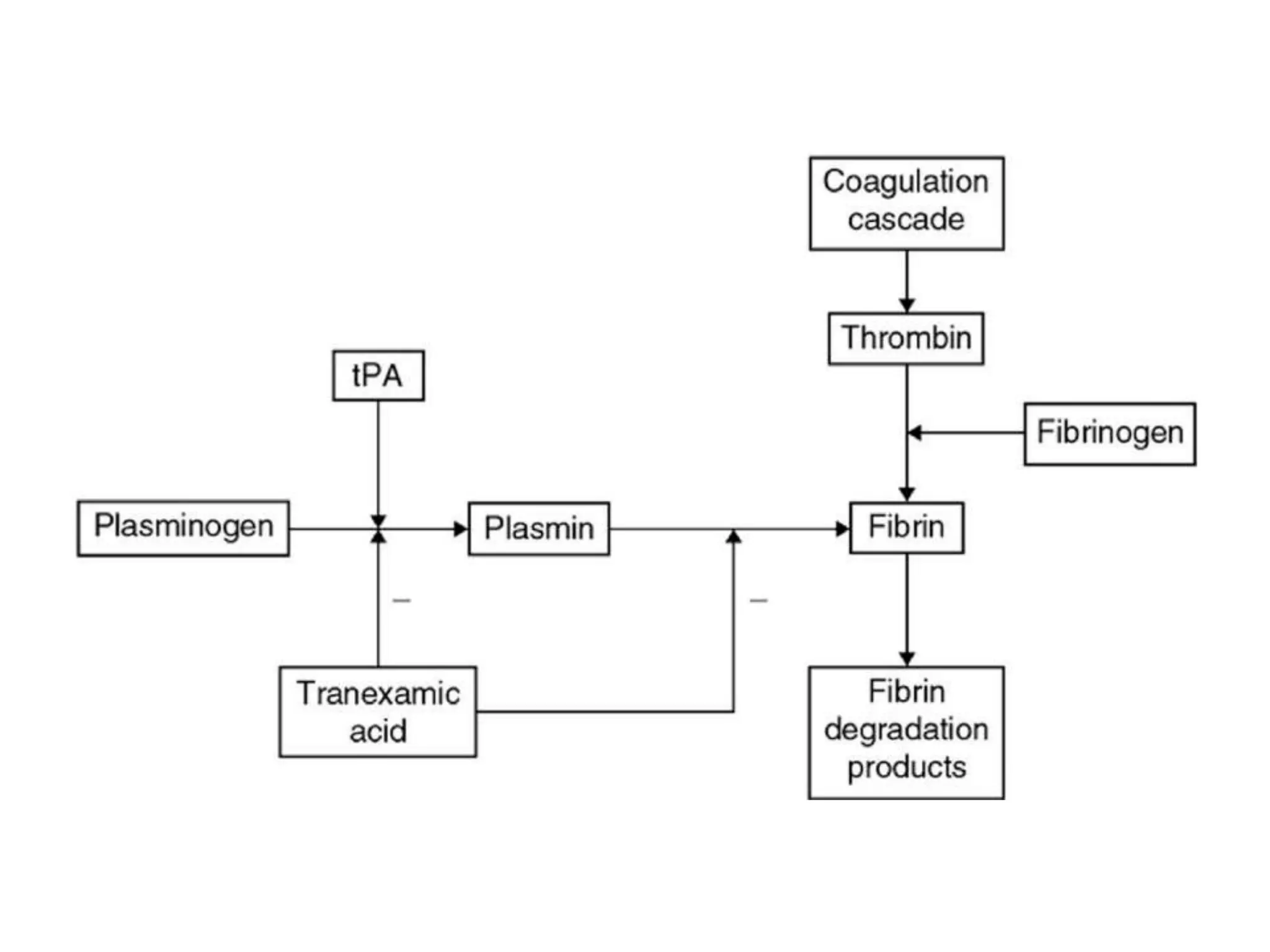
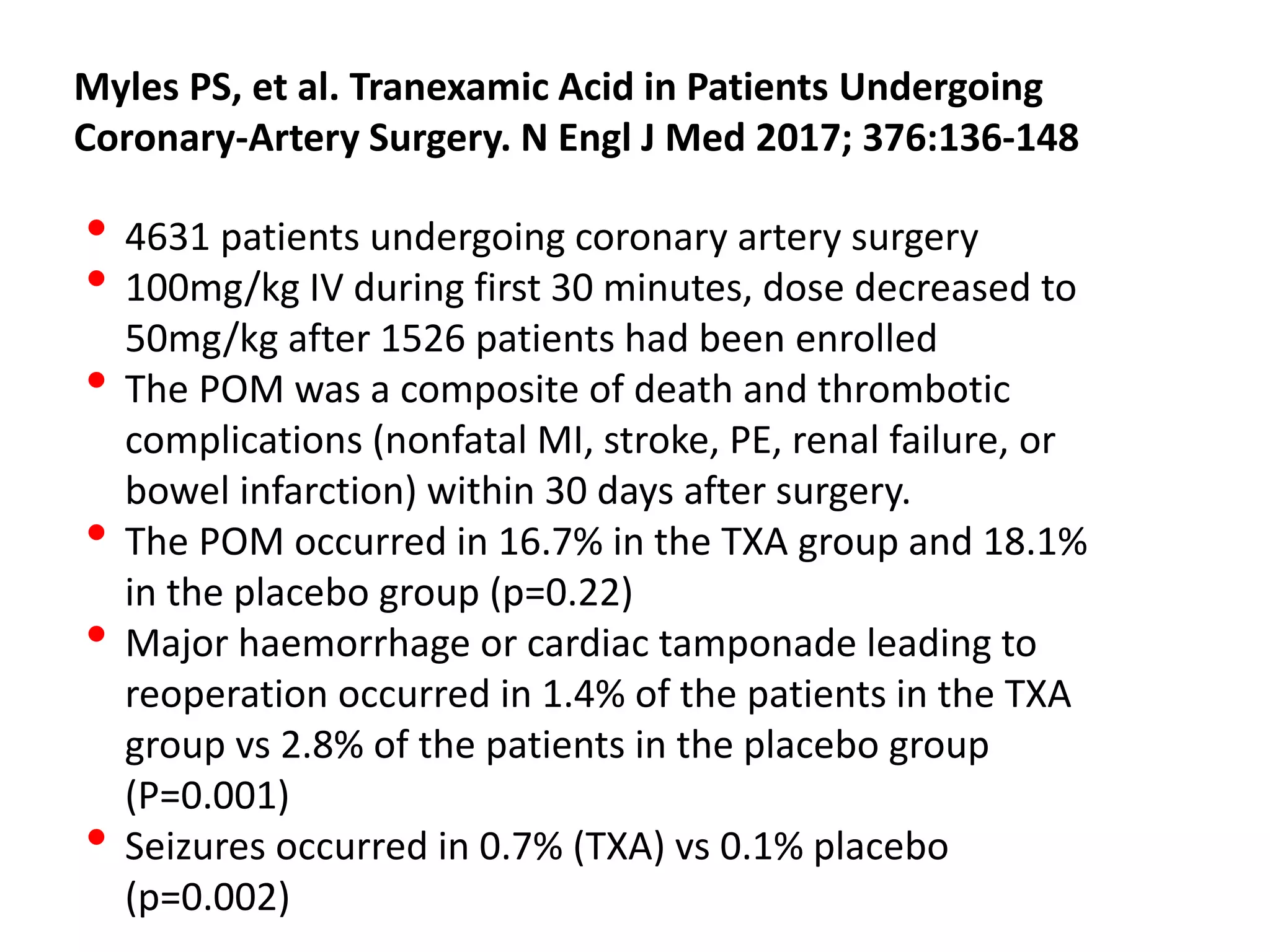
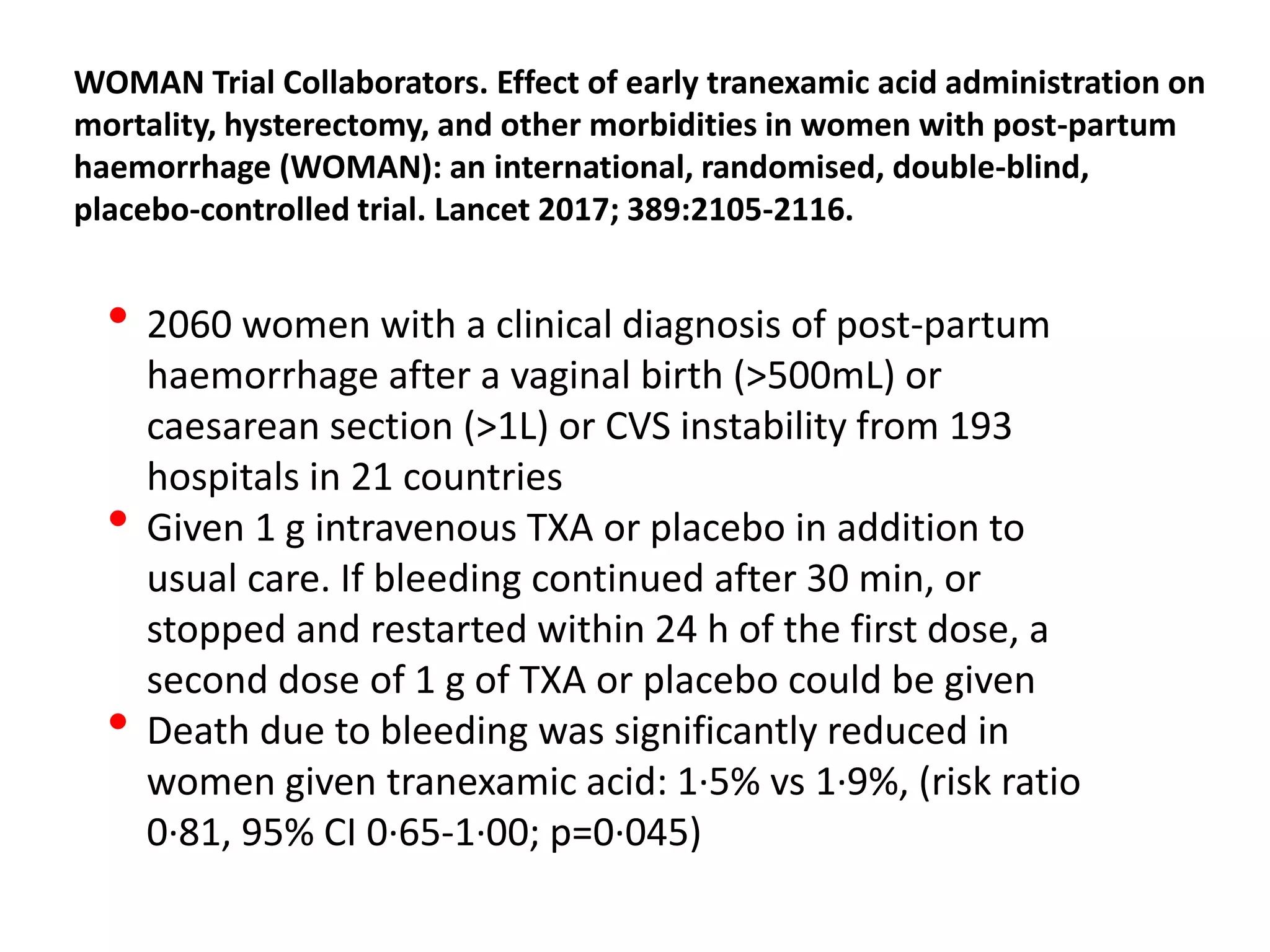
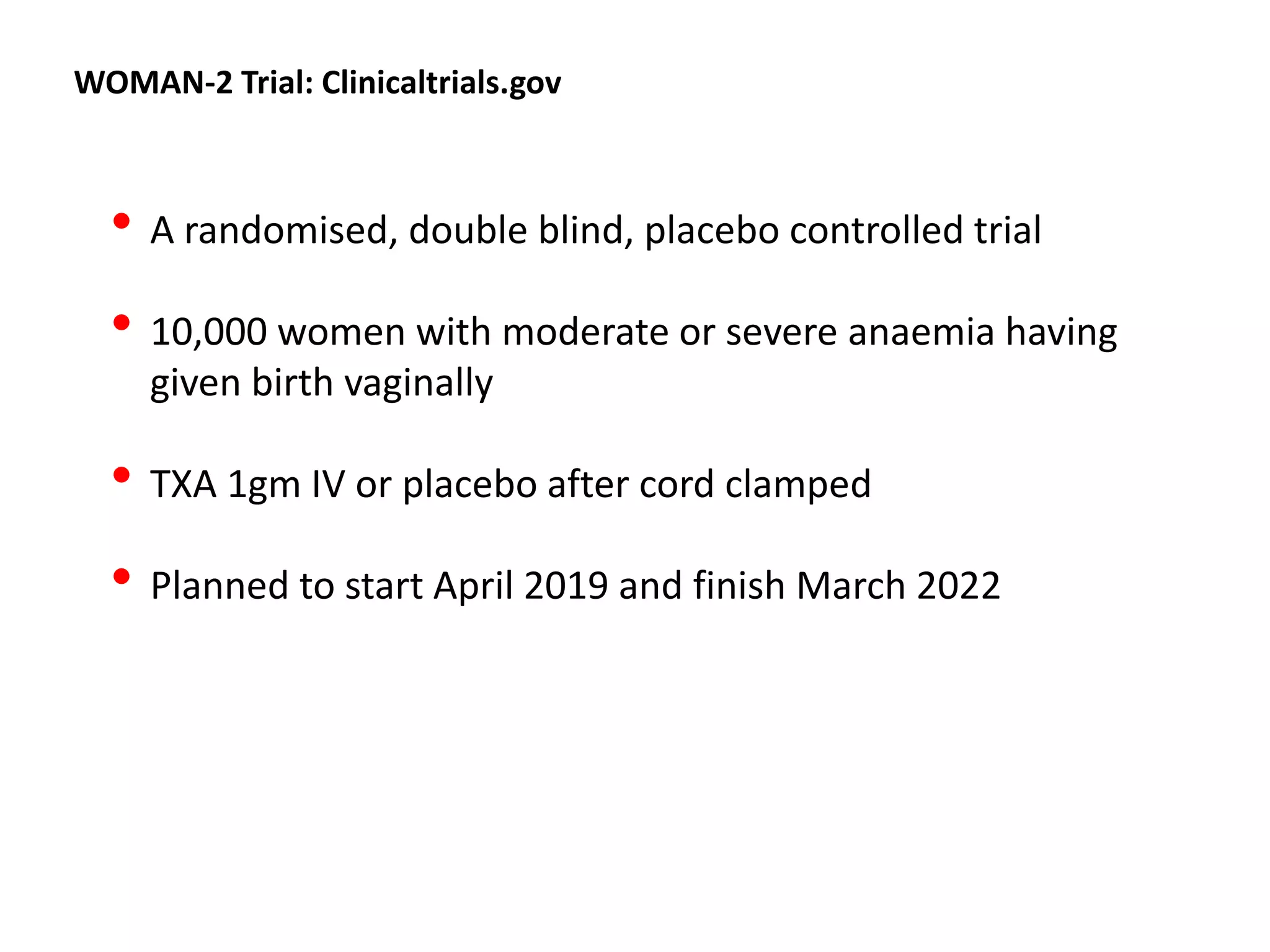
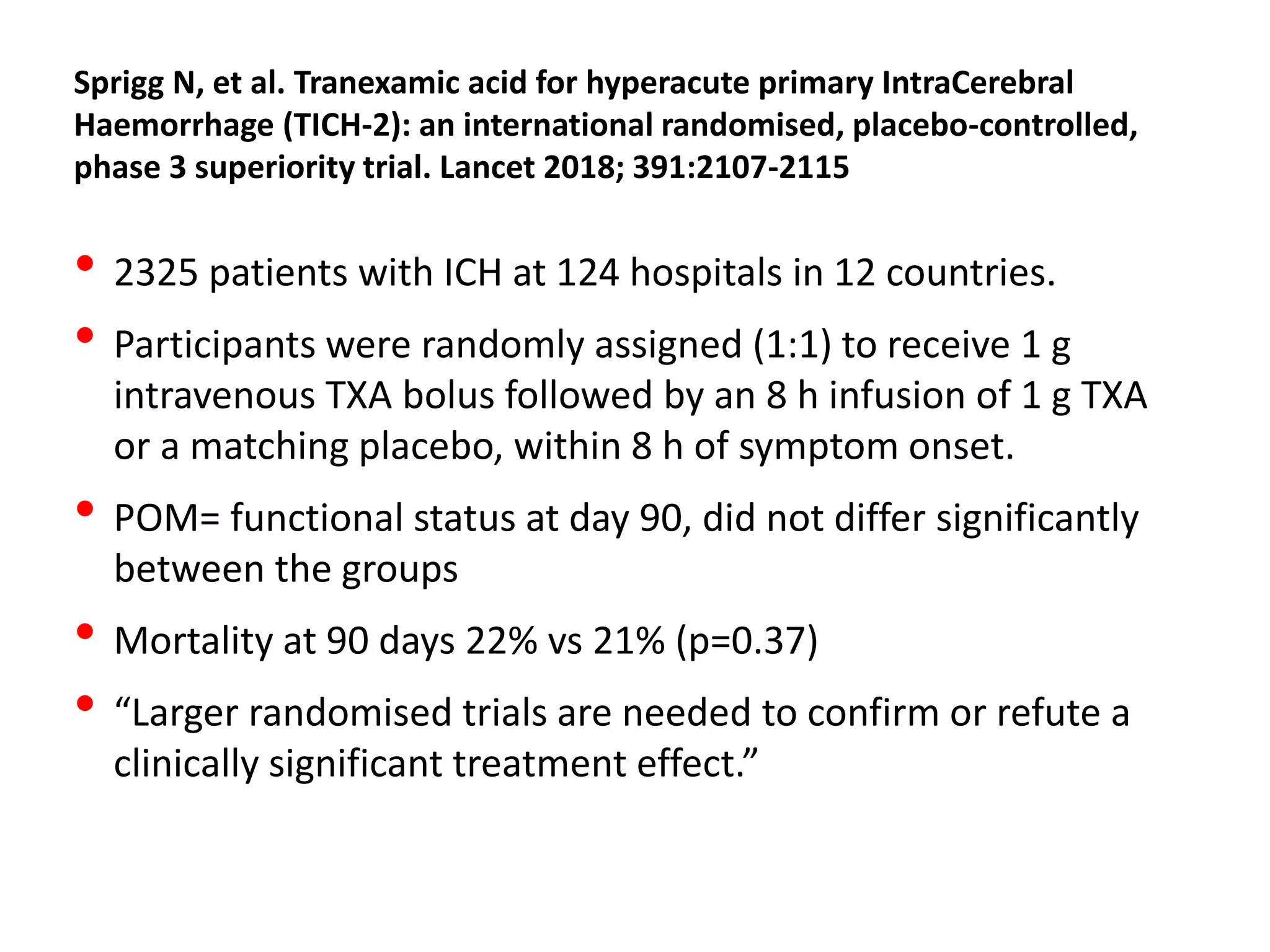
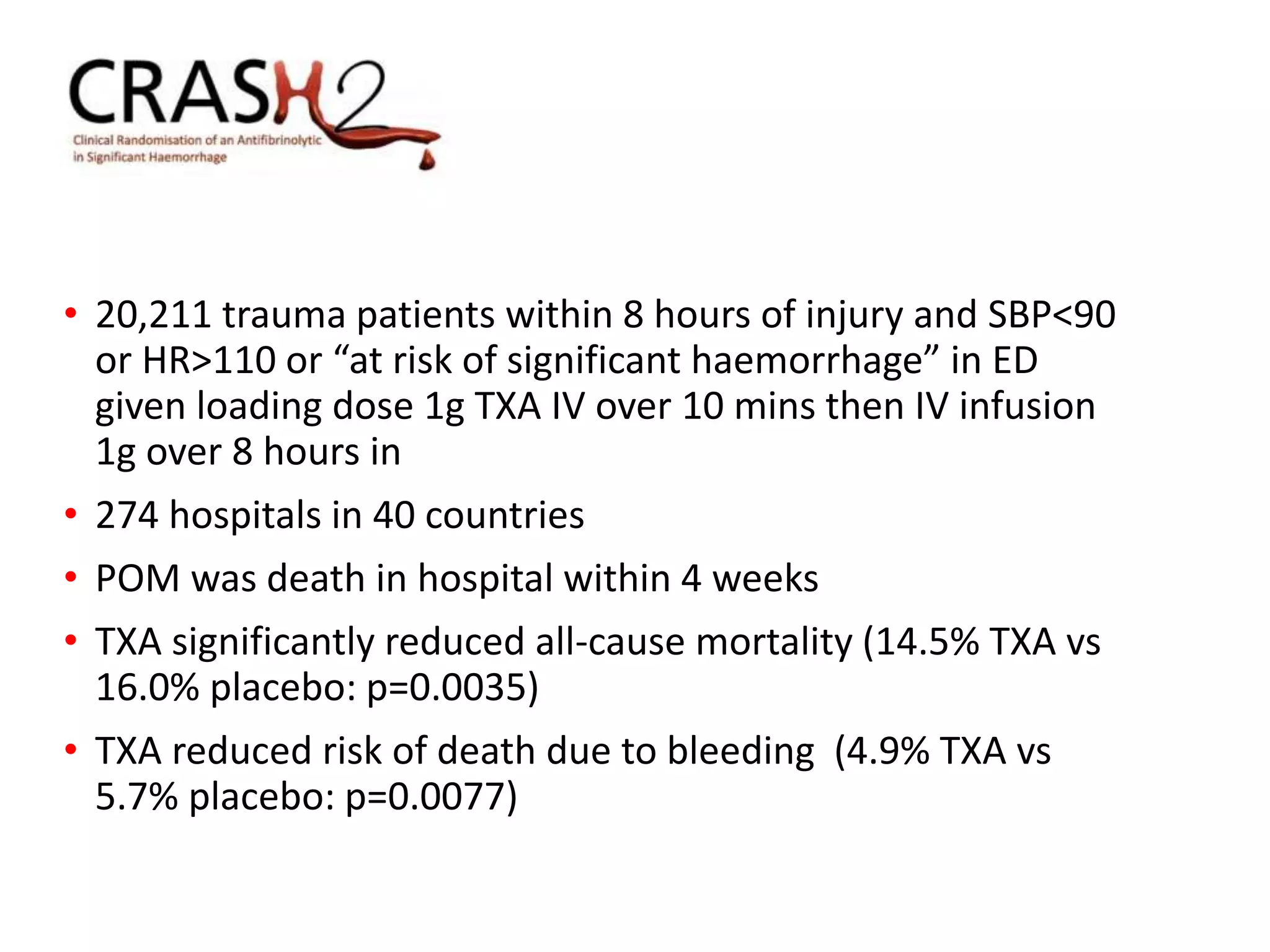
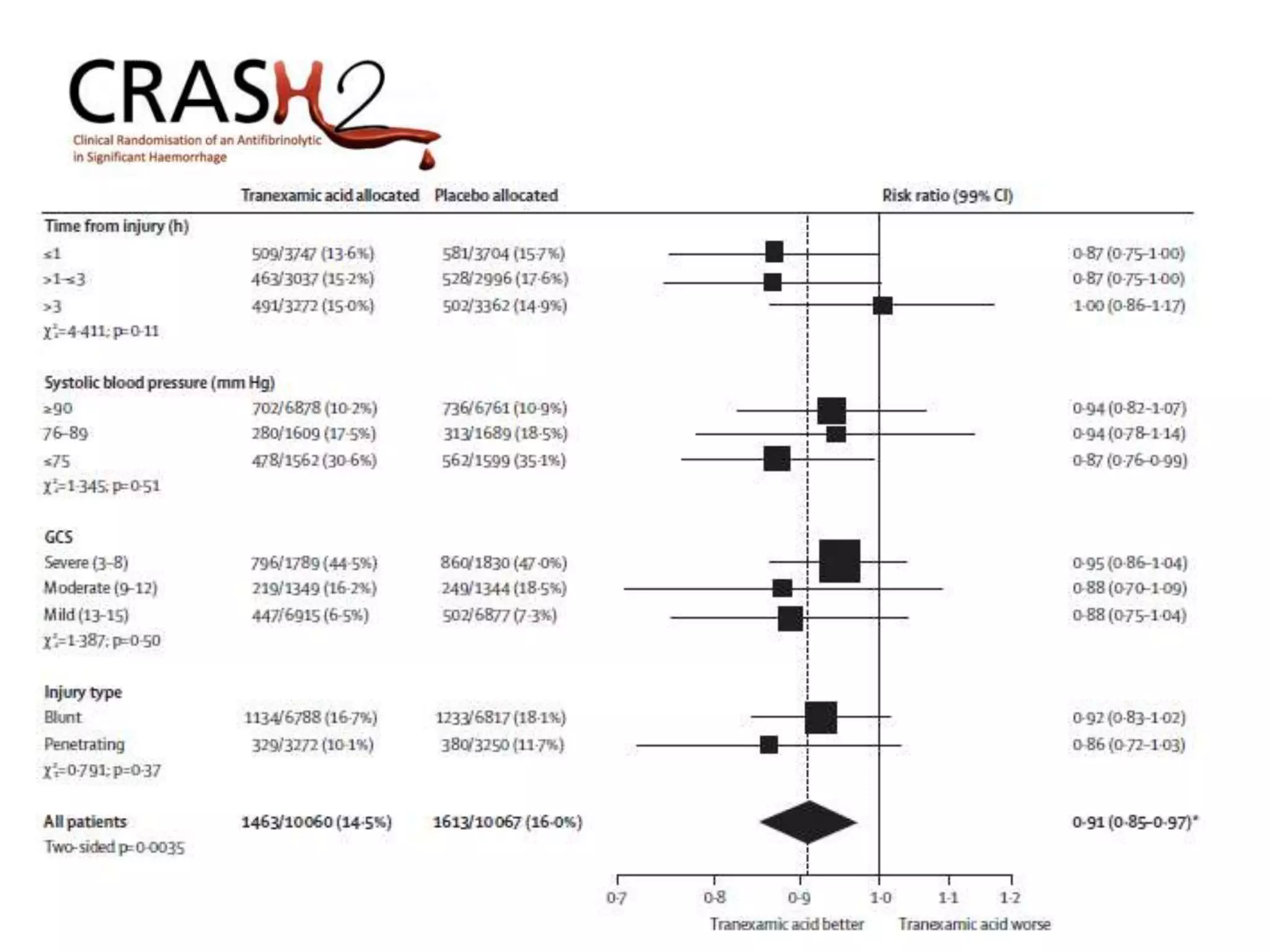
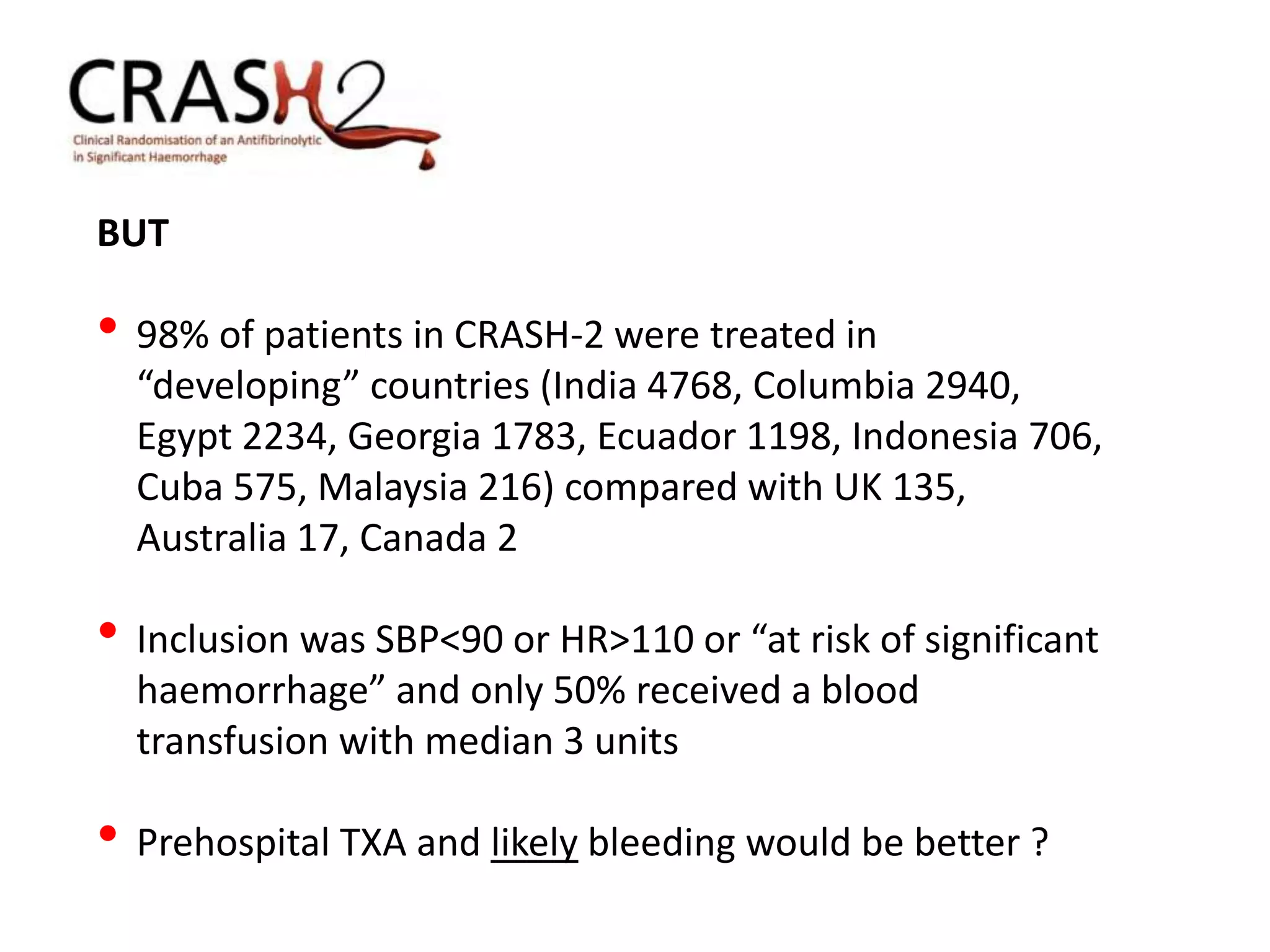
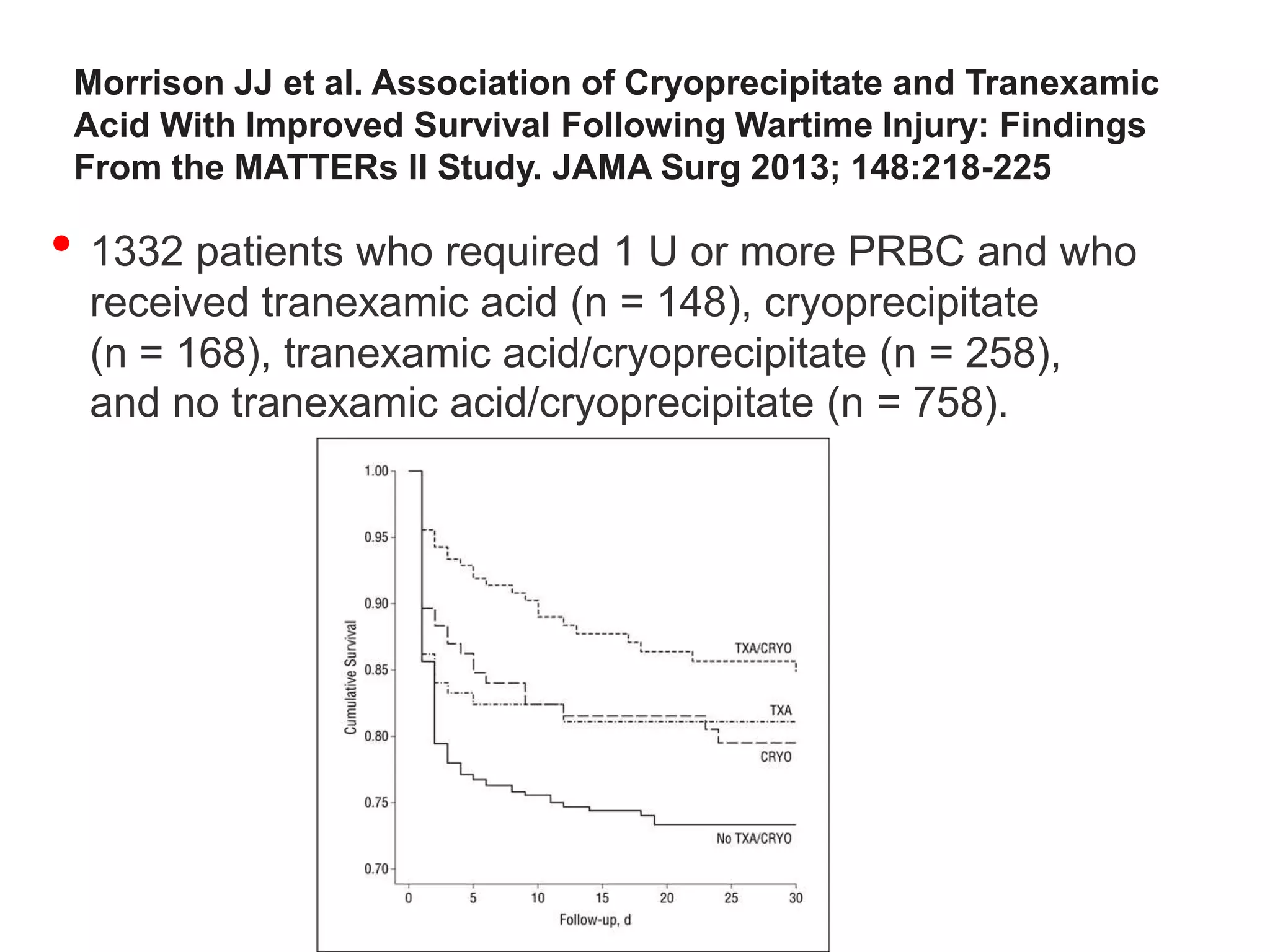
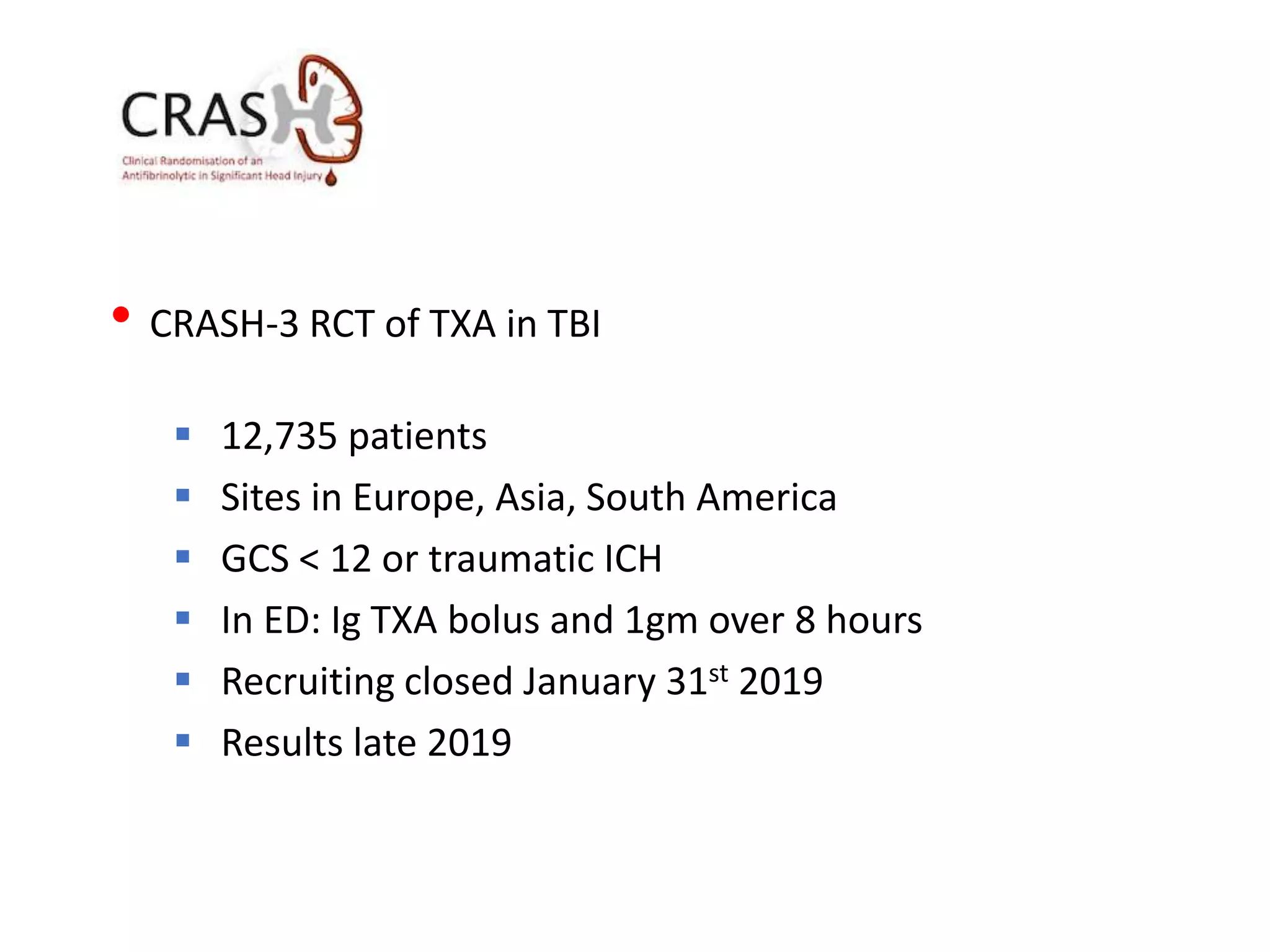
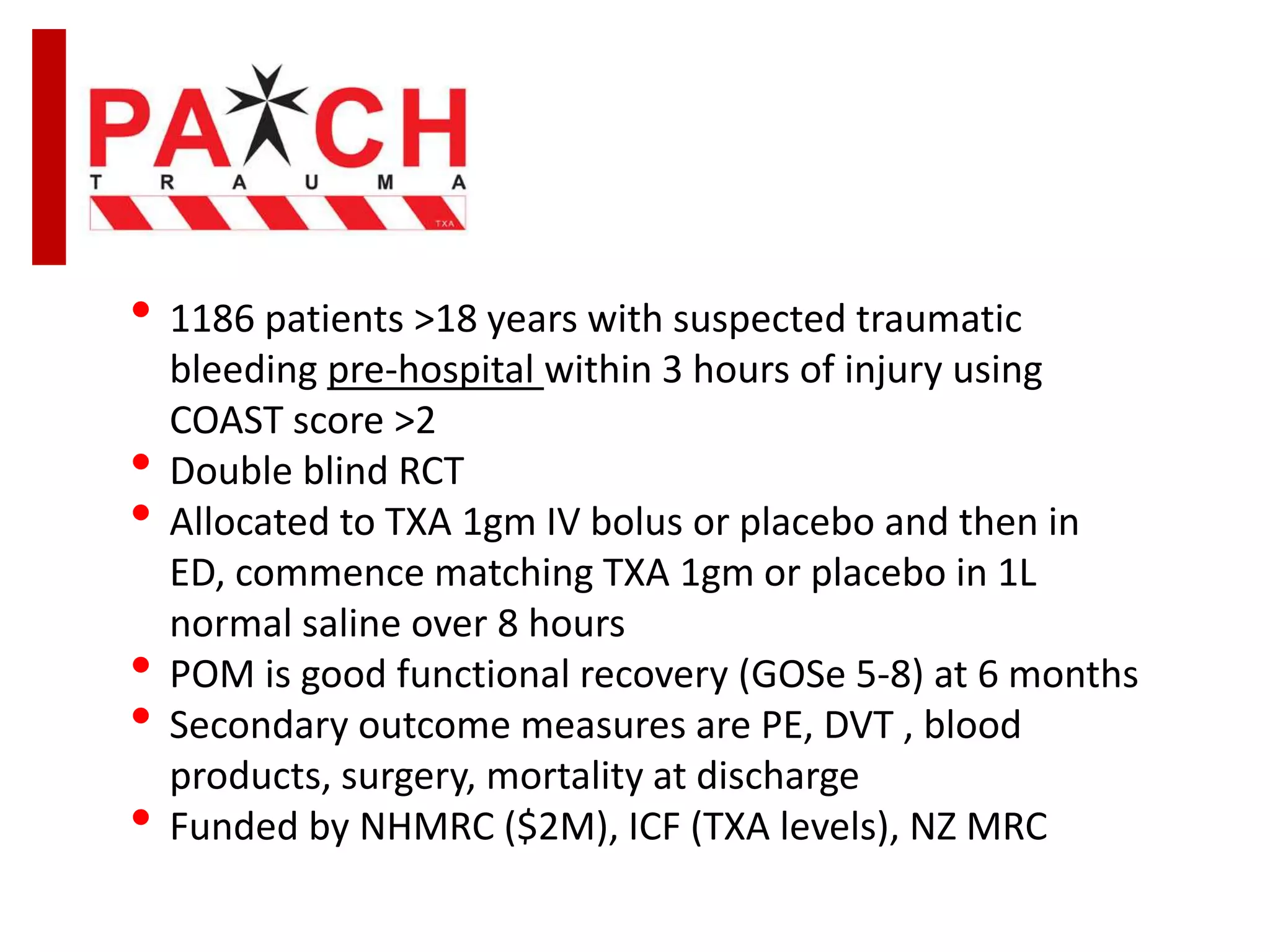
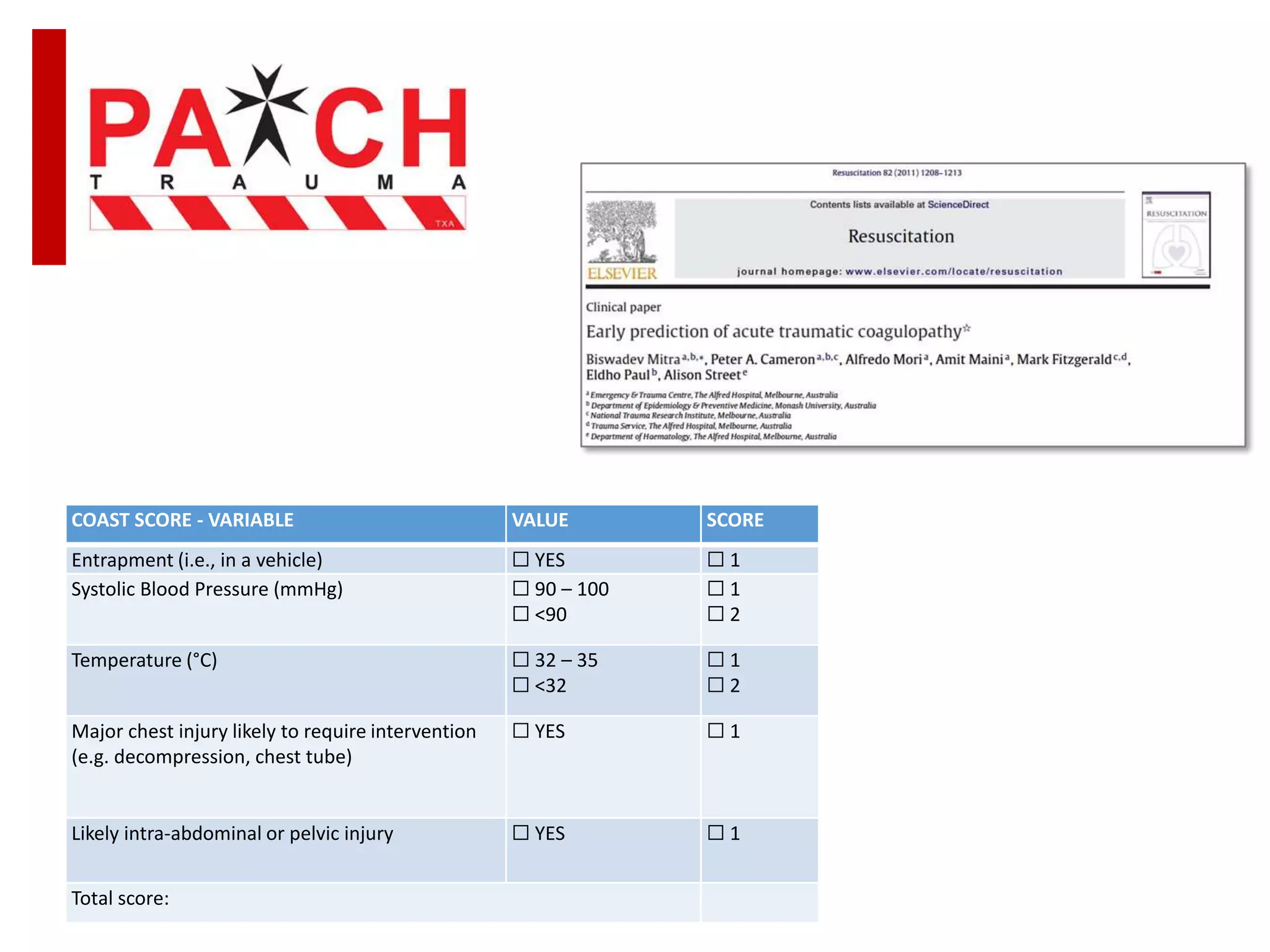
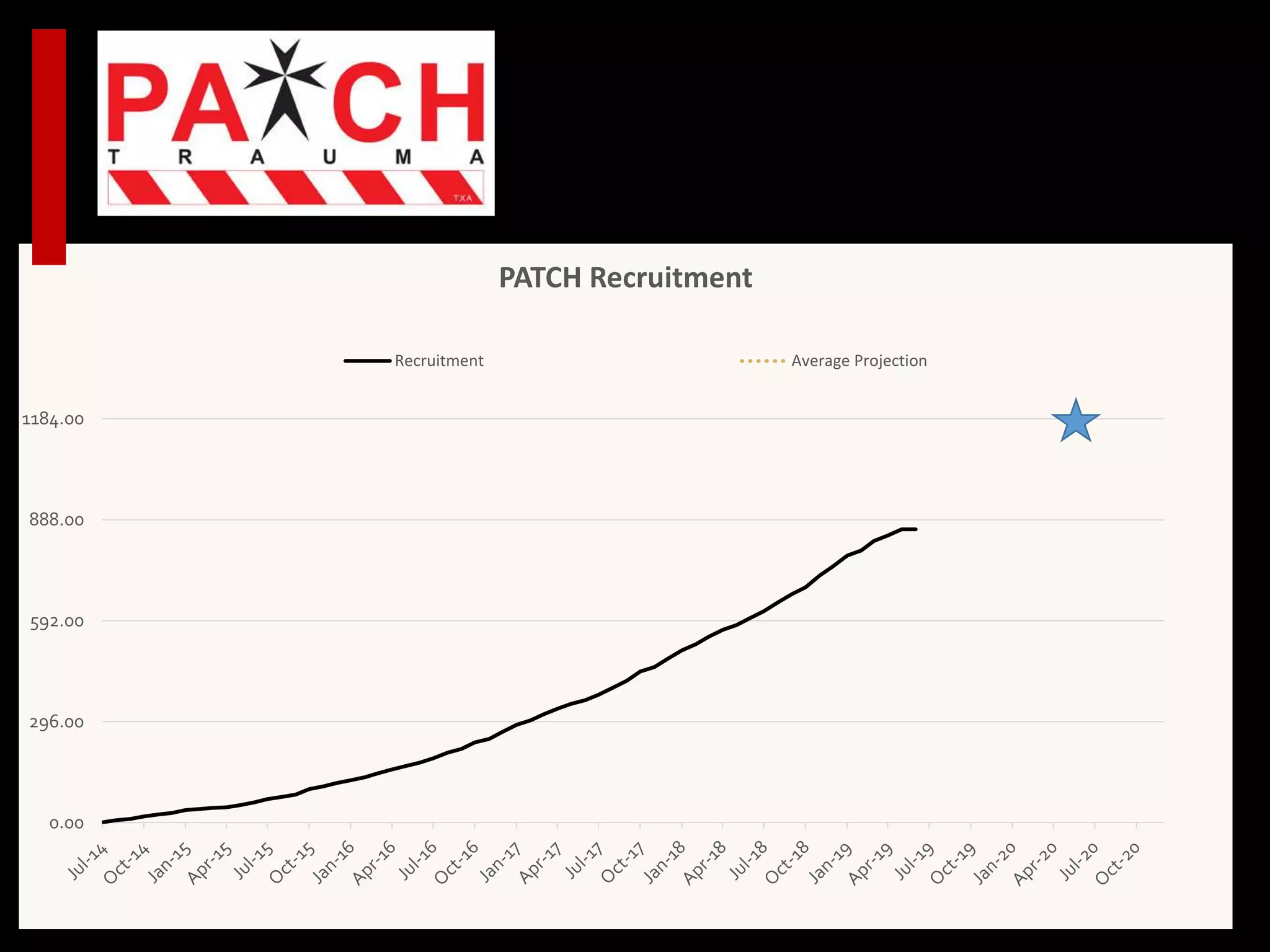
This document discusses the use of tranexamic acid (TXA) in trauma and bleeding patients. It summarizes several randomized controlled trials investigating TXA in coronary artery surgery, postpartum hemorrhage, traumatic brain injury, and trauma. It finds that TXA significantly reduces bleeding and mortality in trauma, postpartum hemorrhage, and cardiac surgery. However, TXA did not show a benefit in intracerebral hemorrhage. It also describes the ongoing PATCH trial investigating pre-hospital administration of TXA in trauma patients.