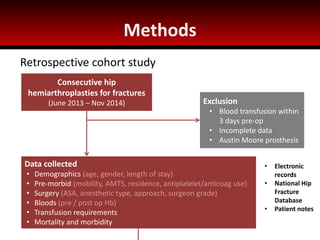
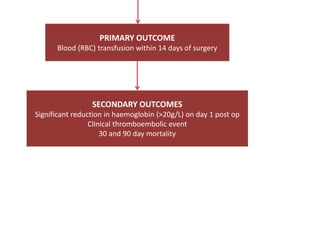
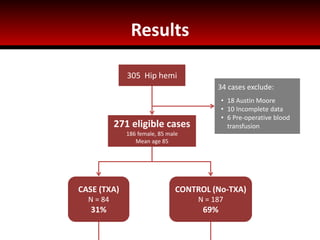
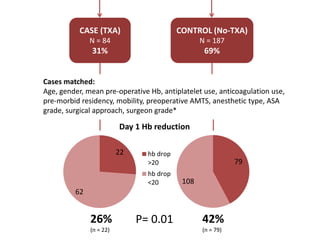
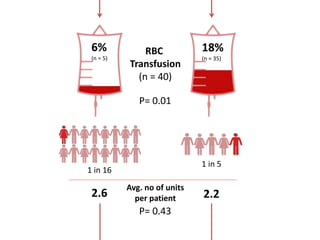
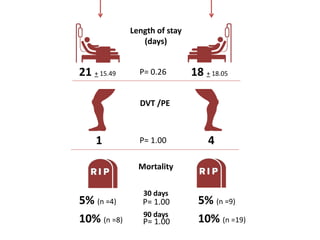
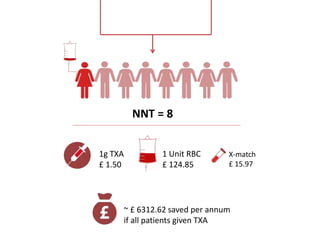
This study examined whether administering tranexamic acid (TXA) before hip hemiarthroplasty surgery reduces postoperative blood transfusions. The study reviewed 271 patient records, with 84 patients receiving TXA and 187 not receiving it. Patients receiving TXA saw a lower drop in postoperative hemoglobin levels and lower transfusion rates. Specifically, the TXA group saw a 26% transfusion rate compared to 42% in the non-TXA group. The study concluded that TXA reduces postoperative blood loss and transfusions in hip hemiarthroplasty patients, and is a safe and cost-effective intervention.
![References
1. Zufferey PJ, Miquet M, Quenet S, Martin P, Adam P, Albaladejo P, et al. Tranexamic acid in hip fracture surgery: a
randomized controlled trial. Br J Anaesth [Internet]. 2010 Jan [cited 2015 Feb 2];104(1):23–30. Available from:
http://www.ncbi.nlm.nih.gov/pubmed/19926634
2. Lawrence VA, Silverstein JH, Cornell JE, Pederson T, Noveck H, Carson JL. Higher Hb level is associated with better
early functional recovery after hip fracture repair. Transfusion [Internet]. 2003 Dec [cited 2015 Feb
2];43(12):1717–22. Available from: http://www.ncbi.nlm.nih.gov/pubmed/14641869
3. Kadar A, Chechik O, Steinberg E, Reider E, Sternheim A. Predicting the need for blood transfusion in patients with
hip fractures. Int Orthop [Internet]. 2013 Apr [cited 2015 Feb 4];37(4):693–700. Available from:
http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3609993&tool=pmcentrez&rendertype=abstract
4. Lemaire R. Strategies for blood management in orthopaedic and trauma surgery. J Bone Joint Surg Br [Internet].
2008 Sep [cited 2015 Feb 2];90(9):1128–36. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18757950
5. Poeran J, Rasul R, Suzuki S, Danninger T, Mazumdar M, Opperer M, et al. Tranexamic acid use and postoperative
outcomes in patients undergoing total hip or knee arthroplasty in the United States: retrospective analysis of
effectiveness and safety. BMJ [Internet]. 2014 Jan 12 [cited 2014 Dec 7];349(aug12_8):g4829. Available from:
http://www.bmj.com/content/349/bmj.g4829
6. Zhou X, Tao L, Li J, Wu L. Do we really need tranexamic acid in total hip arthroplasty? A meta-analysis of nineteen
randomized controlled trials. Arch Orthop Trauma Surg [Internet]. 2013 Jul [cited 2015 Jan 4];133(7):1017–27.
Available from: http://www.ncbi.nlm.nih.gov/pubmed/23615973
7. Ho KM, Ismail H. Use of intravenous tranexamic acid to reduce allogeneic blood transfusion in total hip and knee
arthroplasty: a meta-analysis. Anaesth Intensive Care [Internet]. 2003 Oct [cited 2015 Jan 29];31(5):529–37.
Available from: http://www.ncbi.nlm.nih.gov/pubmed/14601276](https://image.slidesharecdn.com/txastudy-150215150908-conversion-gate01/85/Tranexamic-acid-in-hip-hemiarthroplasty-14-320.jpg)