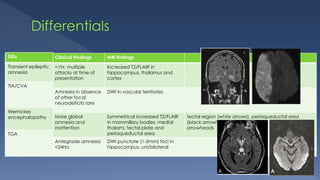
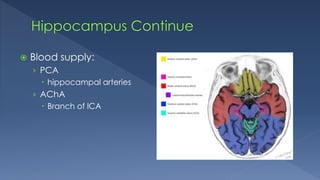
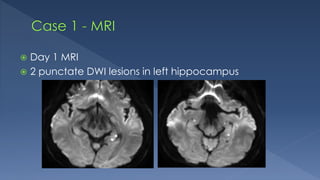
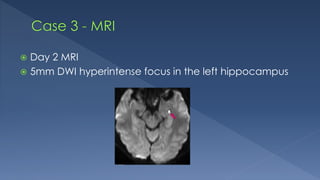
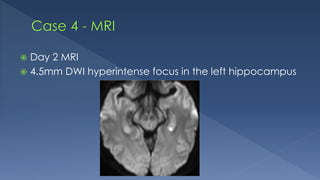
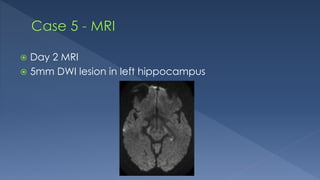
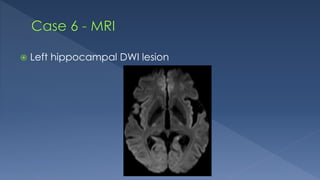
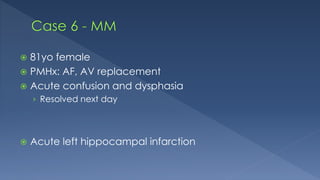
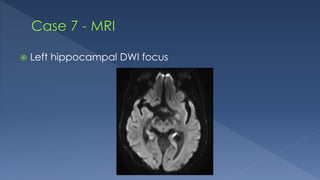
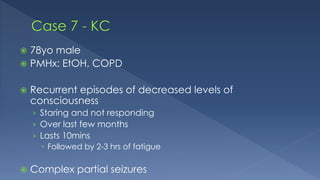
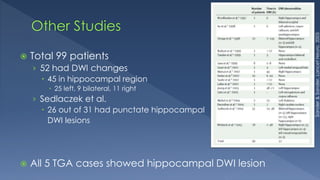
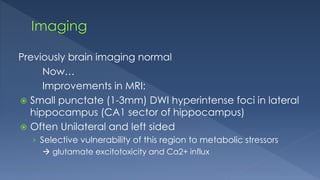
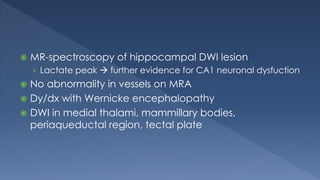
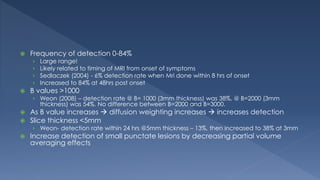
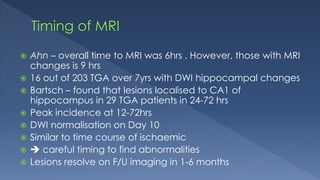
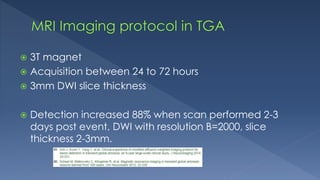
This case series from a hospital presents 5 cases of transient global amnesia (TGA) that were investigated with MRI. MRI findings of small punctate lesions in the hippocampus on diffusion-weighted imaging (DWI) supported the clinical diagnosis of TGA in all 5 cases. Previous studies have found hippocampal DWI lesions in 45-84% of TGA cases depending on timing of MRI and acquisition parameters like slice thickness and diffusion weighting. Improved MRI techniques allow for detection of subtle lesions that correlate with the pathophysiology of selective hippocampal vulnerability in TGA.