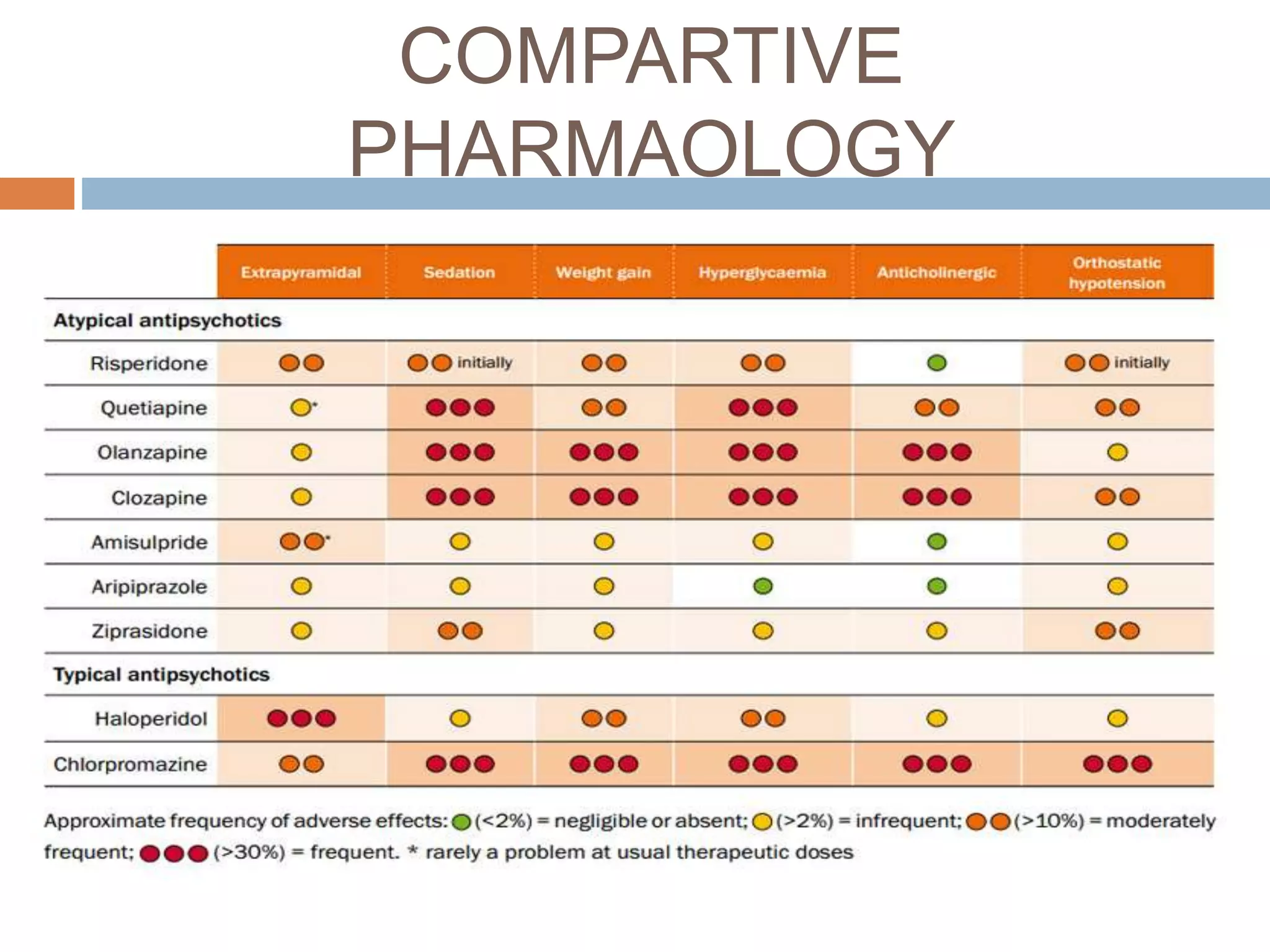
This document provides information on neuroleptic agents, including their uses, mechanisms of action, pharmacokinetics, and side effects. It discusses several classes of neuroleptics such as phenothiazines, thioxanthenes, butyrophenones, and dibenzodiazepines. Key points include:
- Neuroleptics are used to treat schizophrenia, mania, depression and other conditions by blocking dopamine receptors.
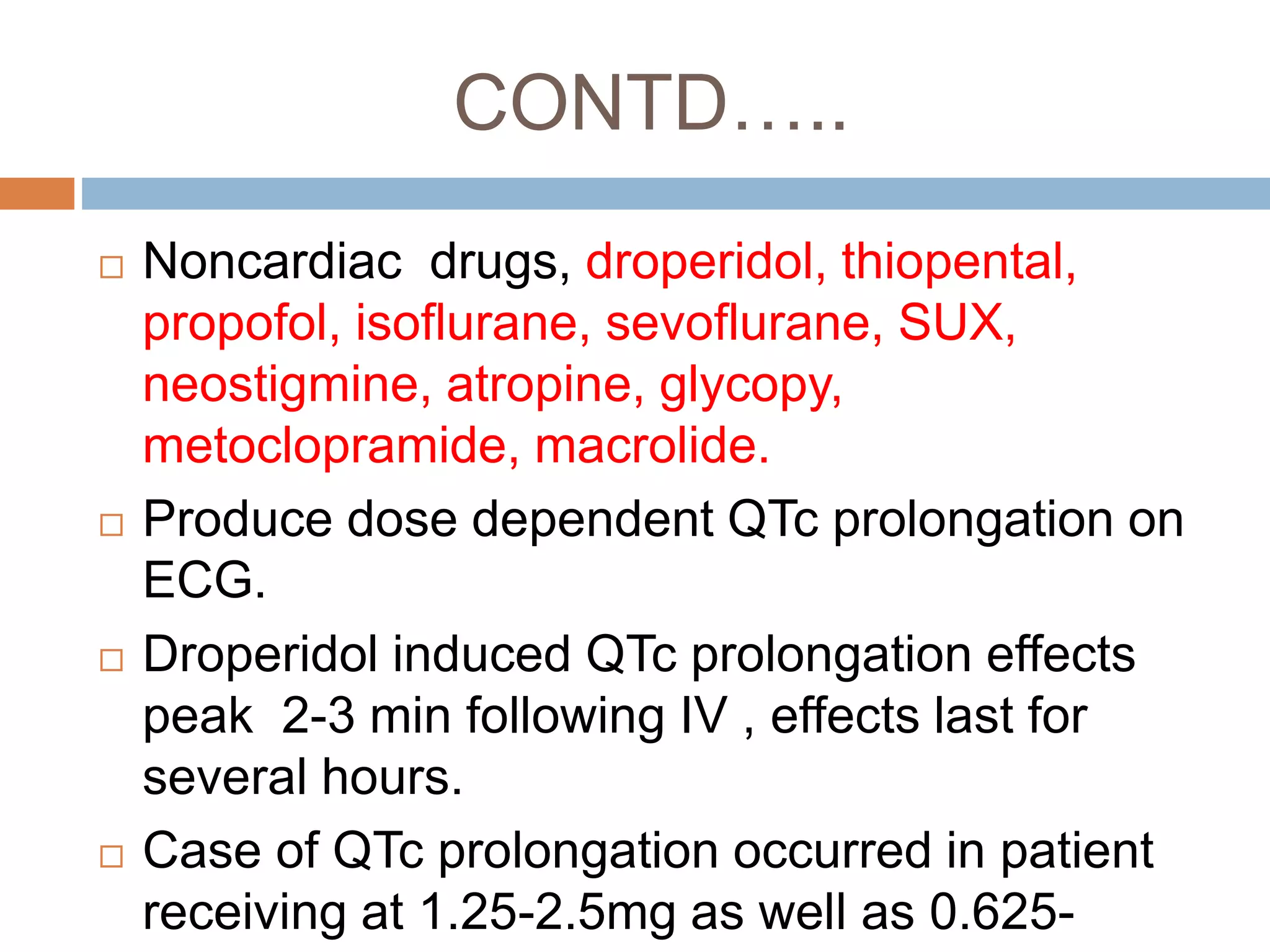
- Side effects include extrapyramidal symptoms, cardiovascular effects like hypotension, and rare but serious issues like neuroleptic malignant syndrome.
- Droperidol is commonly used as a preoperative antiemetic and for neuroleptanalgesia in